Topic outline
UNIT 1: SELECTED NURSING THEORIES
Key Unit Competence:
Integrate the principles of nursing theories in the current nursing practiceIntroductory activity 1
Picture:
Look at the scenario represented by the image below carefully, and attempt to
answer the asked questions.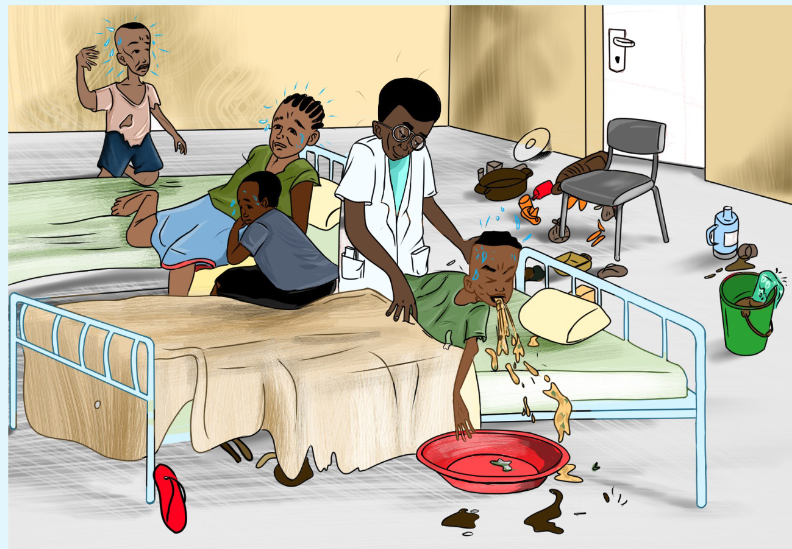
1) In which situation are the people in this Picture?
2) Which kind of issues can you find from this image?
3) Suggest what would happen when the identified issues from the image
are not solved?
4) Think about how patients were helped before modern nursing?
1.1. Historical Overview of NursingLearning activity 1.1
As you have learned in other subject, each science has its own history. Using
the following links: https://brainkart.com/article/Evolution-of-Nursing_35445/;
or using the Library books (fundamentals of nursing) search on Nursing
Evolution.Identify main periods of nursing evolution and what happened in each period
1.1.1. Concepts definition.
Different people have defined nursing in different ways. However, Nursing
is defined as a profession within the health care sector focused on the care of
individuals, families, and communities so they may attain, maintain, or recover
optimal health and quality of life. The nurse is a caregiver or someone who has
been formally trained and educated to tend to the sick and infirm.According to ICN, “Nursing encompasses autonomous and collaborative care of
individuals of all ages, families, groups and communities, sick or well and in all
settings. Nursing includes the promotion of health, prevention of illness, and the
care of ill, disabled and dying people. Advocacy, promotion of a safe environment,
research, participation in shaping health policy and in patient and health systems
management, and education are also key nursing roles.The primary responsibility
of a nurse is to provide nursing care for patients, family and community. In addition,
the nurse plays an important role that include patient advocator, teacher/educator,
leader, collaborator, caregiver, communicator, counsellor, and researcher.Patient: Is someone who is waiting for or undergoing medical treatment and care.
The word “patient” comes from a Latin word meaning “to suffer” or “to bear”.
Traditionally, the person receiving health care has been called a patient. The
connotation commonly attached to the word is one of dependenceClient: A client is a person who engages the advice or services of another who is
qualified to provide this service. The term client presents the receivers of health
care as collaborators in the care, that is, as people who are also responsible
for their own health.
Health: WHO (1947) World Health Organization– definition of health
“a state of complete physical, mental, spiritual and social well- being, not merely
the absence of disease or infirmity”Illness: is referred as the condition in which an individual functions at optimal levels.
It means engaging in attitudes and behavior that enhance the quality of life and
maximize personal potential.Health-illness continuum: Wellness is a dynamic process that is ever
changinCaring: includes assistive, supportive and facilitative acts toward or for
another individual or group with evident or anticipated needs. Caring serves to
ameliorate or to improve human conditions or life ways. Caring is essential to
human development, growth and survival.Caring: includes assistive, supportive and facilitative acts toward or for another
individual or group with evident or anticipated needs. Caring serves to
ameliorate or to improve human conditions or life ways. Caring is essential to
human development, growth and survival.1.1.2. Evolution of nursing
In the times before nursing became an official profession, patient care was
commonly provided to sick people by family, friends, clansmen, or fellow tribe
members. Nursing began as a helping profession, often undertaken by nuns and
military personnel during wartime. Until recent history, nursing was considered
a woman’s profession. Although the origins of nursing predate the mid-19th
century, the history of professional nursing traditionally begins with Florence
Nightingale. The nursing profession has a rich history that spans centuries of
evolving health care for patients, families, and communities. At present, the World
Health Organization (WHO) considers nurses as the backbone of the health care
industry. However, nursing had to undergo a long period of development before
it became the occupation, we are now familiar with. Evolution of nursing can be
divided into three periods of time in history, Early Christian age, Middle age, and
the dawn of modern Nursing.a) Early Christian age
Health care started to become more organized during the early Christian age.
Christianity believed that one should render services of love to humanity without
any reward. It was equal to one’s sincere love to gods. The temples were more
like health spas rather than hospitals in religious institutions governed by priests
and nursing was done by women in temples or home. The caregivers had no
formal training in therapeutic modalities and volunteered their time to nurse the sick.
Deaconesses’ women, with some educational background, were assigned by the
church to take care of ill persons. The Deaconess Phoebe is considered by some
historians to be the first “visiting nurse” because of the home care services she
offered around A.D. 50. This principle was integrated later in nursing and helped to
improve the status of nursing.b) Middle age
Monks and nuns devoted their life to the care and services of the poor and sick.
During the middle age, hospitals in large Byzantine cities were staffed primarily by
paid male assistants and male nurses. These hospitals were established primarily
as charity houses, medical practices in Western Europe remained basically
unchanged until the 11th and 12th centuries, when formal medical education for
physicians was required in a university setting and nursing become differentiated
from medicine and surgery. Although there were not enough physicians to care for
all the sick, other care-givers were not required to receive any formal training. The
dominant caregivers in the Byzantine setting were men; however, this was not true
in the rural parts of the Eastern Roman Empire and in the West. In these societies,
nursing was viewed as a natural nurturing job for women.When taking a sight at nursing in the Middle Ages, there were numerous
advancements and innovations that were implemented within the nursing industry
during these years, helping to form some of the roots of modern nursing. Hospitals
functioned in innumerable ways, housing lepers and refugees among the typical
sick and injured patients. It was due to this that a nurse’s role within the hospital
involved a wider range of duties than may be seen today.c) Modern Nursing:
The dawn of modern Nursing is a very different field than it was before the world
wars, and even before the Crimean War. The history of modern nursing originates
from the pioneering work of Florence Nightingale. Through innovative nursing care
and influence, Nightingale laid the foundation for nursing as an official profession.
Nightingale, who belonged to a wealthy British family, chose not to lead the leisurely
life of a typical upper-class lady during the Victorian era. Instead, she devoted her life
to providing nursing services to sick persons, even if it was not considered a proper
occupation for women in her social class during that period. Miss. Nightingale was
the first to mention Holism (Treating the whole patient) in Nursing. Nightingale was
the founder of modern nursing. In 1860, Nightingale also opened the first nursing
school, called the Nightingale School for Nurses, which began to regulate how
nurses learned and practiced. Not only did this ensure nurses had an educational
foundation of knowledge and techniques, but it helped ensure a standard of care
for patients, as well.Because of the work Nightingale did for modern nursing, the oath taken by nurses
when they graduate is called the “Nightingale Pledge.” The field of health care is
also more diversified, so nurses can choose what area they would like to practice,
and tailor their education to that field. A nurse may choose paediatrics, emergency,
hospice, cardiology, or a number of other areas, and focus his or her efforts on
the care of patients in that area. In the modern nursing field, nurses have a higher
reputation, as well. They are no longer seen as simply assistants to physicians
who do the things physicians won’t do. Instead, nursing is a strong field of its own,
and nurses have a wide range of duties and responsibilities. Nurses earn respect
for themselves among health care professionals because of the education and
experience required to be a nurse.In Rwanda, training of nurses began during the colonial era, many of the nursing
schools were opened by religious institutions such as Catholics, Protestants
and Adventists, some being public and private. During 1980s, education was
restructured and the secondary program was fixed to 6 years; the nursing program
was integrated in secondary education. In 1994, the Genocide against the Tutsi
has seriously affected all sectors of life especially nursing. After the 1994 Genocide
against the Tutsi, the Government of Rwandan invested in training nurses at various
levels, and many public and private nursing and midwifery schools were opened.
Today, with the support from the Government of Rwanda, Nursing and Midwifery
professions are becoming a pillar and cornerstone of Rwandan Health system.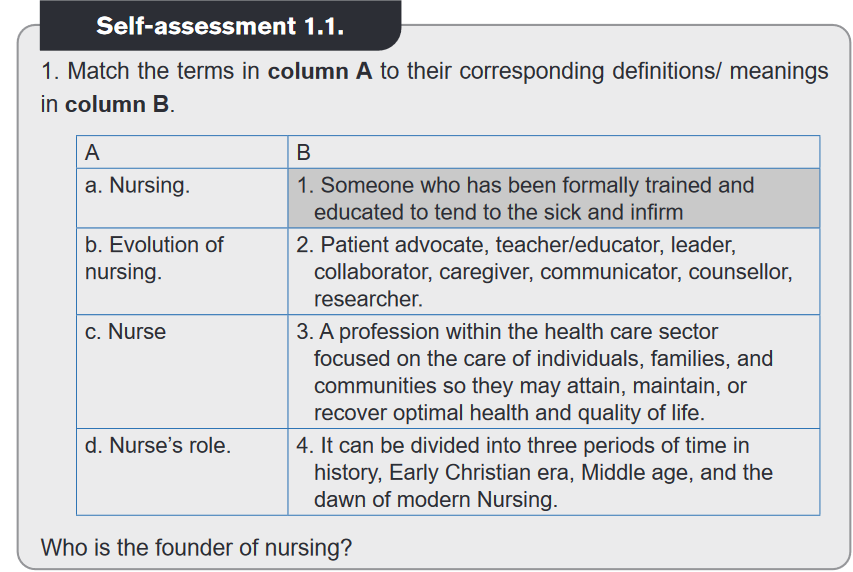
A: With a crush car in accident where there are two survived person (Mrs M and Mrs
T),
B: the survived persons moved to the hospital, both Mrs M and Mrs T is transported
on stretcher,
C: Mrs M was well cared for by a nurse removing dirty clothes, washing her, moving
her from stretch to well make bed
D: There a doctor examining the Mrs M (greetings, ask what happen, how is she
feeling, where she has pain, the patient reply that nothing is ok she feel pain
everywhere, the doctor reassures the patients “do not worry you are in good hand
everything will be ok, let us do x-ray investigation to see if there is no fracture.
E: Mrs T sitting in the wheelchair, with many lacerations on both arms and one leg,
being drowsy, no body care about her.Observe the images and answer the following questions
Between the two persons, which one have received good care and why?
1.2.1. Definition of nursing Theory
Nursing theory is “an organized framework of concepts and purposes designed
to guide the practice of nursing”. It expresses the values and beliefs of nursing
discipline, creating a structure to organize knowledge and illuminate nursing
practice. Nursing theories help us to describe, explain, or predict caring practices.
Briefly nursing theory give us directions of how-to best care for our patients. The first
nursing theories appeared in the late 1800s when a strong emphasis was placed on
nursing education. Nursing theories are developed to explain and describe nursing
care, guide nursing practice and provide a foundation for clinical decision making.
Examples: During care to any patient, you must ensure that the patient has good
hygiene, his surroundings are clean, has fresh air in room, room is warm, has
light, and patient has taken food. This instruction/framework requesting the good
environment of the patient is an example of Theory. The nursing theory to be used
in caring the patients in mental health services will not be the same as the one to
be used in Emergence service1.2.2. Purpose of nursing theories
They provide a foundational knowledge of care concepts that enable those in the
profession to explain what they do for patients and the reasons for their actions.
It helps nurse’s articulate evidence that justifies the methodologies behind their
practice.Self-assessment 1.2.
Answer these questions
1) What do you understand by the term ‘’Nursing theory?
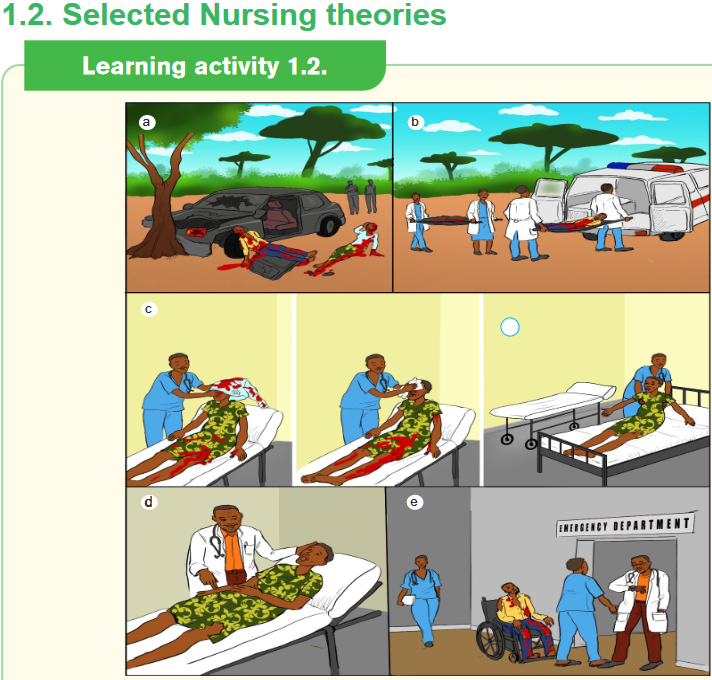
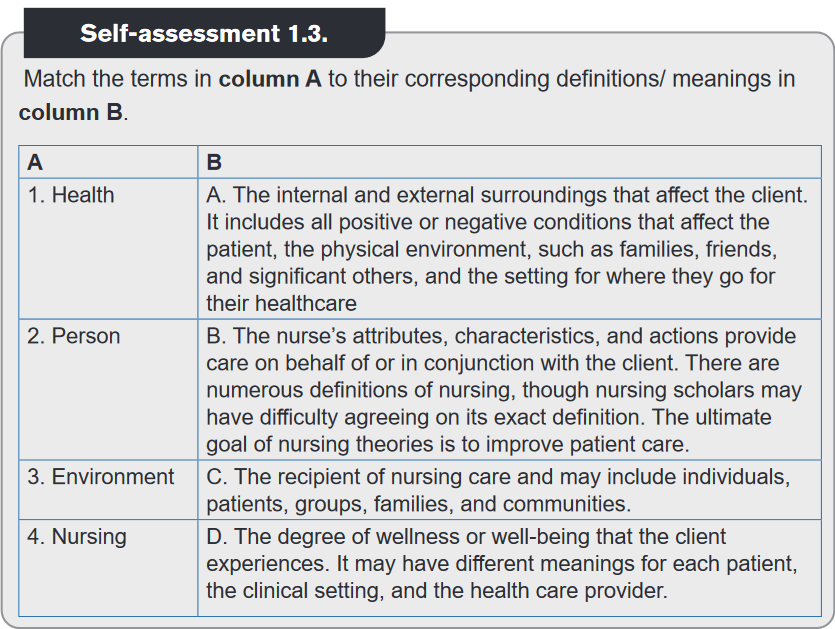
2) Do you think nursing theories are important? Justify your answer.1.3. Major Concepts of Nursing Theory
Learning activity 1.3.
Rwanda as a developing country is building strongly health sector for wellbeing
of its population as it is its precious resources, as an associated nurse your
contribution will require to understand the set of ideas or concepts that provide
the structure for how nursing discipline should function. Read the Page 40
in the book “Kozier and ERB’s Fundamental of nursing concepts, process
and practice fourth Australian Edition”; on “Metaparadigm for nursing” and
in three to four sentences, summarize what you have read in the book.1.3.1. Concept of nursing theory.
A concept, is like ideas, are abstract impressions organized into symbols of reality.
It describes objects, properties, events and relationships among them. Nursing
concept is a fundamental nursing perception also called the metaparadigms of
nursing. They provide the framework for understanding nursing practice.1.3.2. Element of Concepts of Nursing Theory
There are four major concepts of nursing theory which are frequently interrelated
and fundamental to nursing theory: person, environment, health, and nursing.
They are collectively referred to a metaparadigm for nursing.a) Person
Is referred to Client or Human Beings. Person is the recipient of nursing care and
may include individuals, patients, groups, families, and communities.b) Health
The degree of wellness or wellbeing that the person experiences. It may have
different meanings for each patient, the clinical setting, and the health care provider.c) Nursing
The nurse’s attributes, characteristics, and actions provide care on behalf of or
in conjunction with the client. There are numerous definitions of nursing, though
nursing scholars may have difficulty agreeing on its exact definition.d) Environment:
Environment is defined as the internal and external surroundings that affect the
client. It includes all positive or negative conditions that affect the patient, the
physical environment, such as families, friends, and significant others, and the
setting for where they go for their healthcare.
1.4. Selected Nursing theorists
1.4.1. Florence NightingaleLearning activity 1.4.1.
Observe the images below and respond to the questions that follow:
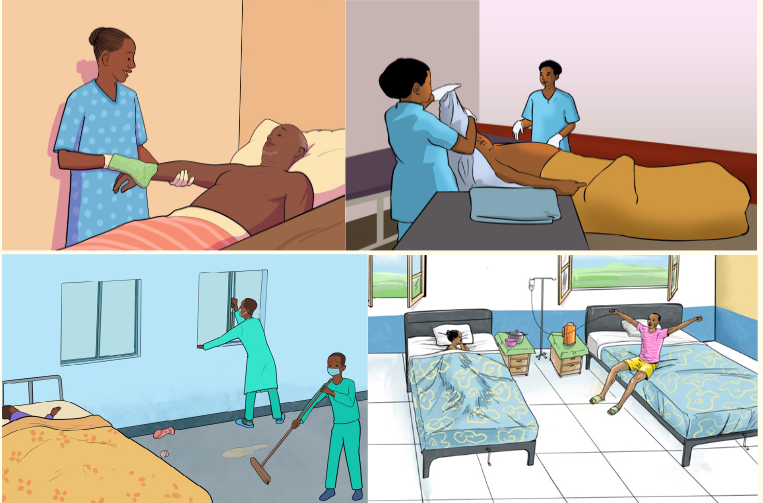
1) Observe the first three images and describe activities that are being
done,
2) What do you think would happen if these activities are not performed?
Florence Nightingale, “the mother of modern nursing”. Florence Nightingale
(1820-1910) was a British nurse, best known as the founder of modern nursing and
“The Lady with the Lamp” because she would visit soldiers at night with a small
lantern in her hand. Her experiences as a nurse during the Crimean War were
foundational in her views about sanitation. Florence Nightingale is the first nurse
theorist well known for developing the environmental theory. Her theory focused on
the environment. She linked health with five environmental factors.In Florence Nightingale’s Environmental Theory, she identified five (5) environmental
factors: fresh air, pure water, efficient drainage, cleanliness or sanitation, and light
or direct sunlight.a) Pure fresh air
“To keep the air he breathes as pure as the external air without chilling him.”b) Pure water
“Well water of a very impure kind is used for domestic purposes. And when
the epidemic disease shows itself, persons using such water are almost sure to
suffer.”c) Effective drainage
“All the while the sewer may be nothing but a laboratory from which epidemic disease
and ill health are being installed into the house.”d) Cleanliness
“The greater part of nursing consists in preserving cleanliness.”e) Light (especially direct sunlight)
“The usefulness of light in treating disease is very important.Deficiencies in these five factors produced lack of health or illness.
In addition to the above factors, Nightingale also stressed the importance of
keeping the patient warm, maintaining a noise-free environment, and attending to
the patient’s diet in terms of assessing intake, timeliness of the food, and its effect
on the person. Her general concepts about ventilation, cleanliness, quiet, warmth,
and diet remain integral parts of nursing and health care today. “To facilitate “the
body’s reparative processes” by manipulating client’s environment”External influences can prevent, suppress or contribute to disease or death
– Nightingale’s concepts• Person/ client
– Patient who is acted on by nurse
– The recipient of nursing care
– Affected by environment
– Has vital reparative powers to deal with disease• Environment
– The major concepts for health are ventilation, warmth, light, diet,
cleanliness, and absence of noise. Although the environment has social,
emotional, and physical aspects, Nightingale emphasized the physical
aspects.
– Internal and external environment were both important to the progress of
the patient’s health.
– The importance of fresh air and ventilation and an environment free of
odors and waste, she knew that properly prepared food and clean water
were also necessary.• Health
– Being well and using one’s powers to the fullest extent.
– Maintaining well-being by using a person’s powers
– Nightingale saw health as an absence of disease
– Health is maintained through prevention of disease via environmental
health factors. Maintained by control of environment and taking care of
the body, health was achieved.• Nursing
– Provision of optimal conditions to enhance the person’s reparative
processes and prevent the reparative process from being interrupted.
– Provided fresh air, warmth, cleanliness, good diet, quiet to facilitate
person’s reparative process
– Facilitates a patient’s reparative process by ensuring the best possible
environment
– Influences the environment to affect healthFlorence Nightingale (1860) defined nursing as: “the act of utilizing the
environment of the patient to assist him in his recovery. Nightingale considered a
clean, well-ventilated, and quiet environment essential for recovery. What nursing
has to do is to put the patient in the best condition for nature to act upon him.
Application of Florence Nightingale theory in nursing education and practice:
The environmental theory of Florence Nightingale is the basis of nursing practice
today. Nurses use the environmental aspects of Nightingale’s theory (ventilation,
warmth, quiet, diet, and cleanliness) in their daily practice to care for patients with
different conditions to assist them in recovery. In addition, Nightingale’s principles
of nurse training provided a universal template for early nurse training schools and
is still evident in today’s nursing programs across the world.Self-assessment 1.4.1.
Read this cases study and criticize according to nightingale theory.
1) In hospital X, where Miss MUKAMANA, associated nurse went for
clinical placement; there was a very small general ward, overcrowded
by patients, with closed windows and small open door in corner. There
were also 3nurses, 4 students; the patient’s belongings were on floor
under bed. With Miss MUKAMANA’s observations, she saw one nurse
feeding the patient A, Nurse MAHORO together with nurse KANYANA
after doing patient B wound dressing and administrating painkiller they
moved him outside for Sunlight exposure as the patients was recovering
and prepared to be discharged. Miss MUKAMANA was very surprise to
see nurses doing all these interventions and her supervisor told her
that it is very good, “Nurses have to care for and respond to all patient’s
Needs.2) Florence Nightingale was known as
a) Nurse who changed nursing forever.
b) Nurse responsible for the end of Crimean war.
c) Lady with the lamp.
d) Mother of nursing.
e) c & d3) The Theory of Florence nightingale focus on the clean environment.
State environmental factors it focused on.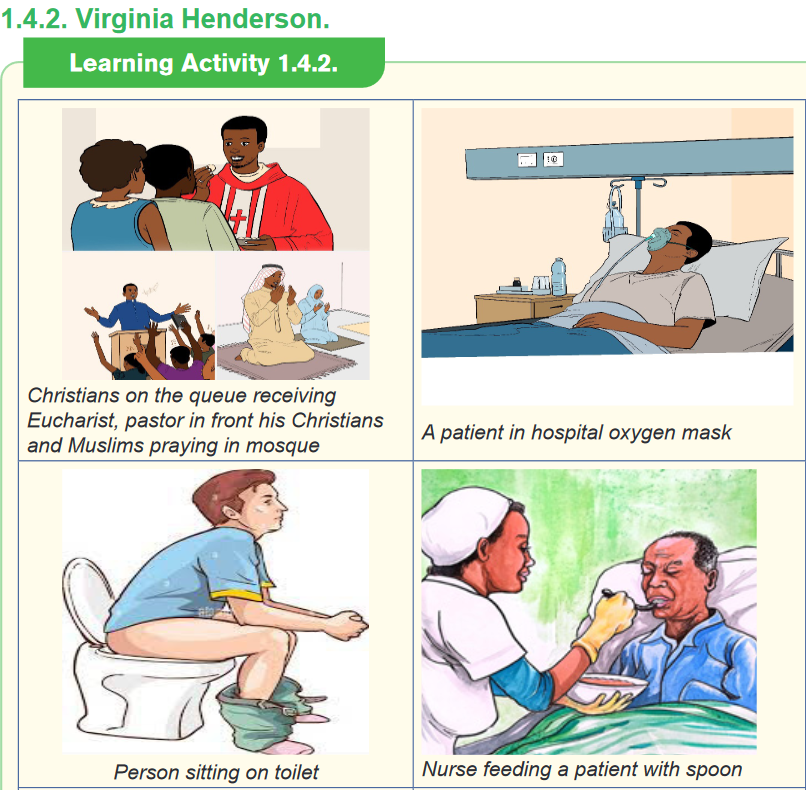
) Observe the different boxes of images and describe how you see the
personnel on the images.
2) Do you think what you have observed are important in our life? Justify
your answer.
Virginia Avenel Henderson (November 30, 1897 – March 19, 1996) was a
nurse, theorist, and author known for her Need Theory. According to Henderson,
individuals have basic needs that are components of health. Virginia Henderson
consider Person, health, nursing and environmental as:
– Person:Individual have basic needs that are component of health and require
assisstance to achieve health and independence or a peacefuldeath– Heath :Balance in all aspect of human life.
– Nursing: Unique function of the nurse is to assist the individual, sick or well,
in the perfomance of those activities contributing to health or or its recovery
that he would perfome unaided , if he has the necessary strenght , will or
knowledge.In such way as to help him to gain independence as rapid as
possible.– Environment: Maintaining a supportive environment conductive for health.
The 14 components of Virginia Henderson need theory show a holistic nursing
approach covering the physiological, psychological, spiritual, and social needs.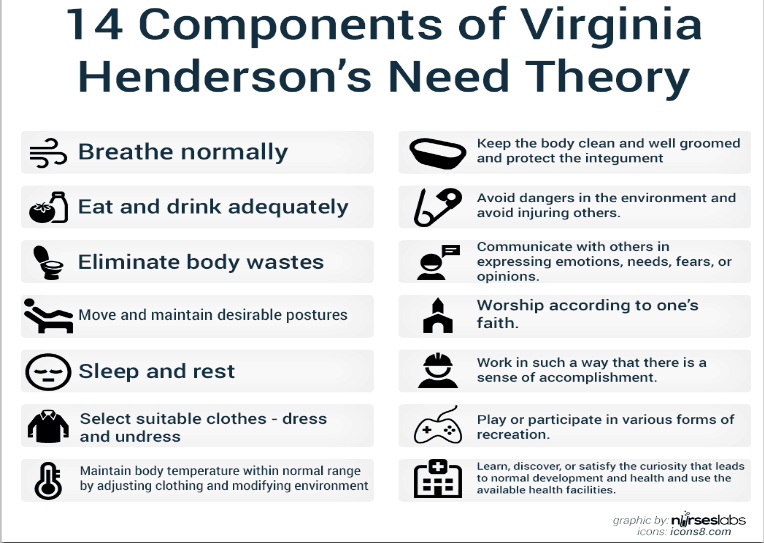
Application of Virginia Henderson theory in nursing education and practice:
Today the nurses use Henderson’s needs theory in their routine practice to set
patient’s goals based on 14 components of Henderson ‘s theory. To utilize this in
the nursing practice, the nurse would see whether the client has all of these basic
needs. If not, then, a problem exists. The nursing diagnosis must be then formulated
and the nurse must assist the client to meet all these 14 fundamental needs.Henderson’s Needs Theory is used in different nursing schools to help the students
learning how to assess the basic needs of a patient, understanding the significance
of theory and determine the situation in which it can be used to assist the patients
regaining independence.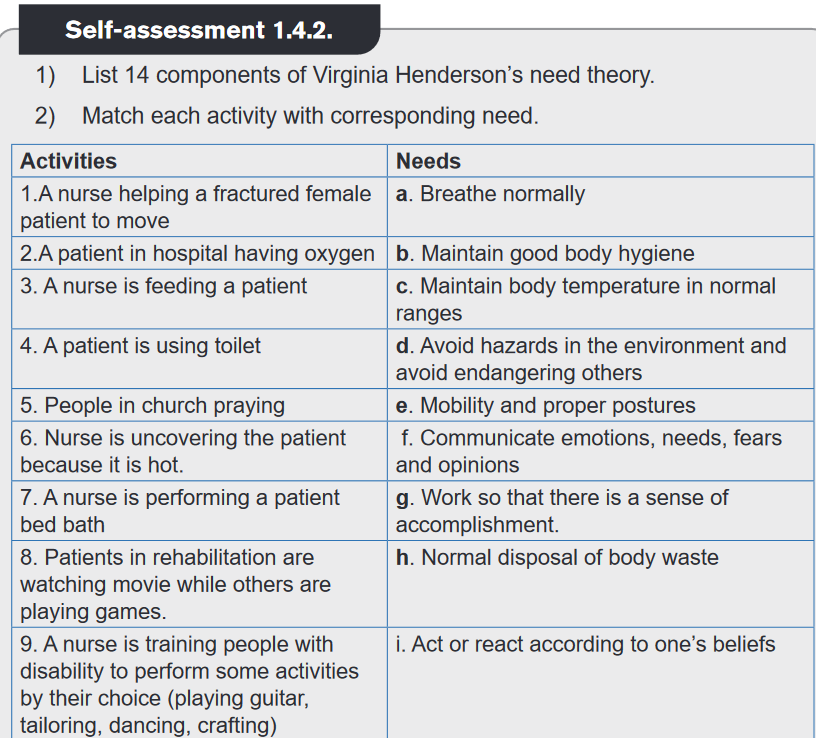
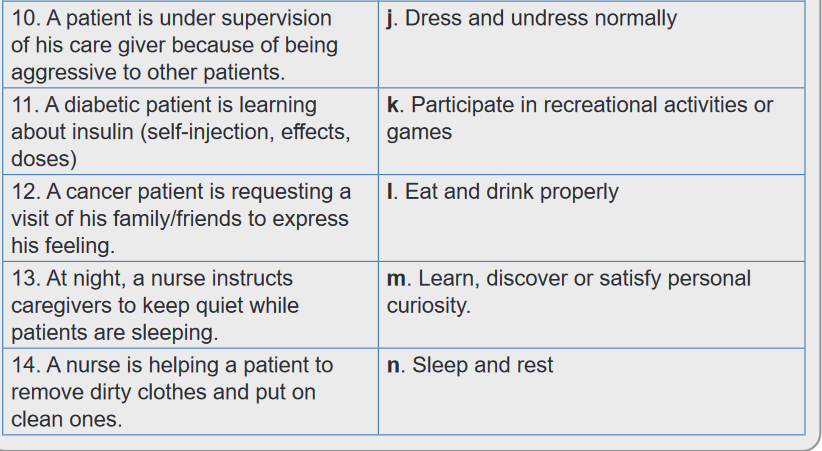
1.4.3. Hildegard Peplau
Learning Activity 1.4.3.
1) Follow the nurse-patient conversation between patient KARAKE (Mr. K)
and nurse UWIMANA and respond to these questions.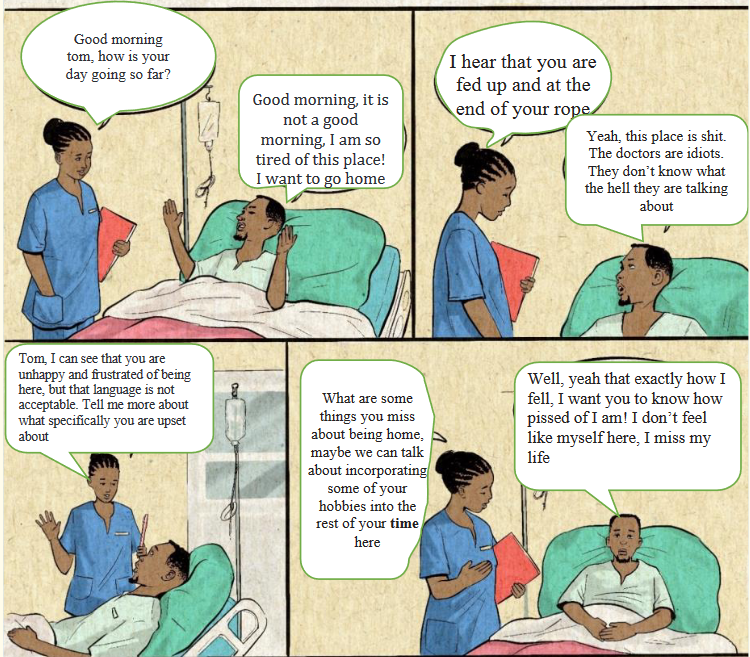
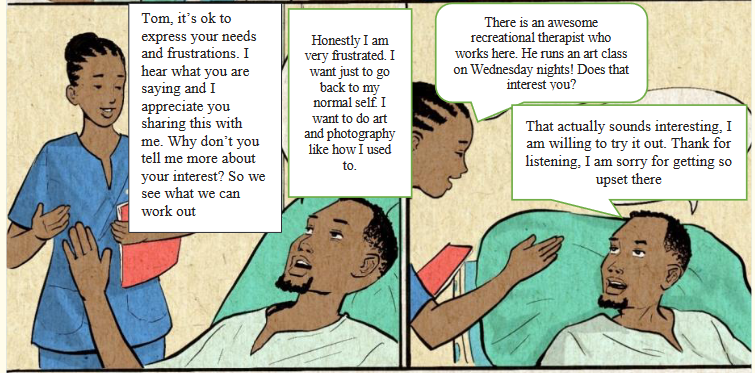
a) In which emotional status is patient Tom Karake?
b) Why patients Tom Karake feels unhappy?
c) What is Nurse UWIMANA doing?
d) How nurse UWIMANA arrived to calm down KARAKE?
e) How the conversation ended up?
2) Do you think it is good to have someone who could understand you?
Explain your answer.
Hildegard Elizabeth Peplau (September 1, 1909 – March 17, 1999) was an American
nurse. She became the first publisher of nursing theory since Florence Nightingale.
Hildegard Peplau’s interpersonal relations theory emphasized the nurse –client
relationship as the foundation of nursing practice. Peplau frequently acknowledged
the importance of patients’ experiences of nursing care. Peplau’s theoretical work on
the nurse patient relationship continues to be essential to nursing practice. Peplau
developed the four levels of anxiety (mild, moderate, severe, and panic levels) that
are the standards nurses use in assessing anxiety. Peplau believed that nurses
play an important role in helping clients reduce their anxiety and in converting it
into constructive action. Large institutions are educating their workforce on the
importance of having a relationship, a connection with those with whom the nurse
interacts and to whom he or she provides care. How Peplau’s theory view person,
health, nursing and environmental?• Person: An organism that strives in its own way to reduce tension generated
by needs or organism that lives in an unstable balance of a given system.• Health: symbolizes movement of the personality and other ongoing human
Fundamental of Nursing | Associate Nursing Program | Senior 4 21
processes that directs the person towards creative, constructive, productive
and community living.
• Nursing is defined as an interpersonal, therapeutic process that takes place
when professionals, specifically educated to be nurses, engage to recognize
and respond to people who are in need of health services though therapeutic
relationships cooperatively
• Environmental: Peplau does not directly address society environment, she
encourages the nurse to consider the patient’s culture and mores when the
patient adjusts to hospital routine. Forces outside the organism and in the
context of the socially –approved way of living, from which vital human social
process are derived such as norms, customs and believedApplication of Hildegard Peplau theory in nursing education and practice:
Peplau came out with four levels of anxiety (mild, moderate, severe and panic levels).
These levels are used by nurses as standards in the anxiety assessment. Peplau
trusted that nurses have a major role in assisting clients minimize their anxiety
and transform it into productive deed. Peplau’s theory continues to be necessary
in nursing practice particularly on the nurse-patient relationship. Nursing schools,
hospitals are educating their students/workers the necessity of relationship; how
important it is to interact with those that they provide care.Self-assessment 1.4.3.
Answer the following questions:
1) Which of the following best describe Peplau’s theory?
a) Putting patients’ needs ahead of your own
b) Providing excellent clinical skills to improve patient’s health status
c) Use excellent interpersonal skills to help patients improve their
health status
d) Self-protection though avoidance of a relationship with the patient2) Peplau viewed nursing intervention as those that:
a) Support the implementation of doctor orders.
b) Direct the wants and desires of the patients
c) Are soundly based on nurse knowledge?
d) Assist patients in gaining interpersonal and intellectual competencies
grown through the nurse –patient relationship.1.4.4. Dorothea Orem
Learning Activity 1.4.4.
1) Observe the images below and list the activities observed on each image.
2) When observing those images who do you think maybe in need of such
kind of care provided as mentioned by the images?
Dorothea Elizabeth Orem (June 15, 1914 – June 22, 2007), born in Baltimore,
Maryland, was a nursing theorist and creator of the self-care deficit nursing
theory, also known as the Orem model of nursing. The theory of self-care, which
focuses on the performance or practice of activities that individuals perform on
their own behalf. Those might be actions to maintain one’s life and life functioning,
develop oneself or correct a health deviation or condition. Orem’s theory provides
a comprehensive basis for nursing practice. It has utility for professional nursing
in the areas of nursing practice, nursing education, and administration. A nurse
assists the patient or family in self-care matters to identify and describe health and
health-related results. Collecting evidence in evaluating results achieved against
results specified in the nursing system design.Theorist Orem Dorothea define Person, Health, Nursing, and environmental as
follow:
• Person: Humans (Men, Women and children) cared for either singly or as
social units and are the of nurses and others who provide direct care• Health: is being structurally and functionally whole or sound.
• Nursing: is an art thought which the practitioner of nursing gives specialized
assistance to persons with disabilities or incapability which makes more than
ordinary assistance necessary to meet needs for self-care.• Environmental: The environment as physical, chemical and biological
features, it includes the family, culture, and community.Application of Dorothea Orem theory in nursing education and practice:
Orem’s theory gives a complete foundation for nursing practice. It has useful
information in nursing practice, education and administration. A nurse helps the
patient or family members in self-care to know and express health and health
related results. Students nurse are educated Orem’s theory to integrate it in their
daily practice during clinical practice. It helps in evaluating the goals set.Self-assessment 1.4.4.
1) Which of the following theories was developed by Dorothea Orem?
a) Developed the self-care deficit theory, which explains what nursing
care is required when people cannot care for themselves
b) Developed the adaptation model, inspired by the strength and
resiliency of children; relates to the choices people make as they
adapt to illness and wellness
c) Developed the caring theory, which focuses on nursing as an
interpersonal process
d) Developed the culture care diversity and universality theory2) Respond by TRUE or FALSE to the following statement
According to Dorothea Orem, Self-care refers to the practice of activities
that individuals initiate and perform on their own behalf in maintaining
life, health and well-being.1.4.5. Jean Watson
Learning activity 1.4.5.
Read careful the following scenario showing jean Watson theory and respond
to the questions.KALISA, a 39-year-old truck driver is admitted to the hospital following an accident
which caused the burn on front of his chest, is feeling much pain, appears very
tense with tears in his eyes, and was rushed immediately to the hospital. The nurse
at the hospital received him, holding his hands, with a soft voice, have a seat,
you are so nervous, feeling too much pain, what happened to you?’’ I am ready
to listen to you,’’. KALISA responded that he got an accident which caused him
to get burned. The nurse in caring voice, oh my God, let me do my best to make
you more comfortably and I am hopeful that you’ll feel better. The nurse started
giving him painkillers, antibiotics, and a rapid infusion of lactated ringers. After one
hour, KALISA started feeling better, very happy, laughing and thank the nurse for his
interest and support.’’ I felt lost’’ stated KALISA. Now I know that somebody is beside
me and has comforted me.
1) How Mr KALISA was helped by the Nurse?
2) What do you think have helped Mr KALISA to feel better and happy?
Jean Watson (June 10, 1940 – present) is an American nurse theorist and nursing
professor known for her “Theory of Human Caring” humans cannot be treated
as objects and that humans cannot be separated from self, other, nature, and
the larger workforce.” The human being is defined as “…a valued person in and
of him or herself to be cared for, respected, nurtured, understood and assisted;
in general, a philosophical view of a person as a fully functional integrated self.
Nursing is concerned with promoting health, preventing illness, caring for the sick,and restoring health.” It focuses on health promotion, as well as the treatment of
diseases. Watson’s Theory of Human Caring is found in the 10 Caritas Processes: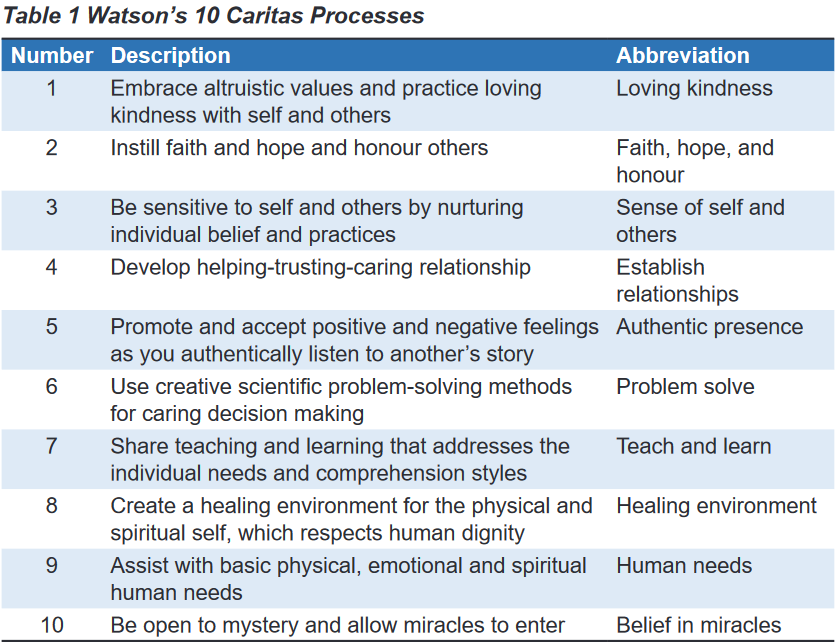
Watson’s theory has been validated in outpatient, inpatient, and community health
clinical settings and with various populations, including recent applications with
attention to patient care essentials and simulating care. Watson’s theory calls upon
nurses to go beyond procedures, tasks, and techniques used in practice settings,
coined as the trim of nursing. Watson’s writings focus on educating graduate
nursing students and providing them with ontological, ethical, and epistemological
bases for their practice, along with research directions. Watson’s caring framework
has been taught in numerous baccalaureate nursing schools.Jean Watson’s metaparadigm
• Person: Human being is a valued person to be cared for, respected, nurtured
understood, and assisted, in general a philosophical view of a person as fully
functional integrated self.• Health: Is the unit and harmony with the mind, body, and soul, health is
associated with the degree of congruence between the self as perceived and
the self and the self as experienced.• Nursing: Is a human science of persons and human health-illness experiences
that are mediated by professional, personal, scientific, esthetic and ethical
human care transactions.• Environment: Society provides the values that determine how one should
behave and what goals s one should strive towards.Application of Jean Watson theory in nursing education and practice:
Watson’s theory is used in all health facilities today (hospitals, health centers,
community settings) whereby nurses involved in the care of inpatients and
outpatients using human caring theory to promoting patient health, preventing
illness as well as the treatment of diseases. In nursing education, students are
educated human caring theory which provide them with ethical, and knowledge
base for their practice.Self-assessment 1.4.5.
1) Which of the following is the theory of Jean Watson?
b) Environmental theory
c) Human Caring
d) Need Theory
e) Self-care deficit2) The following are Caritas Processes. Except.
a) Be open to mystery and allow miracles to enter.
b) Develop helping-trusting-caring relationships.
c) Share teaching and learning that addresses the individual needs and
comprehension styles.
d) Impose your personal beliefs about wellness on others.End unit assessment 1
1) Mrs. UWIMANA is brought to the hospital after sustaining an accident, he is
bleeding and has multiple wounds on her both legs, and clothes were torn
into pieces. She also states that she is dizzy and feeling too much pain, full
of anxiety. The nurse at the hospital immediately received her putting her on
flat bed in clean environment with fresh air and light and start giving her the
medications to calm the pain and fluids to replace fluid loss due to bleeding.
The nurse fails to stop bleeding and call the doctor to help him, the doctor
come and UWIMANA was treated well and become stable. At discharge
time, UWIMANA states that she is very poor and does not have the money to
pay for the service provided. The nurse went to social service in the hospital
to request for social support for Mrs UWIMANA to pay the hospital and find
new clothes. The nurse also told UWIMANA to not worry about her life,
saying that everything will be ok, he started instructing her how to continue
the self-care at home, respecting the hygiene and eating balanced diet.
a) Based on the scenario above, what is nursing?
b) What are the nurse’s roles stated in the scenario?
c) Enumerate the theorists the nurse in scenario referred to, when
giving care to Mrs. UWIMANA and why?2) List the three periods of nursing evolution
3) Match the theorist in column A to their definition of Nursing as one
element of metaparadigm in column B.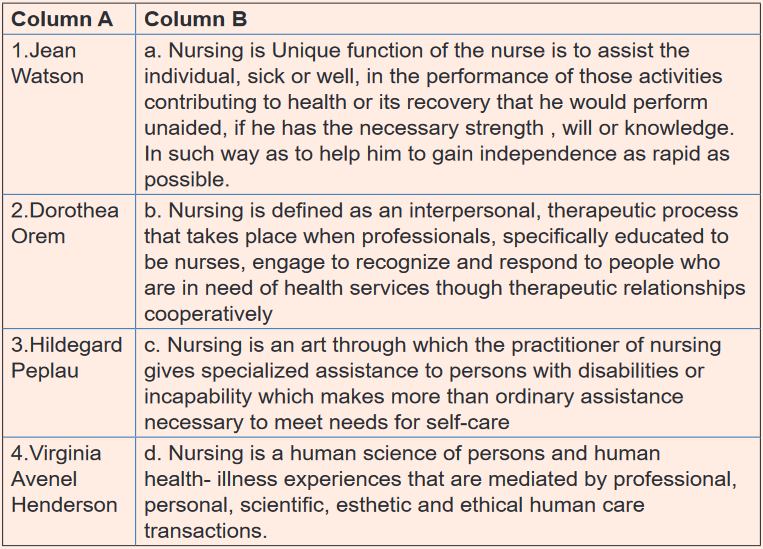
4) Match the following theorists in column A to their corresponding theories
in column B.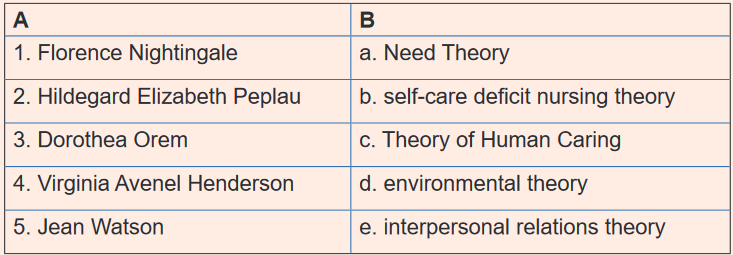
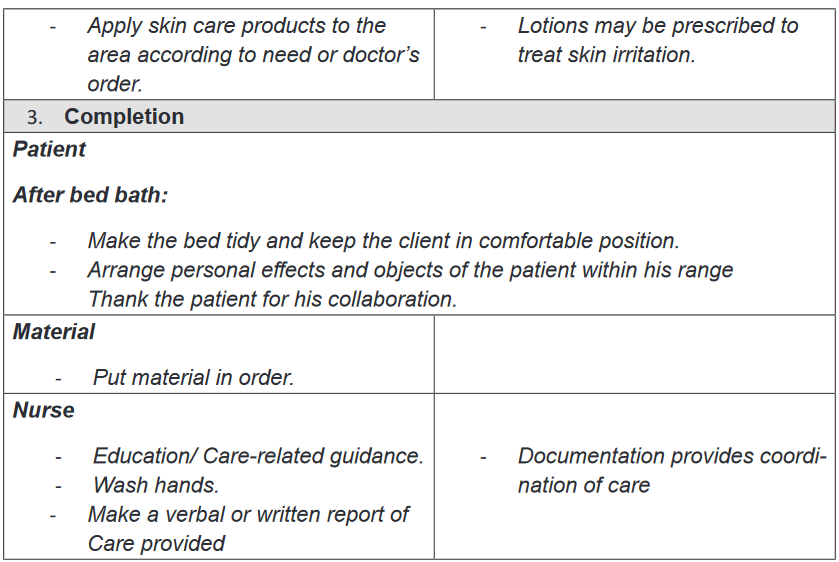
UNIT 2: HYGIENE AND COMFORT CARE OF THE CLIENT/PATIENT
Key Unit Competence:
Perform the Nursing care procedures related to hygiene and comfort of the client/
patient.Introductory activity 2
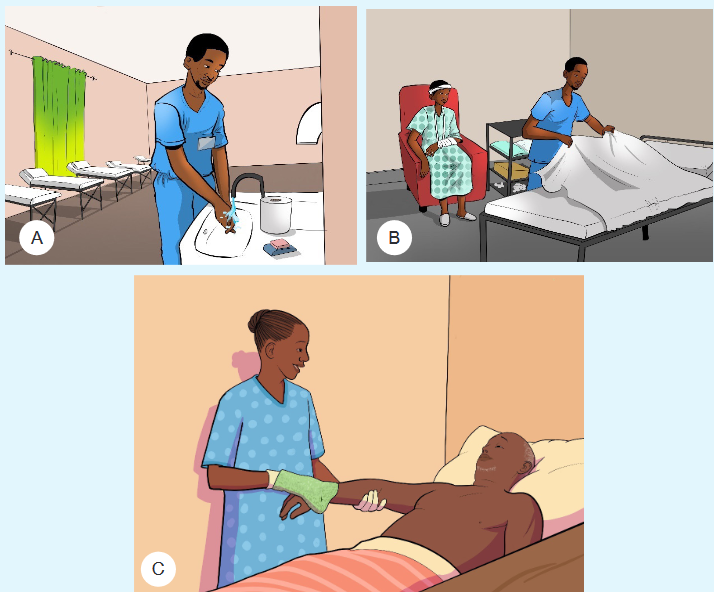
1) The nurse in image A is nearer to the hand washing facilities as it
requires her to perform hand hygiene before going to provide care to
patient. If water or sop is not available, suggest other possible means to
use while ensuring hand hygiene.2) Observe the image B and think about the hygiene and comfort care that
have been provided to the client3) Observe carefully the image C, and identify which kind of care that the
nurse has provided to the patient in bed. Suggest other care that should
be provided to such kind of client.2.1. Hands hygiene and gloving
Learning activity 2.1.
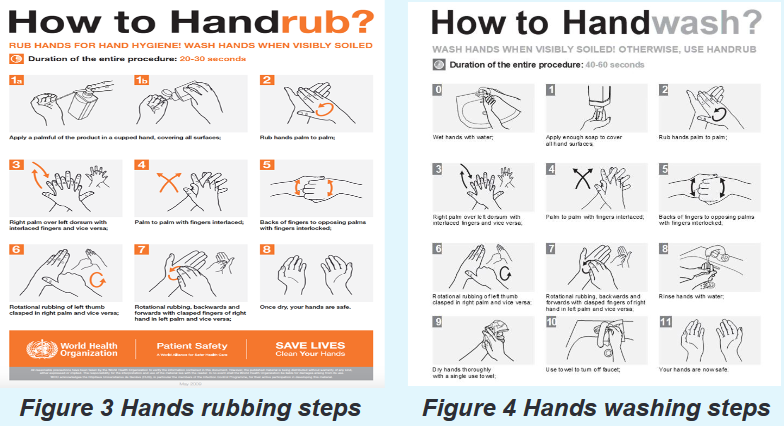
Look at the following figures (Figure 2, Figure 3 and Figure 4) and the
scenario below to respond to the learning questions asked.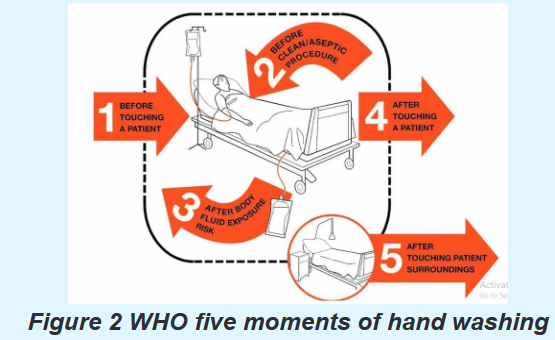
Scenario: A nurse Mary was assigned to provide care to Mr. Paul (Mr. Paul is a
patient who is very dirty) and Mary is required to wash or rub hands to prevent
the cross-infection. Before arriving to Paul, Mary was required to wear proper
gloves since Mr. Paul was bleeding and had skin rashes.1) By looking at the above pictures and by reading book from school library
or other additional resources from internet, explain the following terms:
a) Hand washing
b) Hand rubbing2) Based on the figure 1, explain the five moment of hand washing according
to WHO.3) Referring to the figure 2 and figure 3, demonstrate the technique of hand
washing and hand rubbing4) Based on the scenario, explain the purpose of wearing gloves.
2.1.1. Hands hygiene
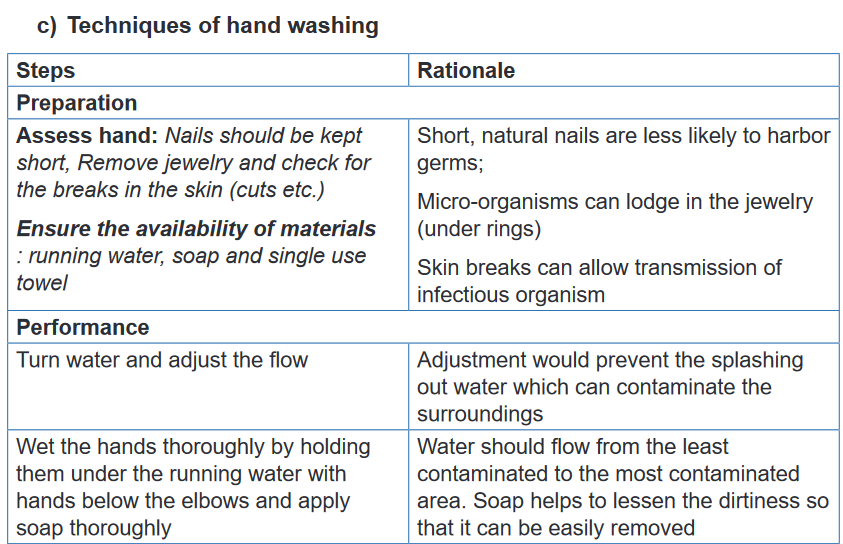
a) Definition and importance
Hygiene refers to conditions and practices that help to maintain health and prevent
the spread of diseases (WHO,2009); this practice is very important for better health.
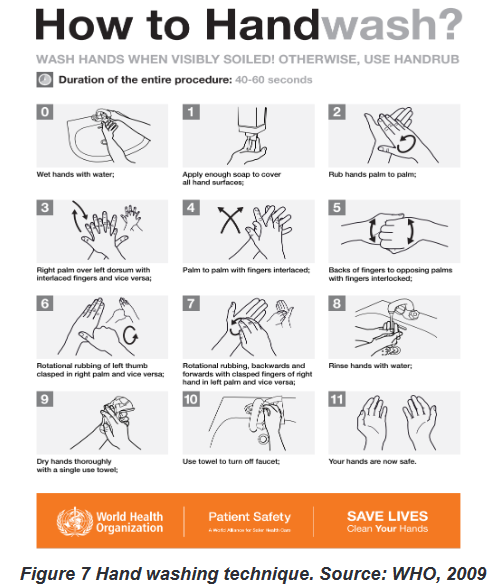
Hygiene includes bathing, toileting, general body hygiene and grooming.Hand hygiene is the most important aspect of the infection control. Hands, the
main pathway for germ transmission in health care settings should be carefully washed
with water and soap or rubbed with appropriate hand sanitizer to remove germs.Hand washing: is the act of cleaning hands using soap and clean water to remove
harmful germs (viruses, bacteria, and other germs), dirt, grease, or other harmful and
unwanted substances stuck on the hands. After washing the hands should be dried.Hand rubbing: Is the act of cleaning hands using an alcohol-containing
preparation (liquid, gel or foam) designed for application to the hands to inactivate
microorganisms and/or temporarily suppress their growth.b) Indications and WHO 5 moments of hand washing
It is indicated that nurses and health care providers should wash their hands more
frequently; that is before and after each procedure and each time your hands are
soiled or suspected to have contracted germs. There are 5 moments recommended
by WHO to wash hands as shown in Figure 5 Five Moments of hand washing
recommended by World Health Organization. Source: WHO, 2009.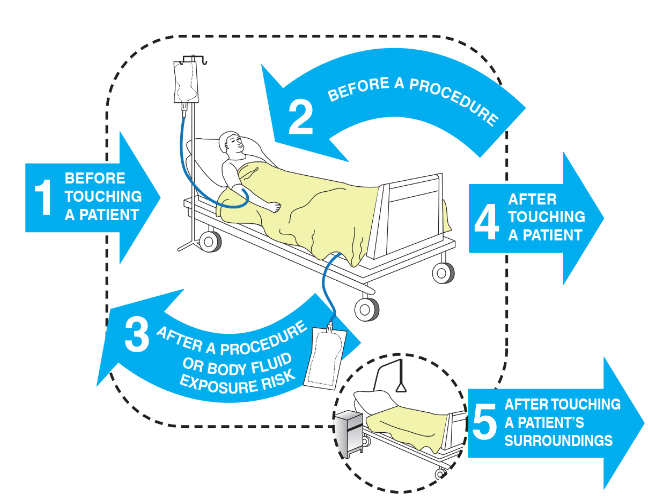
Figure 5 Five Moments of hand washing recommended by World Health
Organization. Source: WHO, 2009
The hand hygiene would not only refer to the technique but also the substance
used to clean. Hand hygiene requires the following materials: running water, soap
and single use paper dryer and appropriate hand sanitizer (when hand rubbing is
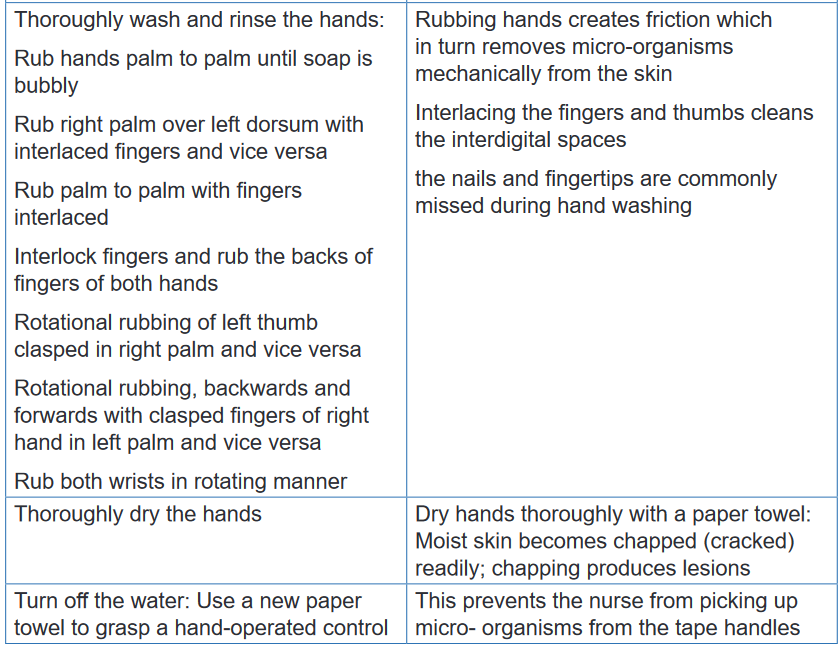
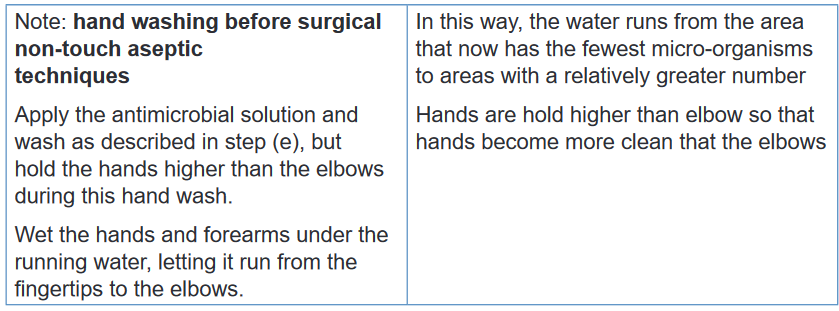
preferred).According to the WHO, there are techniques to follow while washing (see Figure 6)
or rubbing hands (see Figure 7).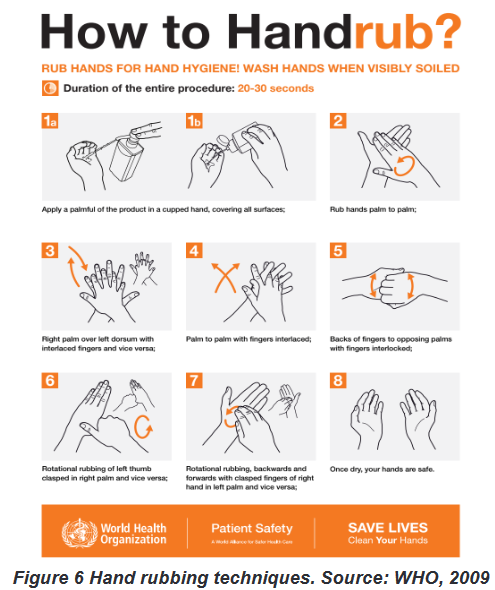
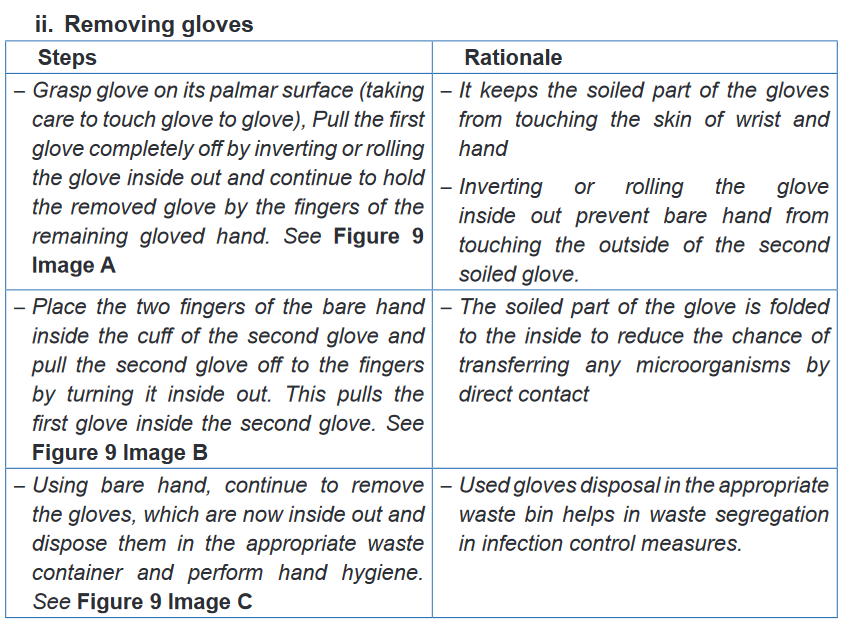
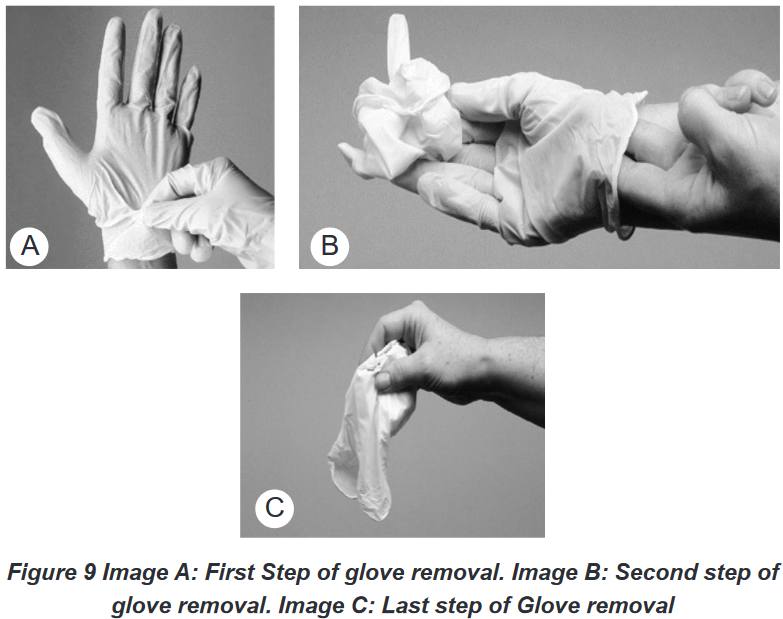
2.1.2. Hand gloving
a) Importance of hand gloving
Complementary to hand hygiene, hand gloving is one of the mechanisms to prevent
the spread of micro-organisms . There are three purposes of hand gloving: firstly,
they protect nurses’ hands when handling substances; secondly, they reduce
the likelihood of transmitting micro-organisms from nurses to the patient and
vice-versa, thirdly, they reduce the possibility of transmitting from one patient
to the other. Gloves should be changed between individuals, and one must wash
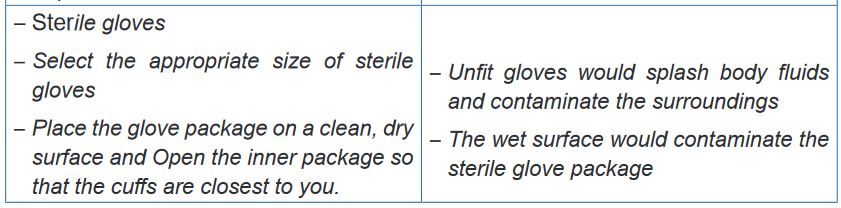
hands after removing gloves.b) Non-sterile and sterile gloving
Gloves are categorized in two types depending to the use: when performing septic
techniques, use clean disposable gloves (also called non-sterile gloves), and
when performing a sterile technique, use sterile gloves.Indications and contraindications
In health care settings the medical gloves are indicated in the following conditions:
protection of the wearer from contamination with blood, secretions, and excretions
and the associated risk of contamination with pathogens capable of reproduction.;
prevention of pathogen release from the hand into the sterile work area during
aseptic procedures; protection of hands from chemicals; pathogen barrier as
protection from biological agent and radiation protection. Gloves are contraindicated
in the following conditions: when a health care provider is away from the bedside or
laboratory bench; when health care provider is in nursing stations to handle phones
or charts; in time of handling clean linens and in case of cleaning non-contaminated
equipment or patient-care supplies (e.g. plate, cups etc.).
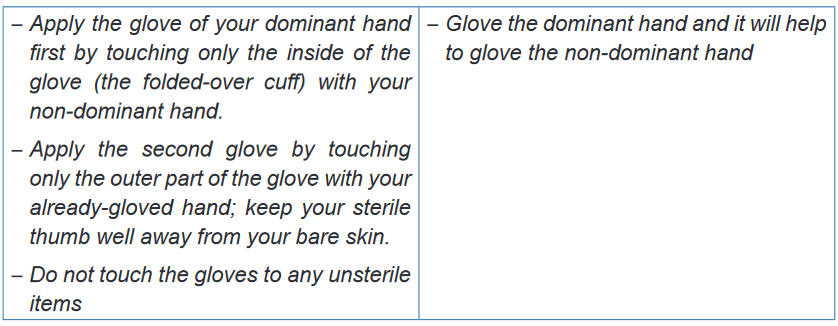
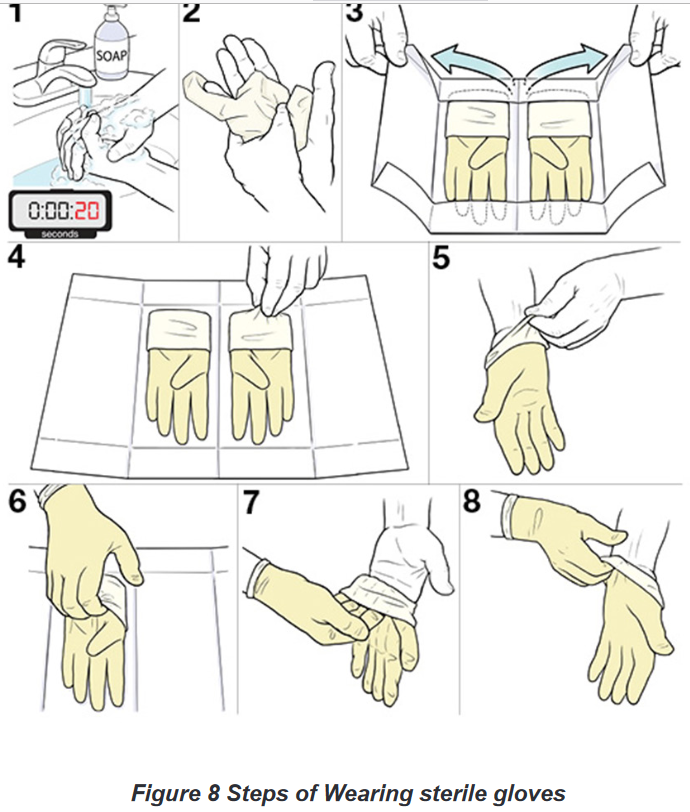
a) Techniques of gloving
Donning disposable clean gloves does not require special techniques, however
there are precautions: one’s hands must be dry, finger nails cut short and
jewellery removed to prevent tearing gloves. Donning sterile gloves on the
other hand, requires specific technique to ensure that no micro-organism is
introduced in a wound or body orifice which should be sterile.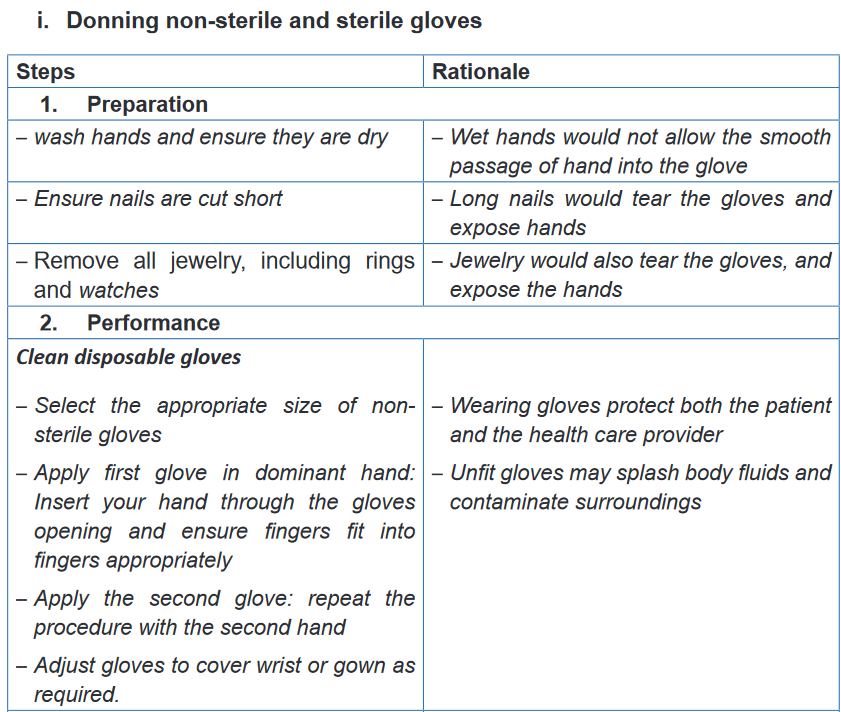
Self-assessment 2.1.
1) A Patient is bleeding on the left leg due to road accident. The nurse
has to get ready to help the patient to stop bleeding nurse is required to
perform hand hygiene before wearing the gloves. What kind or cleaning
technique should the nurse use?
a) Hand washing
b) Hand cleaning using chlorhexidine
c) Hand gloving
d) All the above2) What is the difference between hand rubbing and hand washing
3) Explain the WHO five moments of hands washing
4) Why should the nurse wash his or her hands or perform an alcohol-
based hand rub and then wear clean gloves?5) Nurse was proving bed making but before to wear gloves, she rubs
her hands with Alcohol and the patient asked her Why? Which of the
following is a benefit of an alcohol-based hand rub that the nurse should
explain?
a) Destroys active microbes but not spores
b) Provides the fastest and greatest reduction in microbial counts on
the skin
c) Leads to irritation and drying of the skin compared with soap
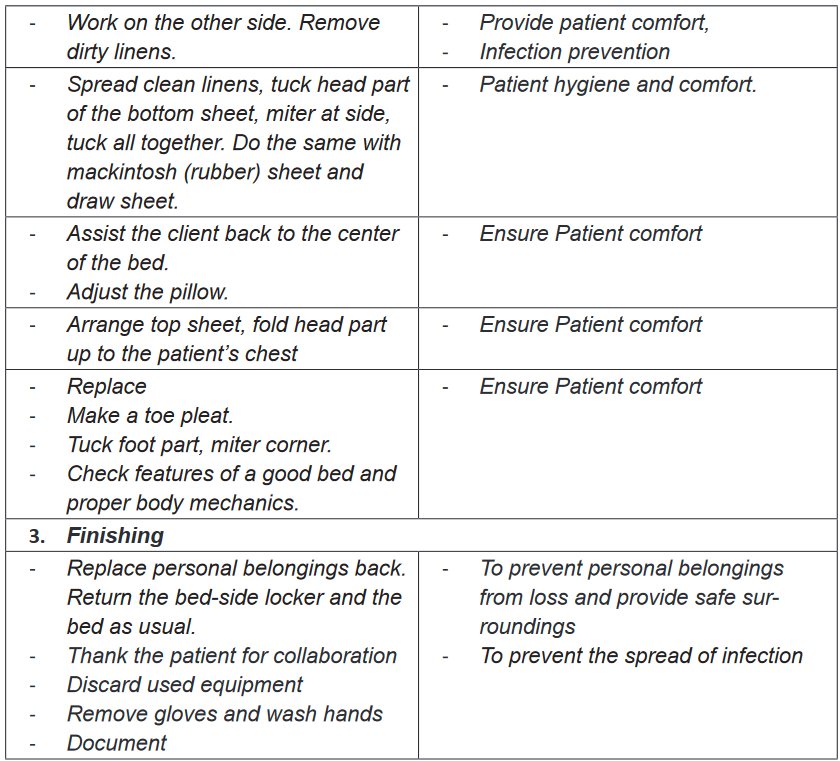
d) Controls viral replication or release from the infected cells.2.2. Bed making
Learning activity 2.2.
Question one
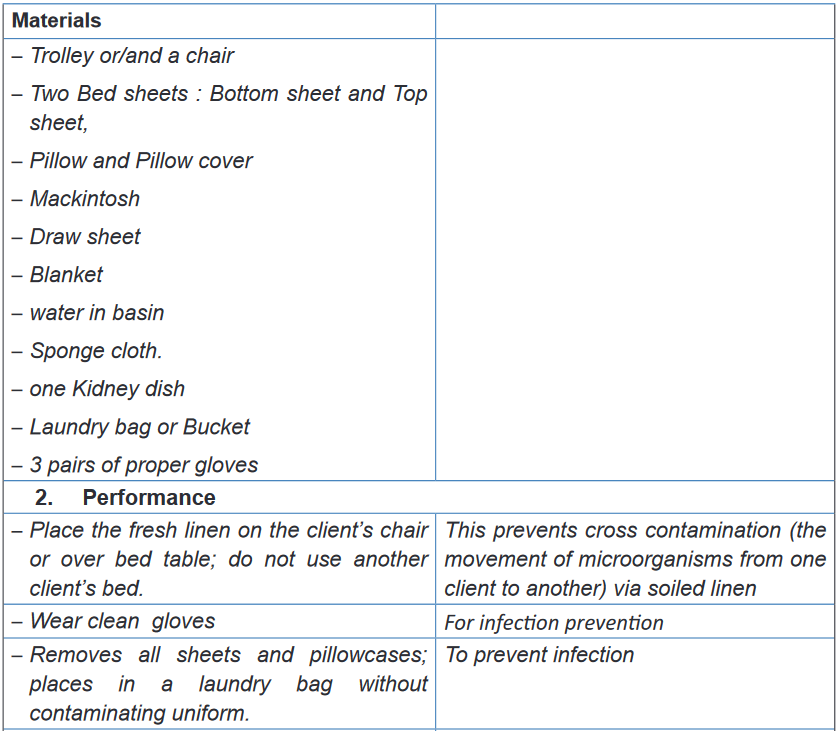
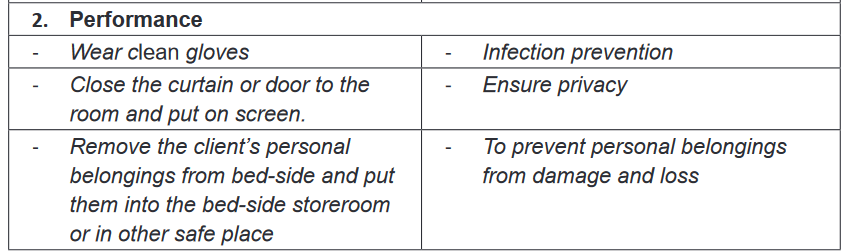
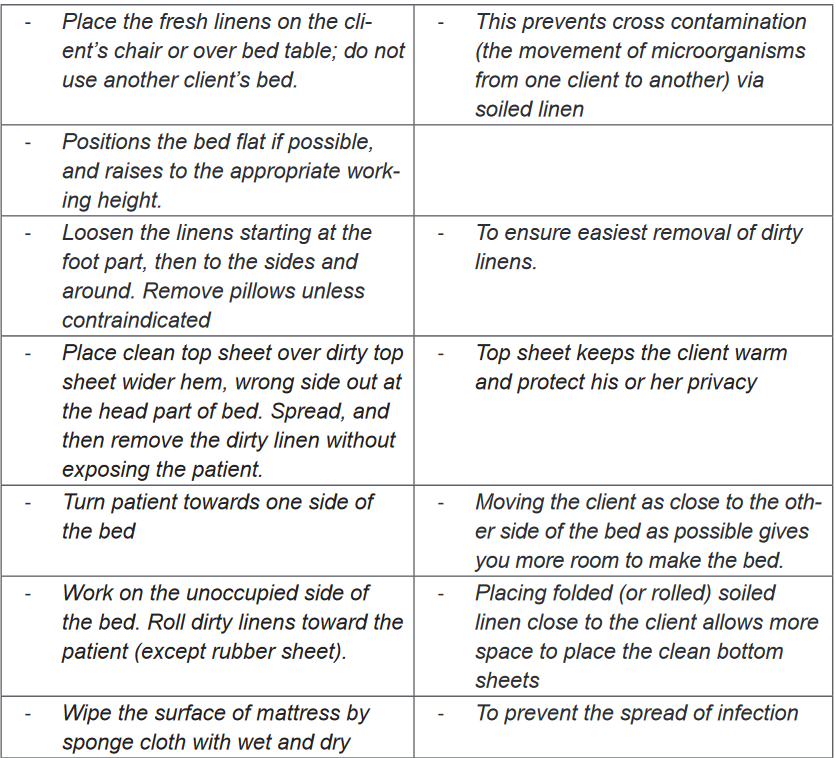
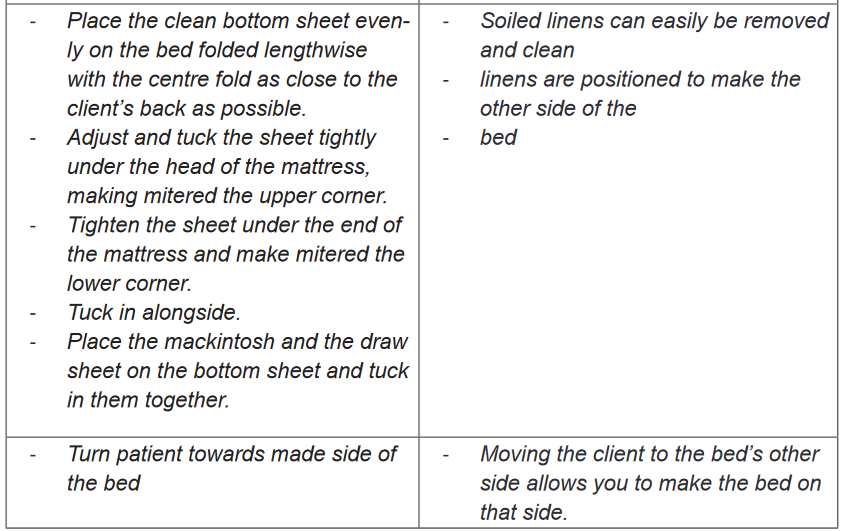
1) The images A & C shown above shows nurses making beds. After
observing the above image, what do you think as the purpose of bed
making?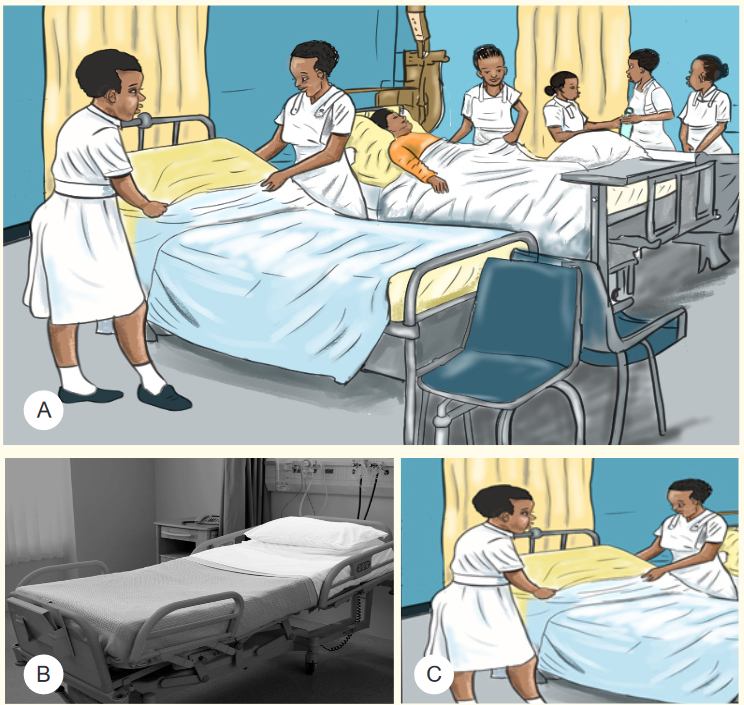

2) List the materials that you have observed in the above image A
3) Observe carefully the images A, B, C and D and highlight the difference
between them
4) Observe the well-made bed and try to make the bed in the same wayQuestion two
Mr. KARINGANIRE is on his day 7 of hospitalization at health facility, is very weak
and is not able to perform any activity, but is able to turn on his left side, he stays
in his bed, and he needs assistance for everything. One morning nurse wants to
change his bed sheets for maintaining the comfort of Mr. KARINGANIRE
1) Based on KARINGANIRE condition is it possible to change his bed
sheets? Yes/No : explain your Answer
2) What do you think as the materials will be used to make KARINGARE’S
bed?
3) What is the importance of listed materials?2.2.1. Definition and Purpose
Bed making is the technique of preparing different types of bed and is required for
all patients. Nurses need to be able to prepare hospital beds in different ways for
specific purposes. Bed making is done for providing comfort, facilitating movement
of the patient and alleviate the pain. It helps to conserve patient’s energy and
maintain current health status. It reduces the risk of infection by maintaining
a clean environment and permitting the physical rest. Bed making is one of the
measures used in prevention of bed sores.2.2.2. Principles of bed making
Prior to bed making, there are principles that have be followed, these are:
1) Arrange bed coverings in order of use
2) Wash hands thoroughly after handling a patient’s bed linen
3) Hold soiled linen away from uniform
4) Linen used for one client is never placed on another client’s bed
5) Soiled linen is placed directly in a portable linen hamper or a pillow case
before it is gathered for disposal.
6) Soiled linen is never shaken in the air because shaking can disseminate
secretions and excretions and the microorganisms they contain.
Fundamental of Nursing | Associate Nursing Program | Senior 4 43
7) When undressing and making a bed, conserve time and energy by undressing and
making up one side as completely as possible before working on the other side.
8) Keep your back straight as you work for preventing back injury
9) To avoid unnecessary movement to the linen supply area, gather all needed
linen before starting to make a bed.
10) While tucking bedding under the mattress the palm of the hand should face
down to protect your nails.2.2.3. Types of bed making
There are 2 two main types of bed making: occupied and unoccupied bed. An
unoccupied bed can be either closed or open. Generally the top covers of an open
bed are folded back (thus the term open bed) to make it easier for a client to get in.
Open and closed beds are made the same way, except that the top sheet, blanket, and
bedspread of a closed bed are drawn up to the top of the bed and under the pillows.While occupied bed is a techniques of making bed for very weak patients who are not
able to get out the bed or restricted in the bed by traction or other therapy condition.2.2.4. Techniques of bed making
a) Unoccupied bed making
Purpose: Unoccupied bed making can be done with different purposes, these are but
not limited to: To prepare the bed for the clients return, to provide a clean environmentTo provides a good appearance and to minimize source of infection.
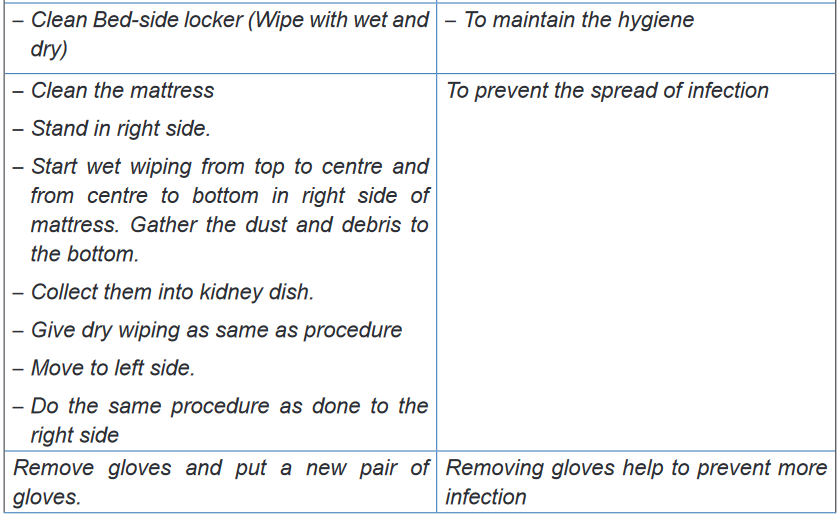
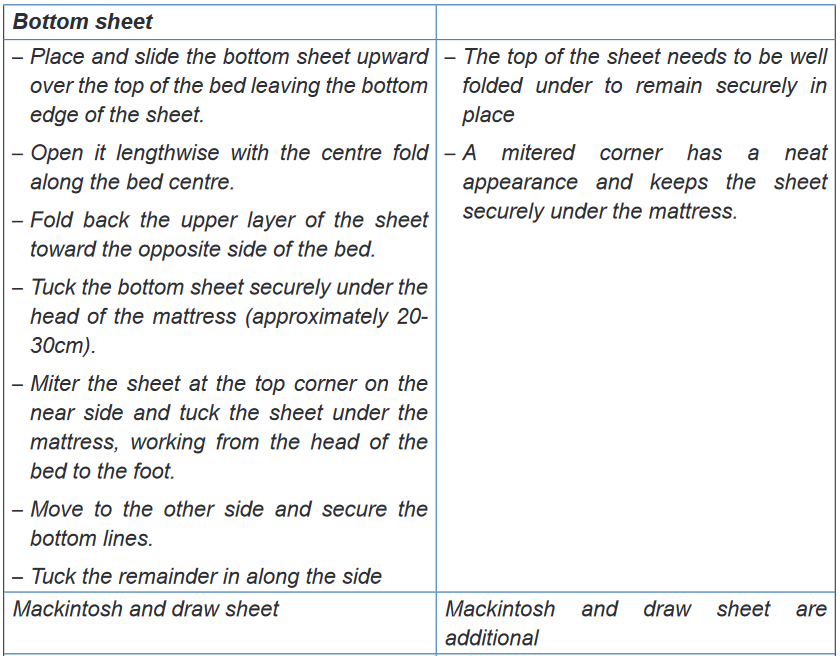
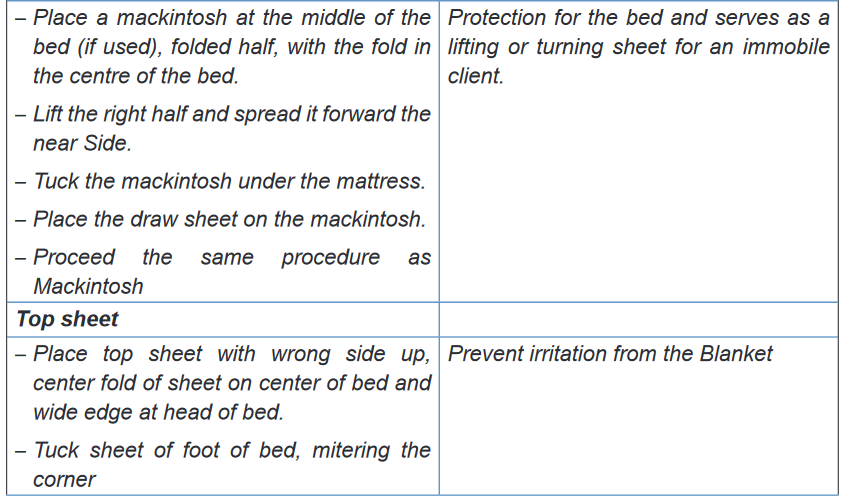
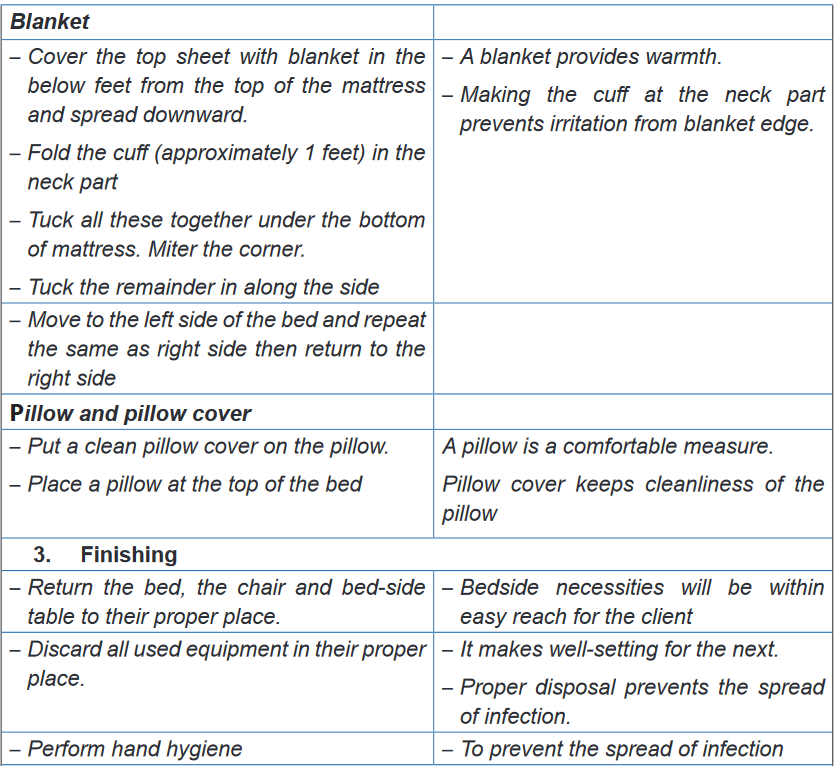
b) Occupied bed making
Purpose: the occupied bed making can be done with different purpose, these are but
not limited to: to provide clean, safe and comfortable bed for the patient, to promote
rest and sleep, to reduce the risk of infection by maintaining a clean environment,
to prevent bed sores and to observe patient and to prevent complications.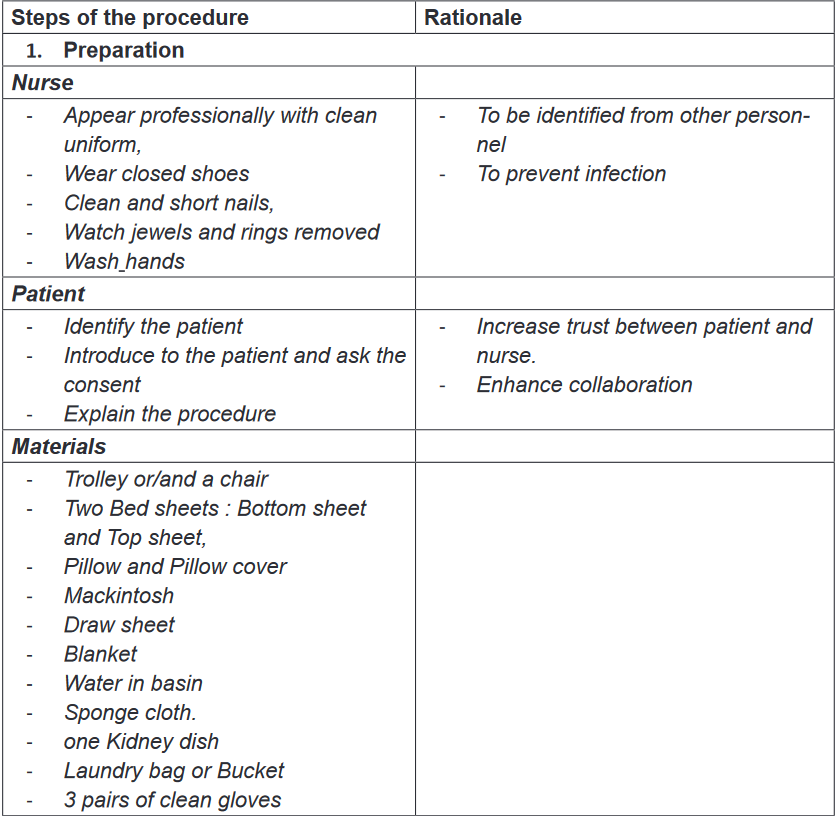
Self-assessment 2.2.
1) Which of the following is true about handling linen?
a) Always carry clean and soiled linen next to your uniform
b) Put the soiled line on the floor when making an occupied bed
c) Soiled linen is never upset(shaken in the air
d) Linen used for one client is directly used for another client’s bed.2) When making an occupied bed
a) The patient is in the bed
b) Keep the bed in the low position
c) Make the top first , then the bottom
d) The patient is out of the bed3) The good ways of making a patient bed are the following except:
a) Complete one side of the bed at time
b) Remove soiled linen a few pieces at a time
c) Move quickly and efficiently
d) Keep you back straight as you work4) When changing the linen that is soiled with body fluids
a) Place the linen on the floor until it can be removed
b) Wear gloves and avoid contact with your uniform
c) Fold or roll with the soiled side out
d) Ask the patient to try to make it to the bathroom next time5) When entering a patient’s room to make a bed, what are the items do
you need to have in hand before entering the patient’s room?6) In skills lab, demonstrate the following techniques of Occupied and
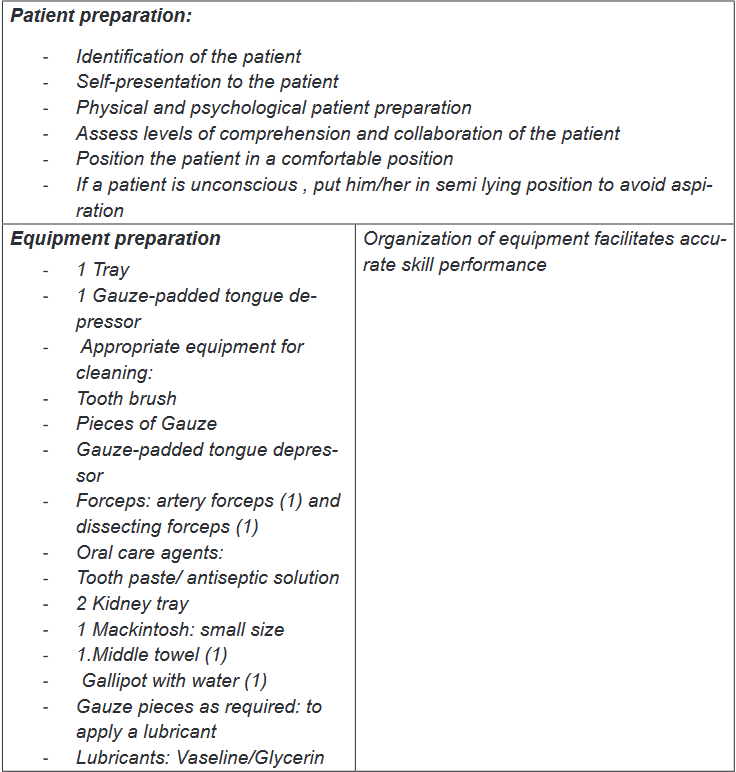
unoccupied bed making.2.3. Bed bath
2.3.1. Complete bed bathLearning activity 2.3.1.
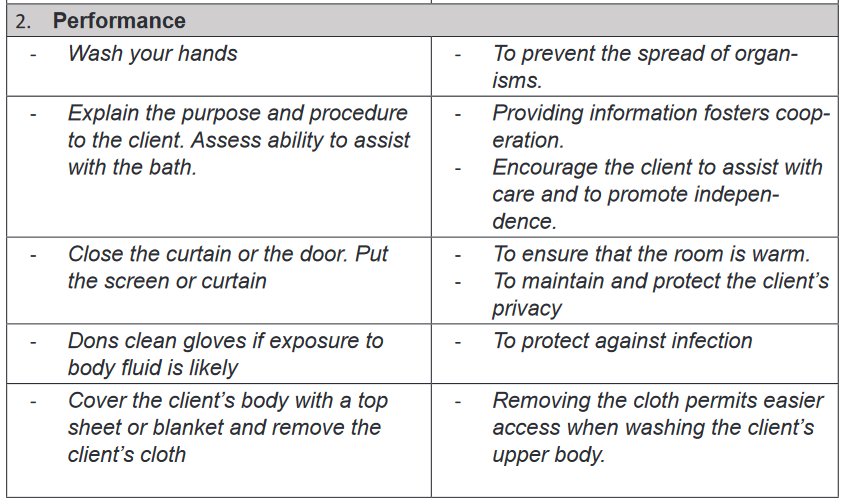
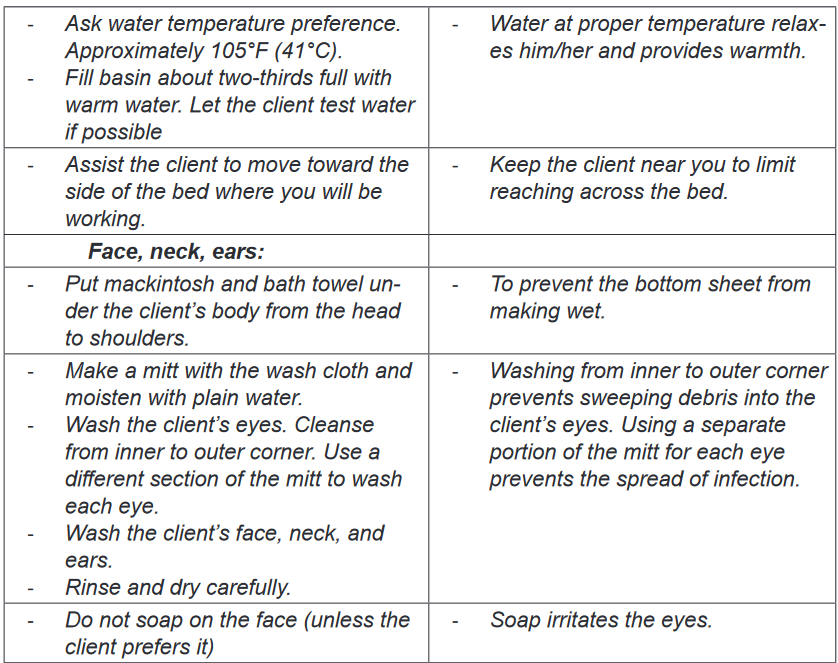
Mr. GAKWAYA was hospitalized for 5 days, he was very sick and he had no
caregiver. A day duty nurse entered in Mr. GAKWAYA’s room and found there was
bad smell. In a very weak voice Mr. GAKWAYA told the nurse that he did not bath
since three days ago. The nurse approached him and found that his bed linens
were dirty and decided to provide a bath. The nurse opened the window to air the
room and went back to the nursing station to prepare the following materials: two
basins, bucket containing water, 2 pair of proper gloves, soap, body lotion/cream,
2 bath gloves, folded screen (for privacy), dirty linen container, bed sheets and
cleaned draw-sheets, individual blanket (Bed-cover), clean clothing or Hospital
gown and bed cleaning material to provide bed bath.
After bed bath Mr. GASANA thanked the nurse and reported that he was feeling
much better and that he will sleep well since last night he did not sleep well.
When the medical team come to visit Mr. GASANA, there was a fresh air in the
room and GASANA was happy.Based on the above scenario, respond to the following questions:
1) Explain the purpose of bed bath
2) Identify the materials needed in bed bath
3) What do you think as the indications of bed bath
4) Watch the video in the skills lab on bed bath and list the steps of bed bath.a) Importance of bed bath
Bed bath helps to stimulate the functions of the skin and increases circulation.
The bath cleanses body of dirt, bacteria, dead skin cells, sweat and odors. Bed
bath provides the opportunity to assess the skin for lesions and breakdown. Bed
bath help the patient to feel comfortable and relaxed which enhance rest and
sleep that promote healing and restoration of health. In comatose patients, who
have neurological impairment, the bath increases sensation by providing sensory
input for the brain to process. Bathing provides improved self -esteem of the
patient. Providing a bed bath helps to establish the Nurse-patient Relationship
by creating trust and rapport between the nurse and the patient.b) Indications and contraindications
In clinical setting Bed bath is mainly indicated for patients who are physical or
mentally impaired due to different condition such as unconscious or semiconscious
patients, postoperative patients, patient with strict bed rest, paraplegic patients,
orthopedic patients in plaster, cast and traction and seriously ill patients. However,
bed bath may be contraindicated is some cases such as: Hypothermia, convulsion,
fresh burns, varicose veins and advance vascular diseases of the legs and feet.c) Principles of bathing the patient
Before performing bed bath of the patient, the nurse should assess patient
‘abilities; such as to understand and follow directions, the degree of assistance
needed during the bath and tolerance of the physical demands during a bath
such as whether the patient is too weak, too ill, or in too much pain to participate.
During the bathing procedure; patient’s preferences such as bathing timing, culture
should be respected.BOX 2.3.
Principles of bed bathing
• Keep the patient warm at all times
• Position a linen skip near the patient and dispose of used linen
immediately to reduce dispersal of microorganisms and dead skin cells
into the environment
• Only expose the area of the body being washed
• Change water if it becomes dirty or cold and always after washing the
genitalia and sacrum
• Change wash cloths if they become soiled and after washing the genitalia
and sacral area
• Check skin for pressure damage
• Avoid contaminating dressings and drains with water
• Pat the skin dry to reduce the risk of friction damage
• Separate skin folds, and wash and pat them dry
• Use the correct manual handling procedures and equipment to avoid
injury to yourself and the patient
• If the patient is unconscious, remember to talk them through what you
are doing; nurses should not talk over the patient.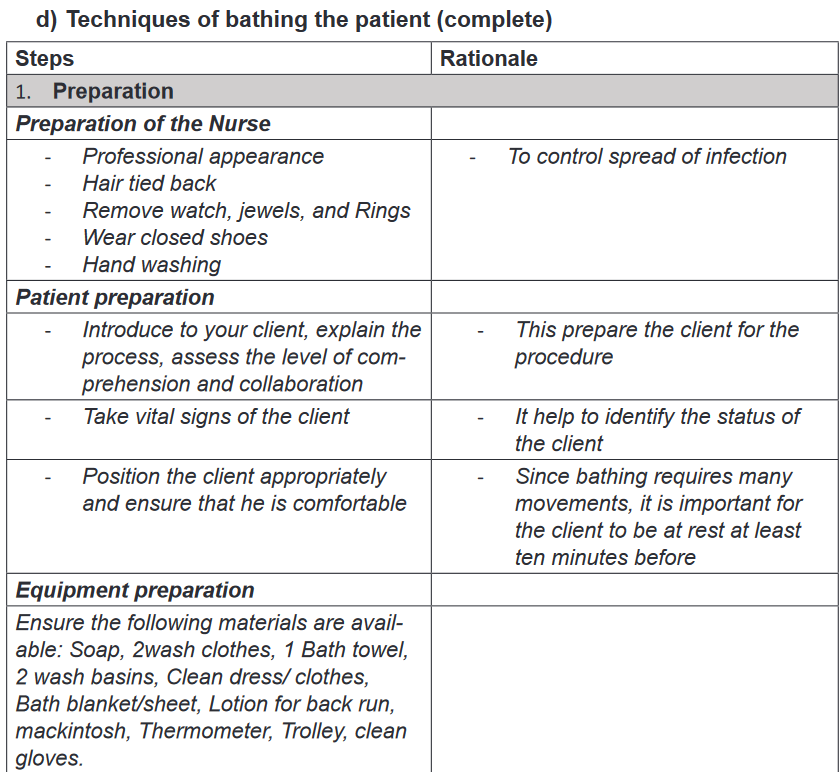
Self -assessment 2.3.1.
Answer the following exercises by marking the lettered response that best
answers the question:
1) When performing a bed bath you should change water when it becomes:
a) Cold, dirty, or excessively soapy.
b) Warm , excessively soapy or too dirty
c) Extremely soapy, dirt or too clear
d) Dirty, old, or too cold2) Which area of the body should not be exposed when washing the upper
and lower limbs?
a) Genitalia.
b) . Feet.
c) Thigh.
d) Stomach area3) When preparing to give complete bed bath to a patient, what would the
nurse do first?
a) Gather the necessary equipment and supplies.
b) Remove the patient’s gown or cloths while maintaining privacy.
c) Assess the patient’s preferences for bathing’s practices
d) Turn the patient in the lateral position4) State at least 5 guidelines that the nurse needs to follow when performing
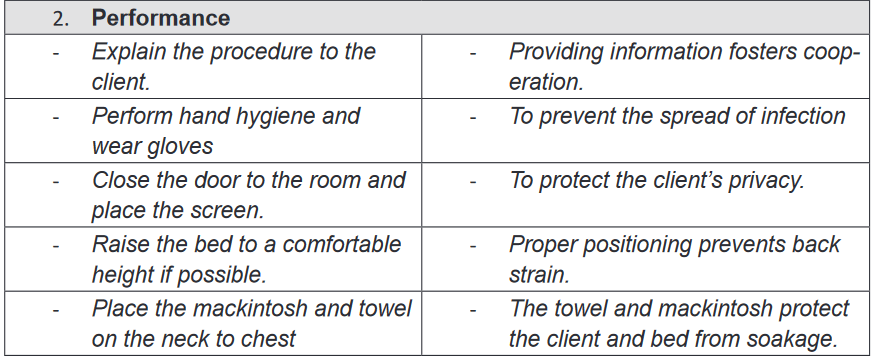
a complete bed bath.2.3.2. Partial bed bath
Learning activity 2.3.2.
Mrs. MUKANEZA is in the hospital for several days, she is very sick and she is
not able to maintain her body hygiene without assistance. This morning Nurse
Jane did her complete bath.Nurse Jane after completing her bed bath; assisted her to brush her teeth
to ensure a good oral hygiene. While the Nurse was trying to comb the hair
of Mrs. MUKANEZA , she found that the hair were dirty and she decided to
shampooing her.Mrs. MUKANEZA had stool and urines incontinence (not able to control stool
and urines), few hours after her bed bath she passed urines in her bed. Nurse
Jane decided to clean her perineal area and to change her bed sheets.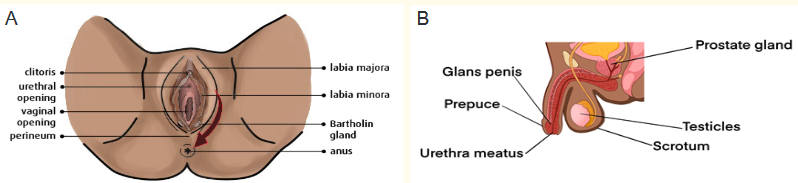
After reading the above scenario and to observe carefully the above image
respond to the following questions:
1) What do you think the oral hygiene will help Mrs. MUKANEZA?2) What do you think as the benefit of shampooing the hair of Mrs.
MUKANEZA?3) Between image A and B what is the image that correspond to the above
scenario and explain why.4) As Mrs. MUKANEZA was passing urines in her bed, nurse Jane
performed her perineal care, observing the image A , what does the
arrow on the image indicate for?5) Observing the image A what do you think as the risk for Mrs. MUKANEZA
if the perineal hygiene is not well kept? And explain why.a) Definition
Partial bed bath consists of bathing selected body part that may cause discomfort if left
unbathed. Most performed partial baths are: perineal care, oral care, foot bath, hair
shampooing and therapeutic baths (SITZ bath).b) Techniques of partial bed bath
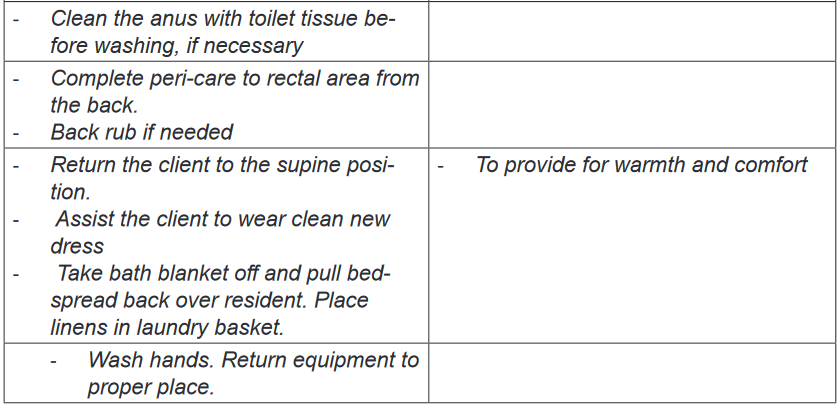
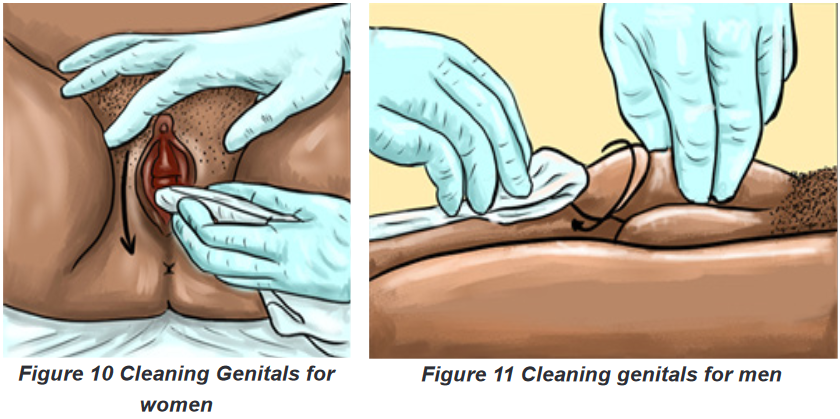
i. Perineal care
Perineal care is also called pericare consists of washing the external genitalia and
surrounding. The perineal area is very exposed to growth of pathogenic organisms
because it is warm, moist and it is not well ventilated. It has many orifices that may
be the entrance of micro-organism in the human body such as urinary meatus,
vaginal orifice and anus.The perineal area is a private part of individual and the perineal care are
embarrassing for many people. The nurse have to build strong relationship with
the client to easy the effectiveness of perineal care. Most people who require a bed
bath from the nurse are able to clean their own genital area with minimal assistance
from the nurse.The perineal care removes normal perineal secretion and odor, it helps to keep
cleanliness and prevent from infection in perineal area and improve the client
comfortable. The perineal care is mostly indicated for patient who are unable to
do self-care, patient with genito -urinary tract infection, patient with incontinence
of urine and stool, patient with indwelling catheter (urinary catheter), postpartum
patients, patients after surgery on the genitor -urinary system and patients with
injury, ulcer or surgery on perineal area.The most important principle to respect during perineal care is to clean the perineum
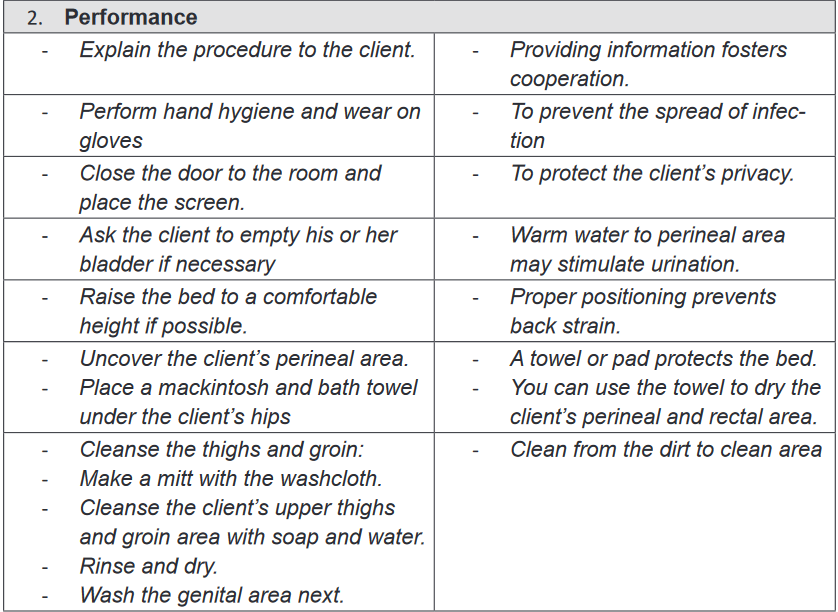
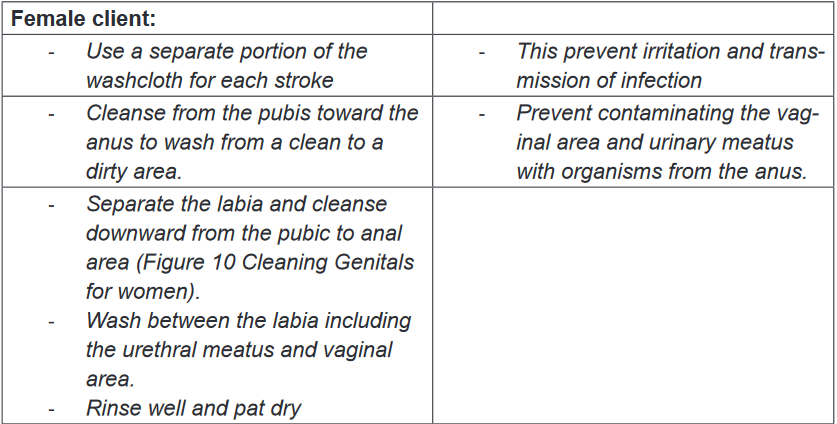
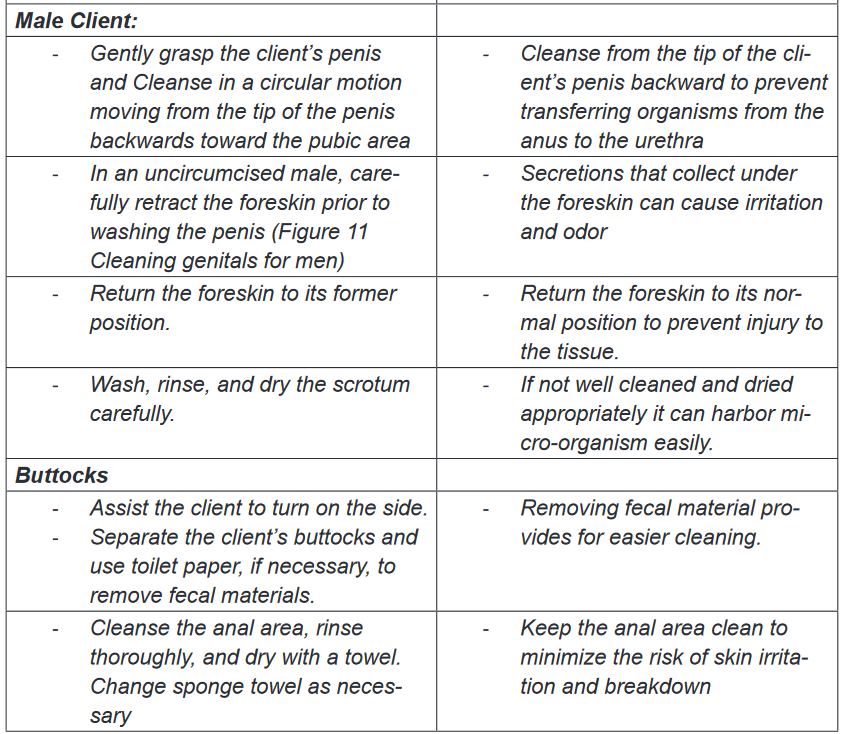
from the cleanest to less clean and to preserve patient privacy.Techniques of perineal care
Purpose: to keep cleanliness and prevent from infection in perineal area and
improve the client comfortable.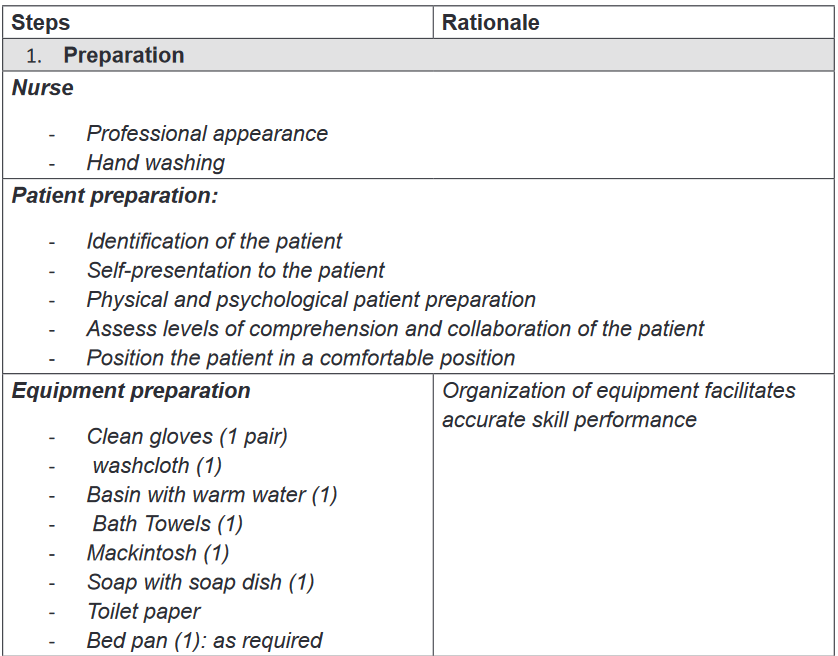
ii. Oral care
Oral care is a fundamental nursing care that consist of keeping mouth and teeth
clean and healthy. Each patient needs oral care; the patients who are confined in
bed with decreased physical and mental capacity need assistance to provide oral
carePurpose: to keep the mucosa clean, soft, moist and intact, to keep the lips clean,
soft, moist and intact, to prevent oral infections, to remove food debris as well as
dental plaque without damaging the gum, to alleviate pain, discomfort and enhance
oral intake with appetite and to prevent halitosis or relieve it and freshen the mouth.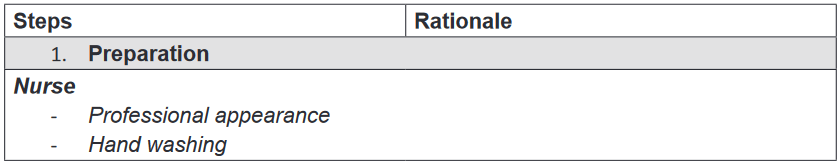
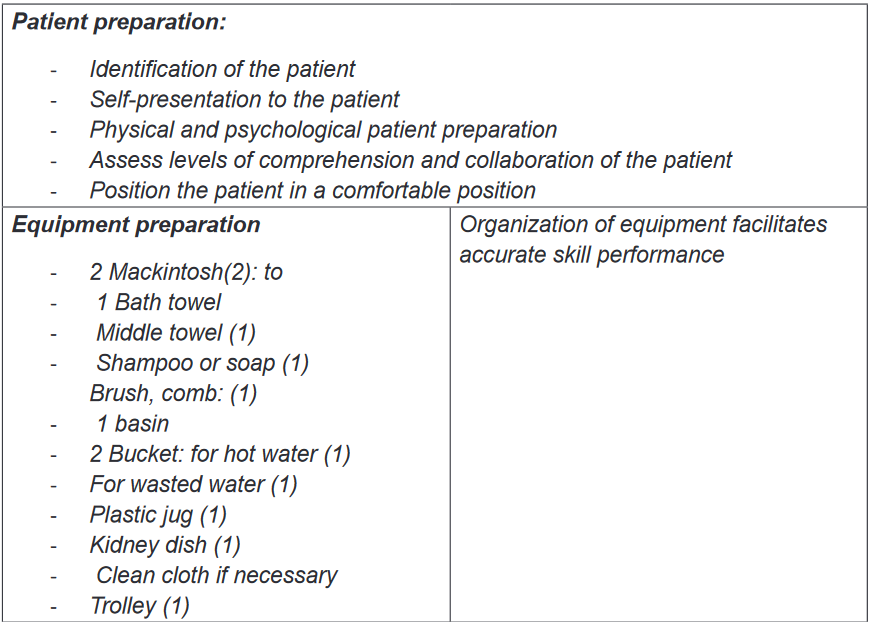
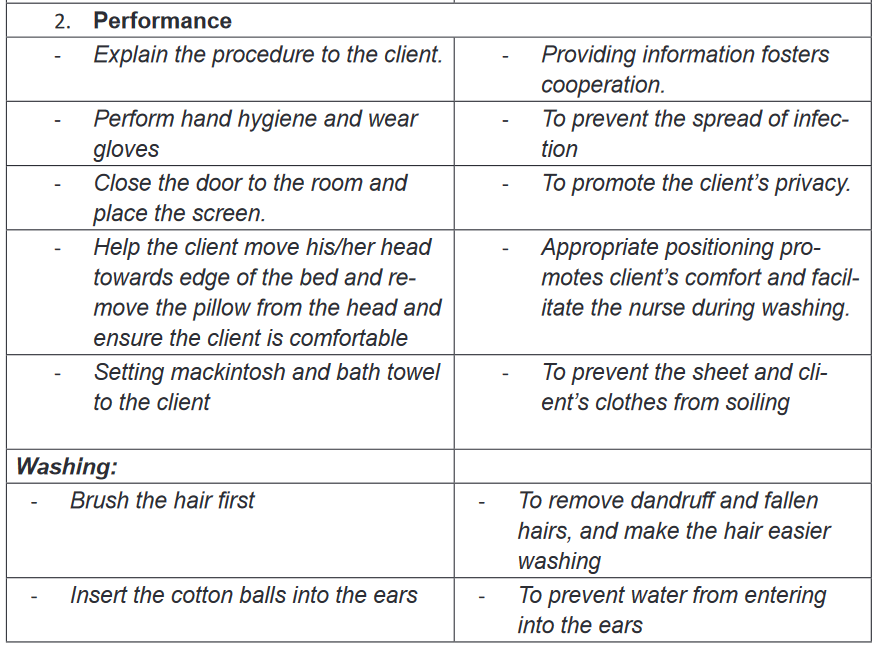
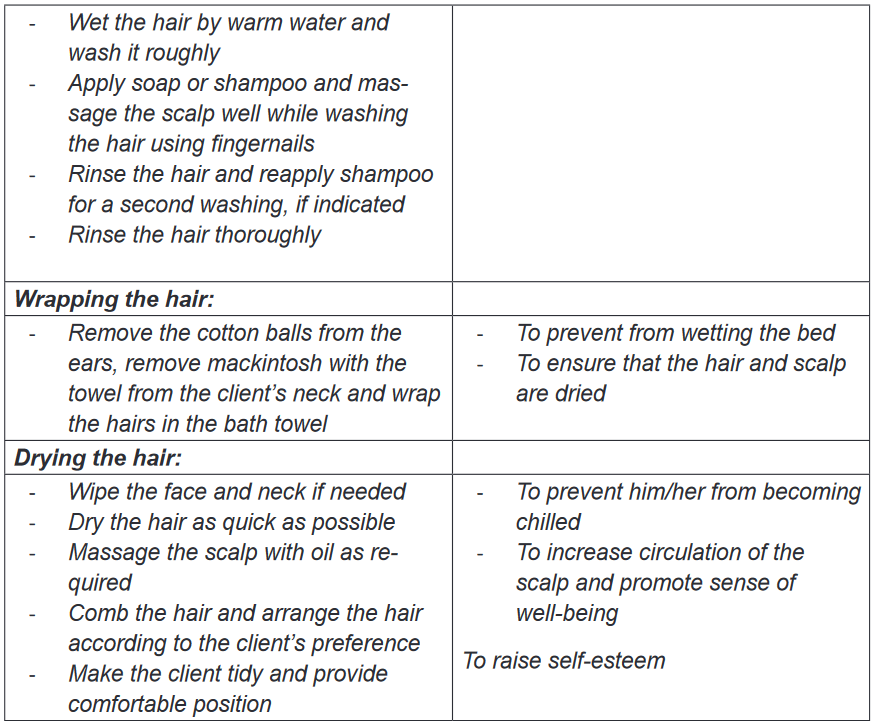
iii. Shampooing
Purpose: It helps to maintain personal hygiene of the client, to increase circulation
to the scalp and hair, promote growing of hair and to make him/her feel refreshed.
Same as other types of bed bath, shampooing is indicated to all patient who are
unable to care for themselves.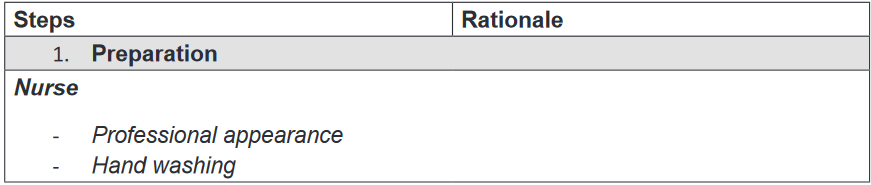
iv. Foot bath
The feet are essential for ambulation and merit attention even when people are
confined to bed. The purpose of feet bath is to maintain personal hygiene of the
client, Soothe sore muscles, to increase circulation and to make him/her feel
refreshed and relaxed. The foot bath is also indicated to all patient with physical
incapacity and is contraindicated to patient with foot injuries. \
\
V. Therapeutic bath: Sitz bath
Definition and purpose
Therapeutic baths are baths that have physical effects; they are given to soothe
irritated skin or to treat an area such as perineum. Medications are placed in water
and the client remain in water for a designed time. A therapeutic bath often last for
20 to 30 minutes.A Sitz bath is a type of therapy that consist of sitting in warm, shallow water to clean
the perineum, which is the space between the rectum and vulva or scrotum. Sitz
is from the German word “Sitzen” which means “to sit”. A Sitz bath helps to clean
and treat certain problems in the anal area, genital area and the perineum. It helps
to increase blood flow to these areas and relax the muscle. A Sitz bath helps to
relieve from pain or itching in the anal and genital area.Indications and contraindications
Sitz bath can be hot or cold; the hot Sitz bath is indicated in case of ovarian pain,
uterine cramps, testicular pain, prostatic problems, intestinal or renal colic, sciatica,
headache; and the cold Sitz bath is indicated in case of uterine prolapse, cystocele,rectocele, constipation and heavy or prolonged menstruation. The alternate hot
and cold Sitz bath is used in case of chronic UTI (Urinary tract infection), pelvic
inflammatory disease, hemorrhoids, fissure, postpartum Contraindications.The Sitz bath is contraindicated in case of hemorrhages, menorrhagia, acute
congestion, acute inflammation, painful conditions with spasms or colic, and heart
problems.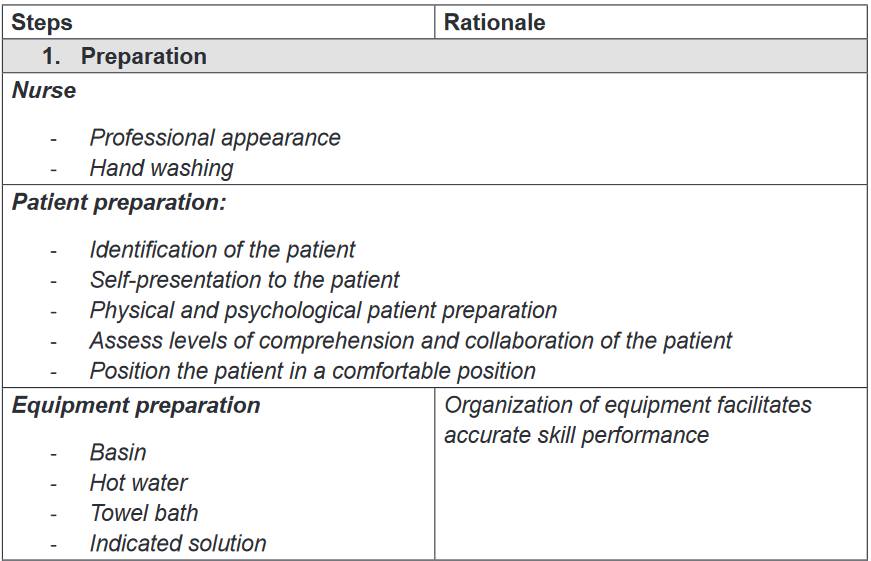
Self-assessment 2.3.
1) When providing peri-care always wash from ______ to _____
2) What is perineal care
a) Washing a patient back
b) Washing a patient’s genital and anal area
c) Giving a complete bath
d) Washing patient’s genitalia only3) For an uncircumcised male patient , the nurse needs to first:
a) Pull back the foreskin
b) Turn the penis to the side
c) Push the foreskin foreword
d) Gently pat the area with a dry towel before washing4) Which of the following statements is correct regarding perineal care?
a) Always wear gloves when providing pericare.
b) Wash the peri area with soap and cold water.
c) Wash from back to front when providing peri care.
d) The client lies on his/her stomach during peri care.5) Why the client is offered the bedpan or urinal before beginning peri care?
6) List two purposes of giving peri care.
7) You ARE giving oral care to unconscious person ,which action is incorrect
a) Provide privacy
b) Place a kidney basin under the chin
c) Place the mackintosh and towel on the neck to chest
d) With your fingers open the client’s mouth.8) In order to prevent aspiration when performing oral hygiene on a person
who is unconscious, they are placed
a) In high Fowler’s
b) In supine
c) In side lying position
d) Reverse Trendelenburg9) Enumerate at least two purposes of foot care
10) Explain the purpose of a Sitz bath
11) During a Sitz bath the patient sit in water for:
a) 45-60minutes
b) 5-10 minutes
c) 40-50 minutes
d) 20-30 minutes2.4. Bed sores or Pressure ulcers
Learning activity 2.4.
Mrs. MUKANKIKO, a 75 years old patient was hospitalized for four weeks,
she was severely sick and she couldn’t move nor turn in her bed and she was
malnourished. While providing bed bath, Mr. KWIZERA, a student nurse in his
first clinical practice, has found that she had redness on her buttocks (redness:
is one the signs of bedsores. A bedsore is a damage to an area of the skin
caused by unrelieved pressure on the area for a long time) due to prolonged
compression on the side she was lying on.Mr. KWIZERA recalled that bedsores can be prevented by changing position,
maintaining adequate nutrition, hygiene (body and surrounding hygiene), and
exercises to promote blood circulation and decided to change position every
two hours for Mrs. MUKANKIKO and to do advocacy to the nutritionist and
social workers for they can ensure good nutrition.
1) What do you think as the risk factors of bedsores?
2) What do you think Mr. KWIZERA could do to prevent bedsores?
3) Basing on the Figure 15, classify Mrs. MUKANKIKO’s bedsore stage.2.4.1. Definition of bedsores
Bed sores also called pressures ulcers or decubitus sores are lesions caused by
unrelieved pressure, including shearing and friction forces. Bed sores are a big
problem in hospital settings. Bed sores are due to localized deficiency of blood
supply to the tissues. The tissue is compressed between two surfaces, usually the
surface of the bed and the bony skeleton. When blood cannot reach the tissue, cells
are deprived of oxygen and nutrients, waste products of metabolism accumulate in
the cells and the tissue consequently dies.2.4.2. Risk factors of bed sores
Immobility that leads to unrelieved pressure to the skin over a bony prominence
is the most factor in development of pressure ulcers. Individual risk factors for
pressure ulcers may be categorized as extrinsic or intrinsic. Extrinsic factors are
external conditions in the immediate environment that place a vulnerable individual
at risk such as Friction and shearing, force (pressure) and moisture. Intrinsic factors
are conditions and comorbidities peculiar to the individual that confer risk such
as: immobility and inactivity, inadequate nutrition, fecal and urinal incontinence,
decreased mental status, diminished sensation, excessive body heat, advanced
age and certain chronic condition (Diabetes). Below are detailed risk factors• Friction and shearing force: Friction is a force acting parallel to the skin
surface. (Sheets rubbing against skin create friction).Friction can abrade the
skin, remove the superficial layers, and make it more prone to breakdown.
Shearing is a combination of pressure and friction. They damage blood
vessels and tissue area.• Immobility: refers to reduction in the amount and control of movement.
Normally people move when they experience discomfort due to pressure on
an area of the body. However decreased activity, extreme weakness, pain
or any cause of decreased activity can hinder person’s ability to change
positions independently and relieve the pressure, even if the person can
perceive pressure.• Inadequate nutrition: Prolonged inadequate nutrition causes weight loss,
muscle atrophy and loss of subcutaneous tissue. These three reduce the
amount of padding between the skin and bones, thus increasing the risk of
pressure ulcer development. Inadequate intake of protein, carbohydrates,
fluids, zinc and vitamin C contributes to pressure ulcer formation.• Fecal and urinary incontinence: Moisture from incontinence promotes
skin maceration (tissue softened by prolonged wetting or soaking), making
the epidermis more easily eroded and susceptible to injury. Digestive
enzymes in feces, gastric tube drainage and urea in urines also contribute
to skin excoriation. Any accumulation secretion or excretions irritate the skin,
harbours microorganisms and makes an individual prone to skin breakdown
and infection.• Decreased mental status: Individuals with decrease level of awareness are
at risk because they are less able to recognize and respond to pain associated
with prolonged pressure.• Diminished sensation: Loss of sensation reduces a person’s ability to
respond to trauma, to injurious heat and cold and to the tingling (pins and
needles).
Fundamental of Nursing | Associate Nursing Program | Senior 476• Excessive body heat: An elevated body temperature increases the
metabolic rate, thus increasing cellular need for oxygen. This increased need
is particularly severe in cells of an area under pressure, which are already
oxygen deficient. Severe infections with accompanying elevated body
temperature may affect the body’s ability to deal with the effects of tissue
compression.• Advanced age: ageing processes bring about several changes in skin and its
supporting structures, making the older person more prone to impaired skin
integrity. These changes are loss of lean body mass, generalized thinning
of the epidermis, decreased strength end elasticity, increased dryness,
diminished pain perception and diminished venous and arterial flow due to
ageing vascular walls.• Chronic medical conditions: Certain chronic conditions such as diabetes
and cardiovascular disease are risk factors for skin breakdown and delayed
healingAreas where bedsores occur
Bed sores mostly develop in areas where bones are close to the surface (bony
prominences) and areas that are under the high pressure. For People who uses
wheelchairs, bedsores occur on tailbone or buttocks, shoulder blades and spine,
backs of arms and legs where they rest against chair. For people who stay in bed,
bed sores develop on the back or sides of the head, the should blades, the hip,
lower back or tailbone, the heels, ankles and skin behind the knees.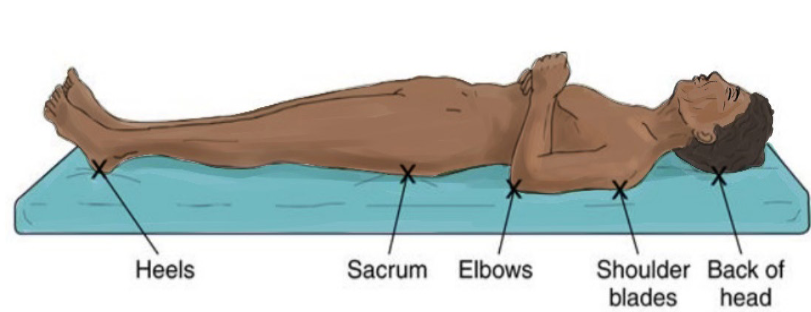
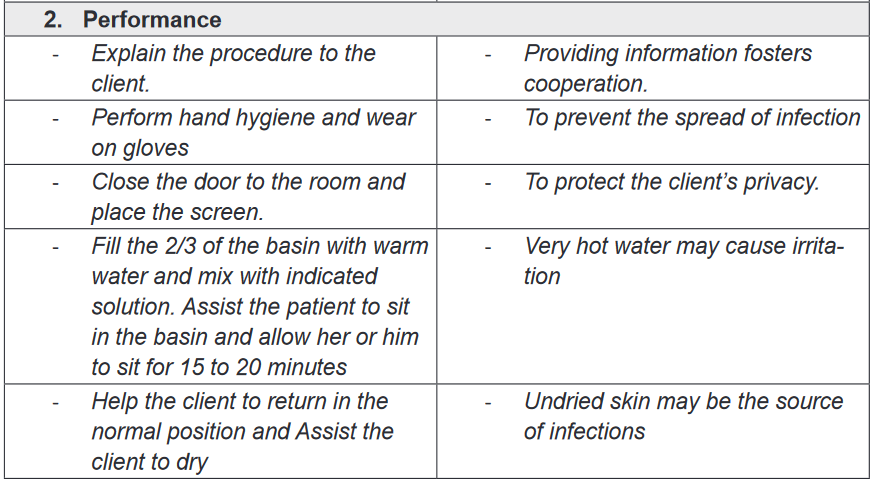
2.4.3. Stages of bed sores
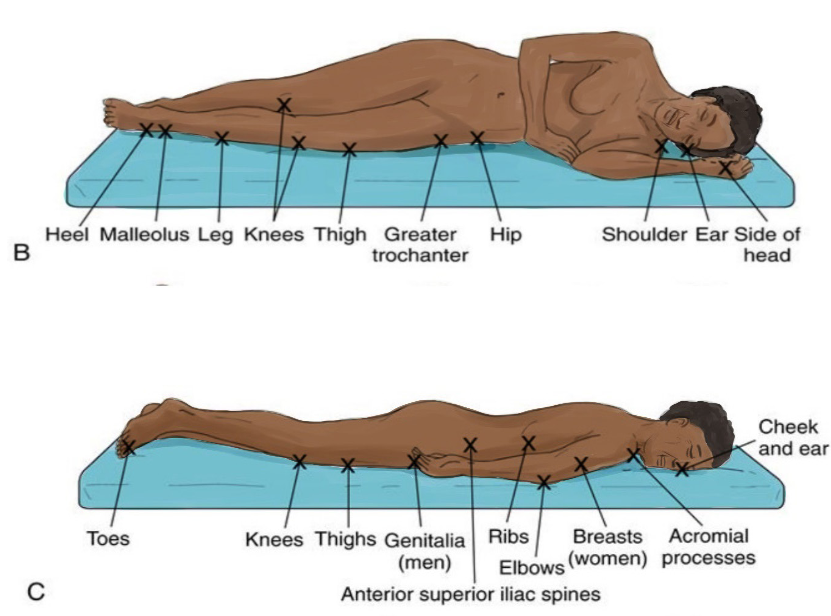
Bed sores have four clinical stages as shown s below in details:a) Staged 1-Pressure injury: Non blanchable erythema
This first stage is characterized by intact skin with non -blanchable redness of a
localized area usually over a bony prominence. In darkly pigmented skin may not
have visible blanching; its color may differ from the surrounding area. The area
may be painful, firm, soft, and warm or cool compared to adjacent tissue. It may be
difficult to detect in individuals with dark skin tones.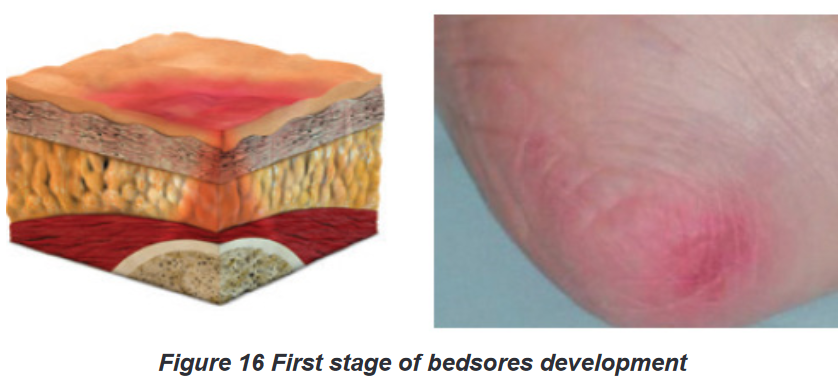
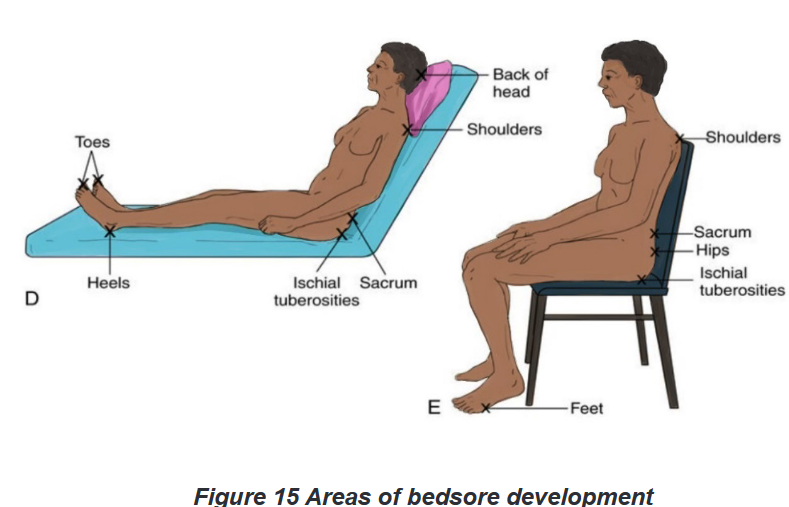
b) Stage 2- Pressure injury: partial thickness skin loss
The second stage is characterized by partial thickness loss of dermis presenting
as a shallow, open wound with a red-pink wound bed, without slough. May
also present as an intact or open/ruptured serum-filled blister. Presents as a shiny
or dry, shallow ulcer without slough or bruising.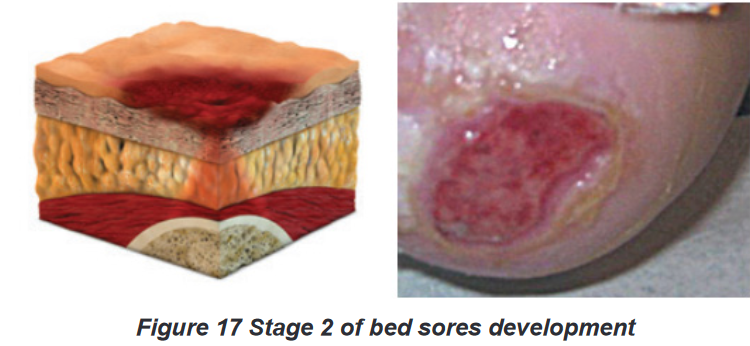
c) Stage 3-Pressure injury: full thickness skin loss
The third stage is characterized by full thickness tissue loss. Subcutaneous fat may
be visible but bone, tendon or muscles are not exposed. Slough may be present but
does not obscure the depth of tissue loss. May include undermining and tunneling.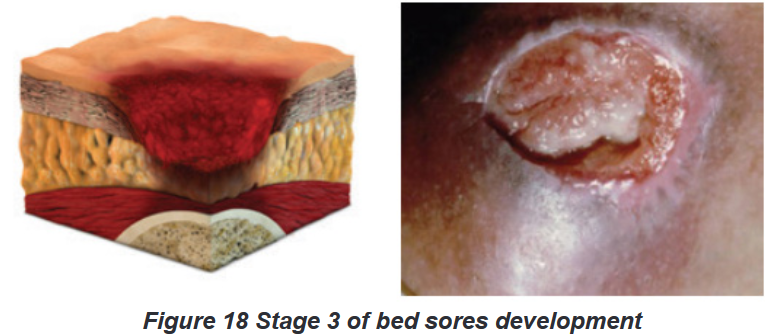
d) Stage 4- Pressure injury: full thickness tissue loss
The fourth stage is characterized by full thickness tissue loss with exposed bone,
tendon or muscle. Slough or eschar may be present on some parts of the wound bed.
2.4.4. Prevention and management of bedsores
Management of bed sores is complex; early identification of risk factors is key
to prevention and management of bed sores. Prevention of bedsores consist of
providing adequate body hygiene by keeping the skin clean and dry and keeping
the bed tidy and dry; turning and repositioning the client every two hours prevent
bedsores; and adequate nutrition with enough calories, vitamins, minerals, fluids
and protein help to prevent bedsores and accelerate healing process of sores.Management of the wound depend on the stage of bedsores; consist of wound
cleaning, removing the damaged, infected or dead tissue(debridement) and
transplanting healthy skin to the wound area (skin grafts). Administration of
antibiotics may be necessary to treat infection that may associated with bedsores.Self-assessment 2.4.
1) The most common areas where pressure ulcers occur are the
a) Hands and neck
b) Coccyx and neck
c) Sacrum and coccyx
d) Back of the head and hands2) In which of the following pressure injury stages is the skin still intact?
a) Stage 1
b) Stage 2
c) Stage 4
d) Stage 33) The following are risk factors of bed sores except:
a) Advanced age
b) Physical exercise
c) Poor Nutrition
d) Diabetes4) The pressure ulcers can be caused by
a) Wrinkled linen
b) Soiled linen
c) Dragging the patient across linens
d) All the above5) Staging systems for pressure ulcers are based on the depth of tissue
destroyed. Briefly describe each stage.2.5. Moving and positioning patients in bed
Learning activity 2.5.1.
Look at the following table that describe different positions that a person may
(be assisted to) take depending on her or his status and condition and attempt
the questions which follow it.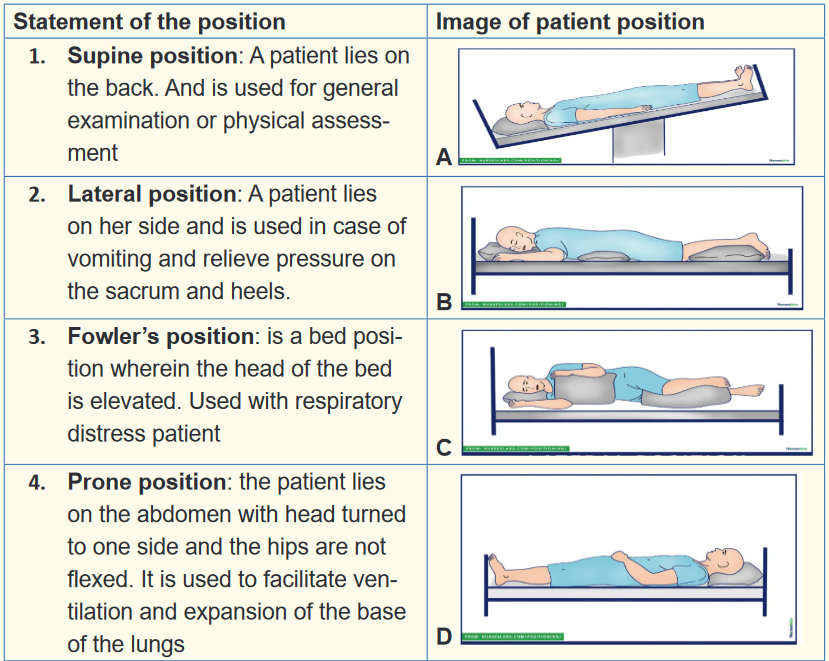
1) Match each statement with its corresponding image
2) After sustaining a road traffic accident, Mr. RUKUNDO has bled heavily.
Which appropriate position for Mr. RUKUNDO and why?
3) Mrs. MUGWANEZA was lying on her back position and you noticed that
she is vomiting. What is the suitable position to her?Learning activity 2.5.2.
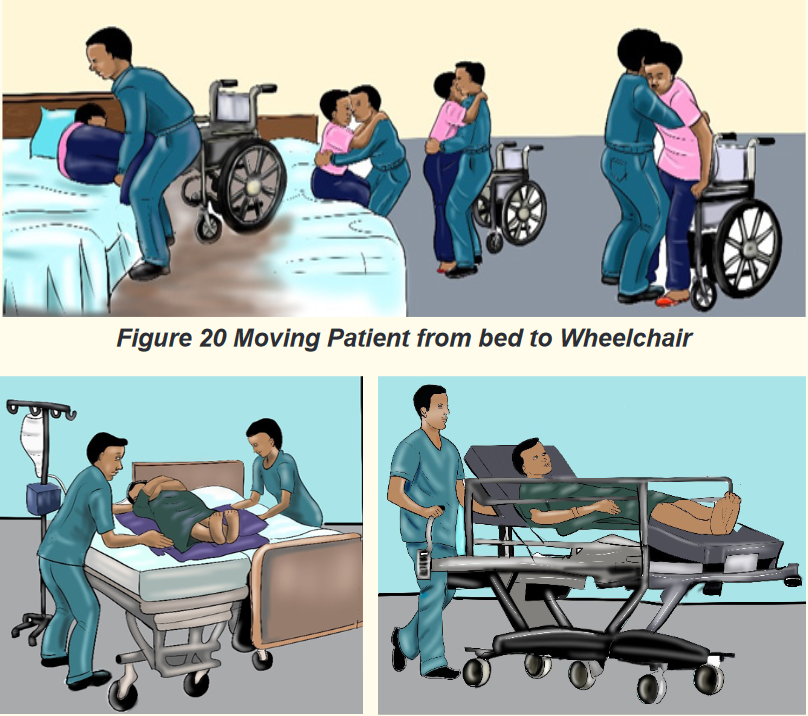
Figure 21 Moving patient from bed to stretcher (a stretcher is a device
used to carry a person who must lie flat and can’t move on their own)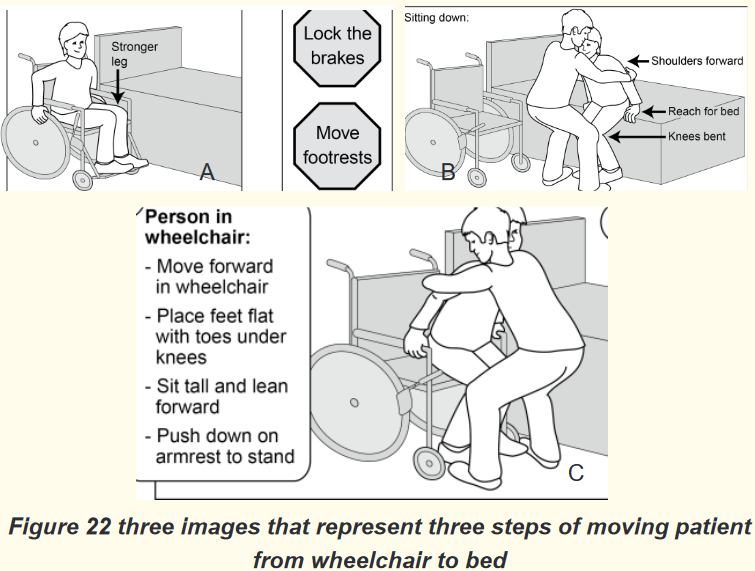
1) Look at the Figures 20, 21 &22 and think about the purpose of moving
patient from bed to wheelchair
2) From the Figure 21, what do you think is the purpose of moving
patient from bed to stretcher
3) Observe the Figure 22 and provide the chronological order of steps.
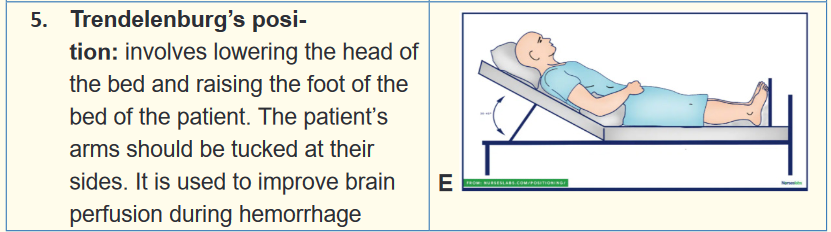
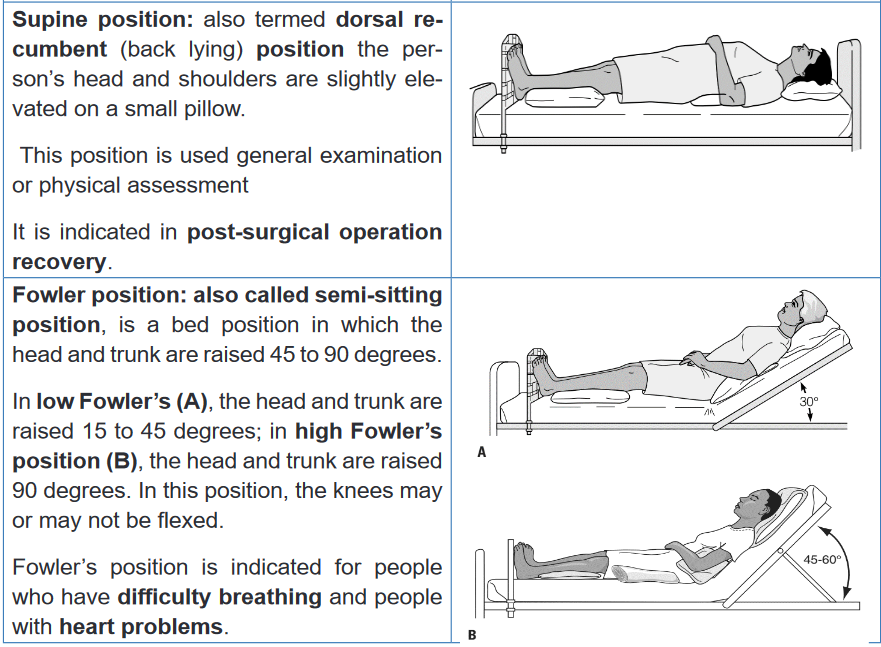
Think about how these persons will use their muscle during the move.2.5.1. Positioning patients
a) Patient positions
Patients with impaired nervous, skeletal or muscular system functioning
and increased weakness and fatigue often require assistance from nurses for
positioning while in bed or sitting and for moving. Positioning a patient in good
body alignment and changing position carefully and systematically are essential
aspect of nursing practice.Any position, correct or incorrect, can be detrimental if maintained for a prolonged
period of time. Frequent changes of position help to prevent muscle discomfort,
undue pressure resulting in pressure injuries, damage to superficial nerves and
blood vessels and contractures. Position changes also maintain muscle tone and
stimulate postural reflexes.Positioning materials and aids are available but sometimes can be made from
the available ones. Pillows, are used to protect bony prominences. Trochanter
roll, prevent external rotation when lining in supine position. The trapeze bar, a
triangular device hanged on the bed that can be used by the patient whose upper
extremities functions well.When positioning ensure the following: Mattress should be firm and level yet
has enough give to fill in and support natural body curvatures; Bed should
be clean and dry (wrinkled or damp sheets increase the risk of pressure injuries
forming; that’s why bed making is important), support devices/aids according
to patient’s position (pillows and trochanter roll are examples), avoid placing
one body part directly on top of another body part (especially one with bony
prominences) because pressure can damage veins and causes thrombus formation;
ensure the 24-hour schedule of position changes, frequent position changes
are essential to prevent pressure sores; and always obtain patient’s information
on which position is comfortable and appropriate.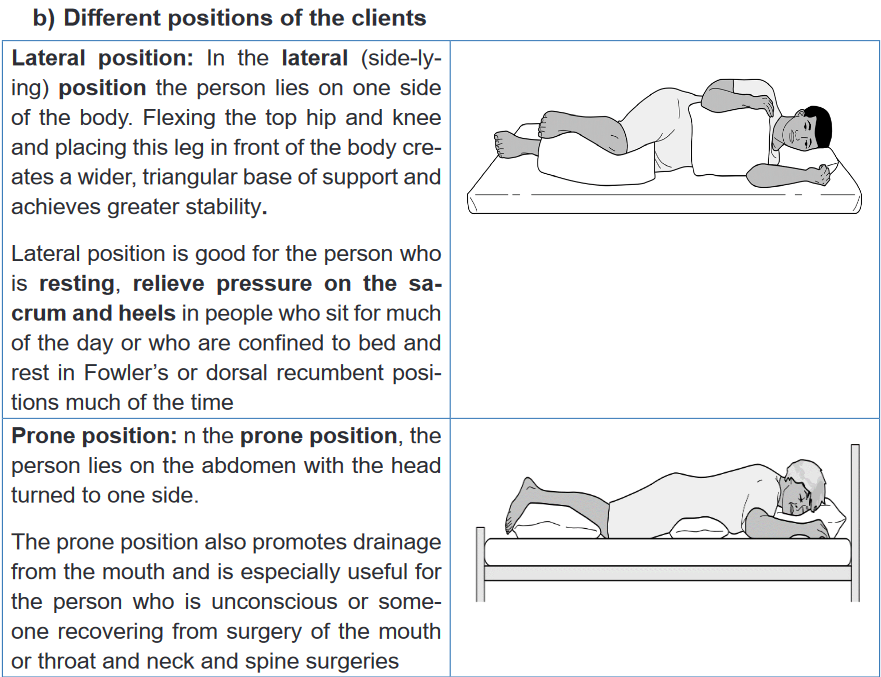
c) Principles of changing positions
Healthy people change position, with little effort, however ill people may have
difficulties of moving or changing positions even in bed. Nurses should be sensitive
to both the need of clients to function independently and their need for assistance
to move. Comfortable and correct body alignment should be maintained in order
to prevent undue stress on the musculoskeletal system. When turning the
client, nurse should ensure the appropriate number of staffs and assisting materials
needed.When positioning patient, there are couple octions and ratonales which are
applicaple to moving and lifting:• Before moving a client, assess the client’s physical abilities, and ability
to assit with the move, degree of comfort, client’s weight, orthostatic
hypotension and your strength and ability.
• Prepare assitive materials available (e.g: pillows, trochanter roll);
• Plan around incumbrances to movement (e.g: IV, Urinary catheter, cast);
• Be aware of medications effects (e.g: effect on alertness, balance, strenth
and mobility);
• Ensure assistance (if needed) from other people is available;
• Explain the procedure and listen suggestions from patient, or support
people have;
• Provide privacy;
• Perform hand hygiene;
• Raise the bed of the client to bring the client to your center of gravity;
• Lock the wheels on the bed and raiserails on the other side to ensure
client safety;
• Face the direction of the movement to prevent spinal twisting;
• Stand appropriately to increase the stability and provide balance;
Fundamental of Nursing | Associate Nursing Program | Senior 4 87
• Lean your trunk forward and flex you hips, knees and ankles to lower
your center of graity, ensure stability and ensure use of large muscle groups
during movements;
• Tighten your gluteal, abdominal, leg and arm muscle to prepare them for
action and prevent injury;
• Rock from the front leg to the back leg when pulling or from the back leg
to the front leg when pushing to overcome inertia counteracy the client’s
weight and help attain a balanced smooth motion;
• After moving determine and document the client’s comfort, body
alignment tolerance of the activity (check pulse rate, blood pressure),
abilty to assit and understand and safety precautions required.d) Techniques of changing position of the patient
i. Turning client to the lateral or prone position in bed
Purpose: the lateral positioning maybe needed when placing a bed pan, changing
bed linen or repositioning the client.
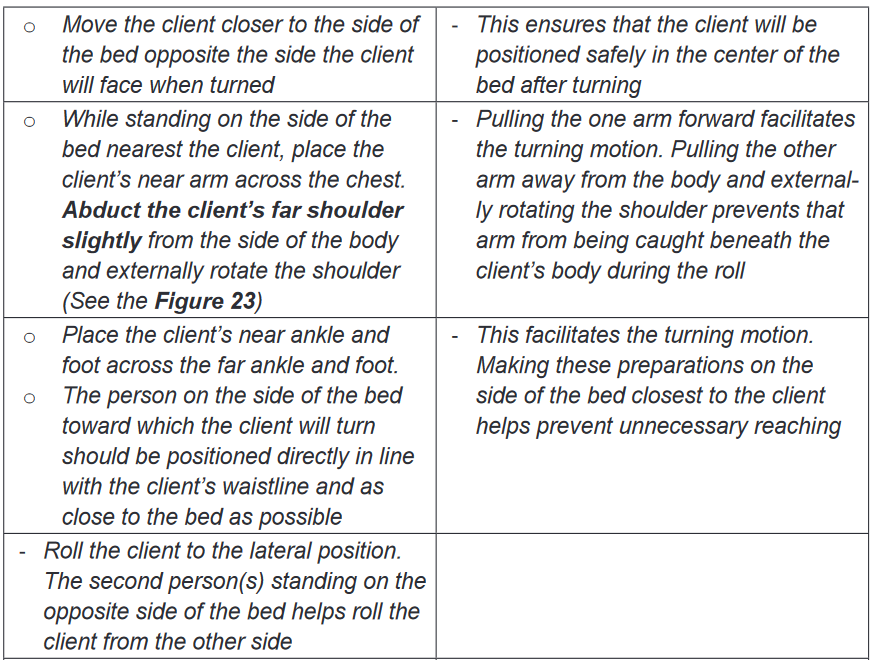
ii. Logrolling a client
Purpose: the purpose it to turn the client whose body must at all times be kept in a
straight alignment. E.g. client with back surgery or spinal injury.
2.5.2. Moving the patient
a) Purpose of moving patient
Many clients may require some help in transferring between bed and chair or
wheelchair, wheelchair and the toilet, and from bed to stretcher (mostly with
clients who cannot sit on wheelchair. Whenever the client is able to move him/
herself from bed to chair, wheelchair or stretcher encourage him to do so and
provide the required and appropriate assistance.b) Techniques of moving the patient
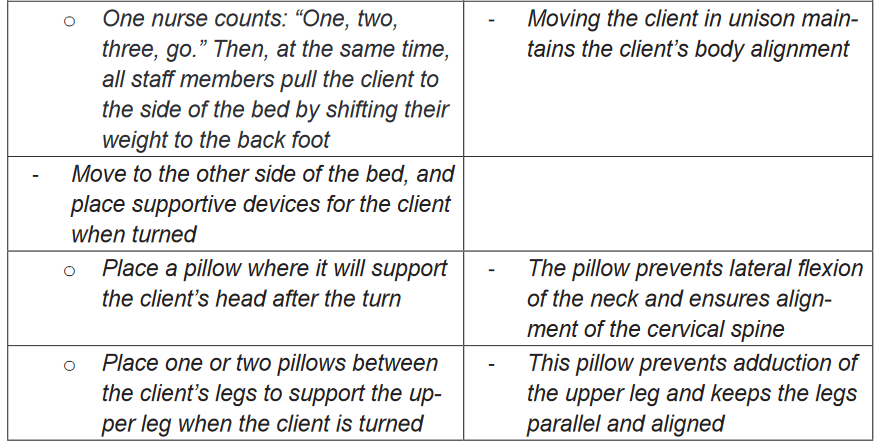
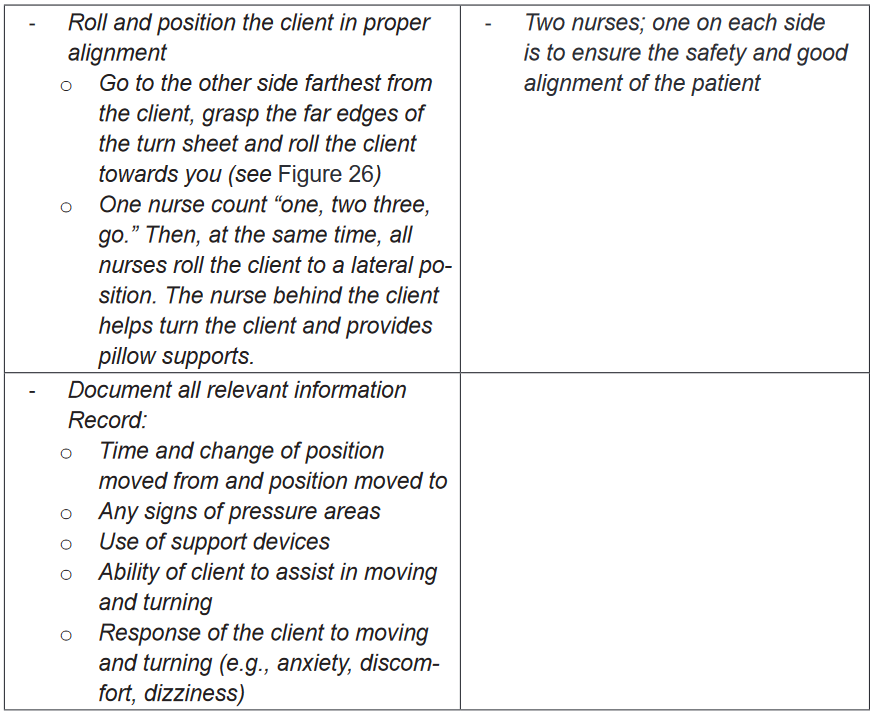
i. Moving patient in bed (two nurses using turn sheet)
Purpose: To assist clients who have slid down in bed from the Fowler’s position to
move up in bed.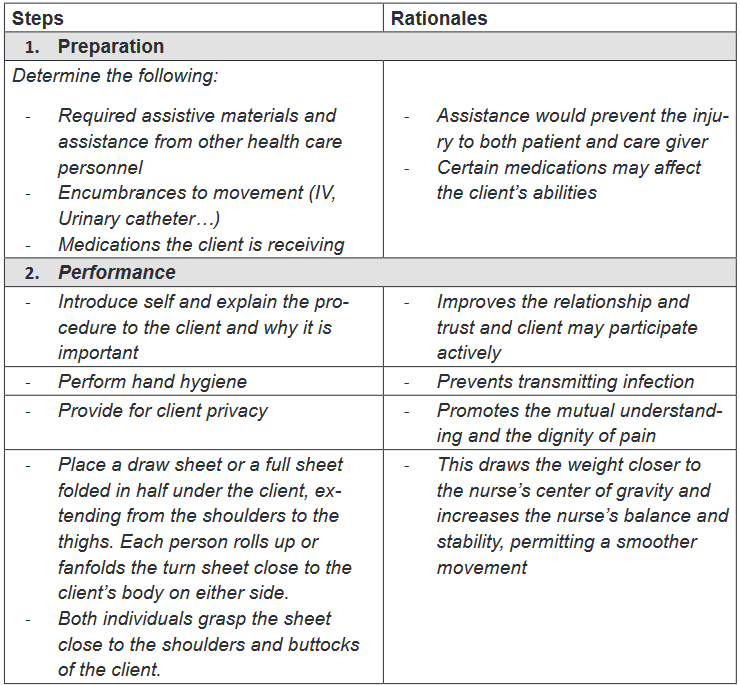
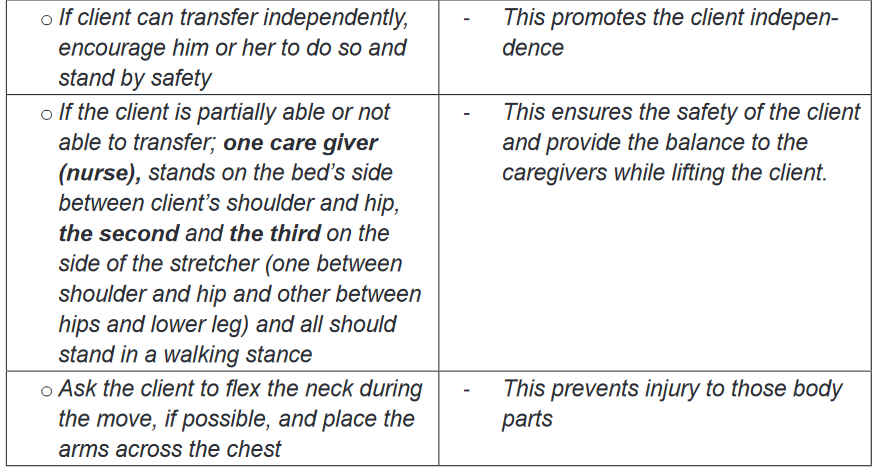
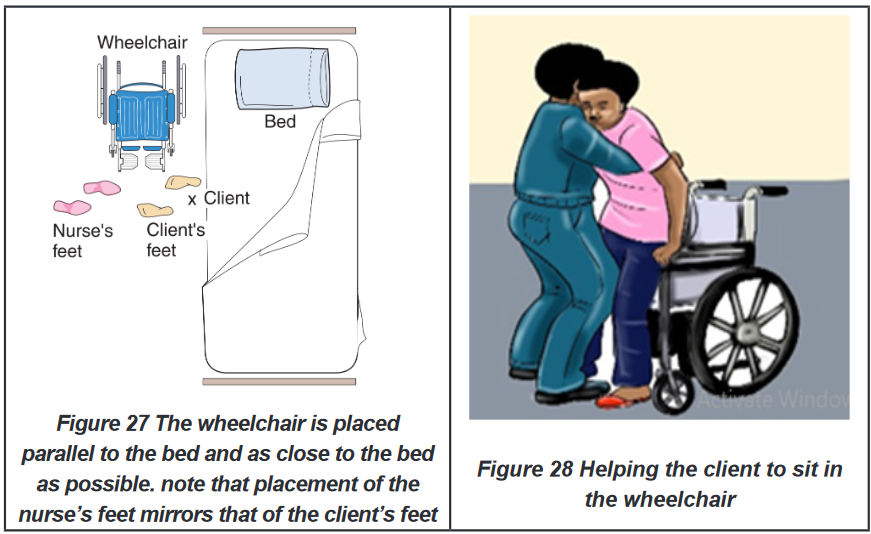
ii. Moving the patient from bed to chair or wheel chair (one nurse and two
nurses)
Purpose: clients who cannot move by themselves but can sit may need to be
transferred from bed to chair, or wheelchair due to different purpose: changing
position, ambulation, or transfer to operating room.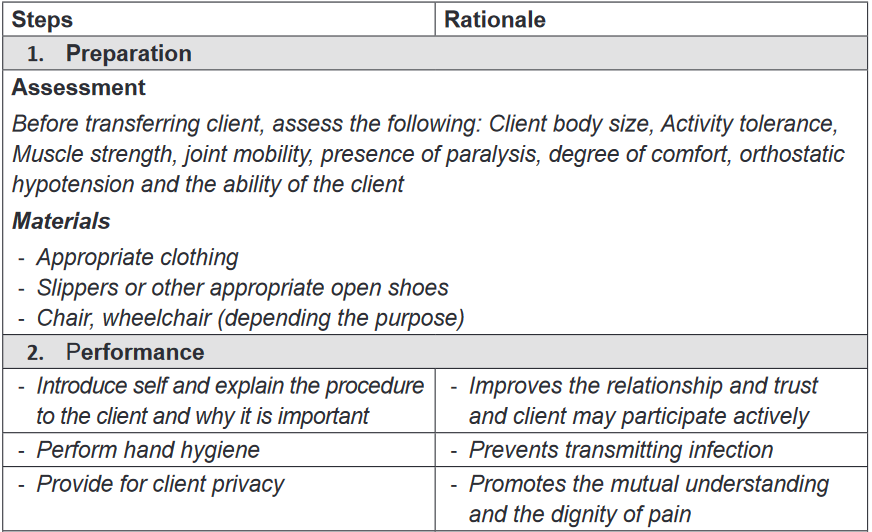
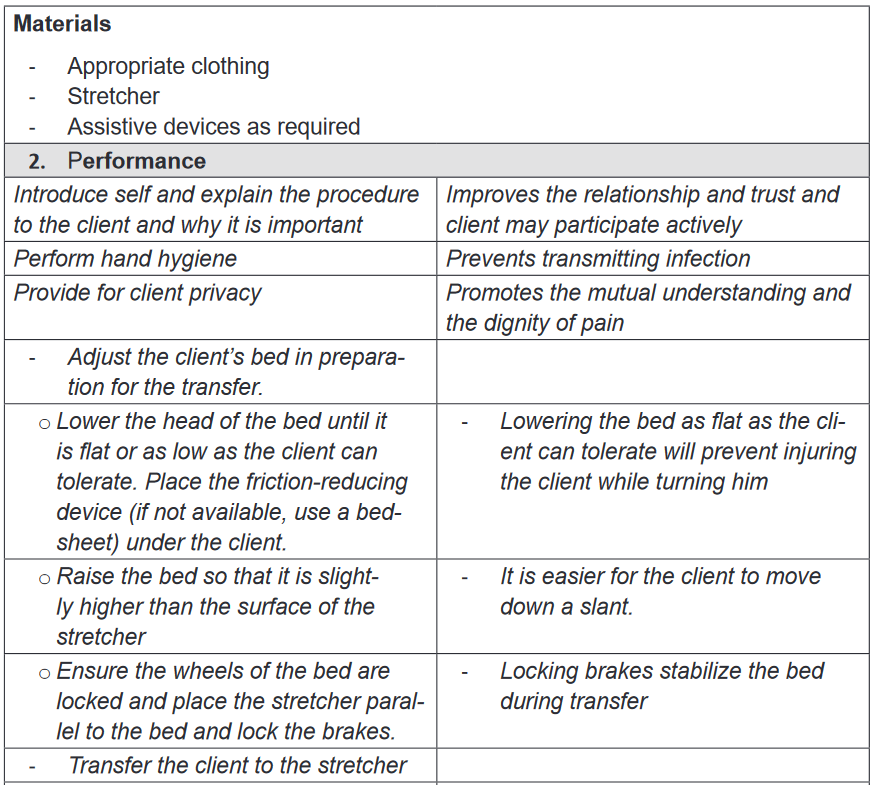
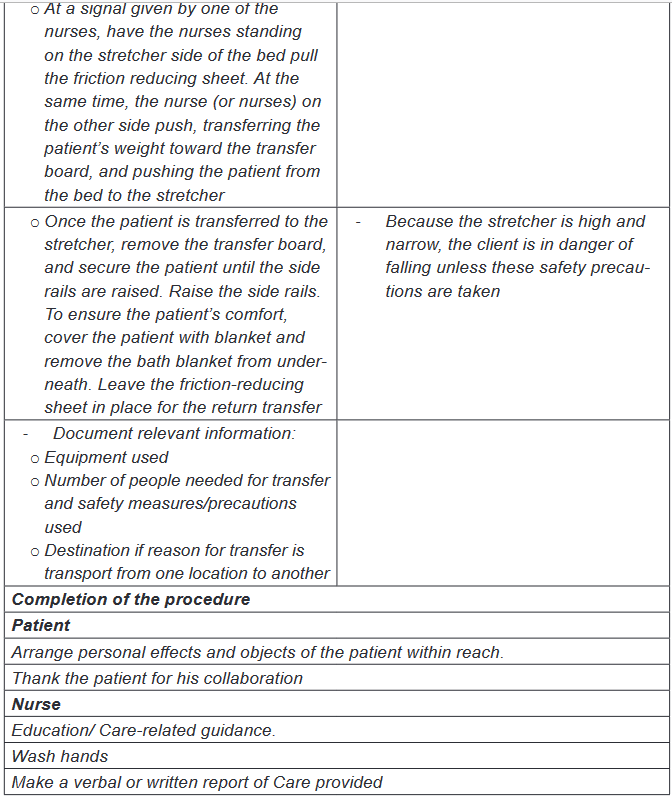
iii. Moving the client from bed to stretcher
Purpose: the stretcher is used to transfer the client in supine position from one
location to another (post-operated patients, patient with spinal injuries etc.)
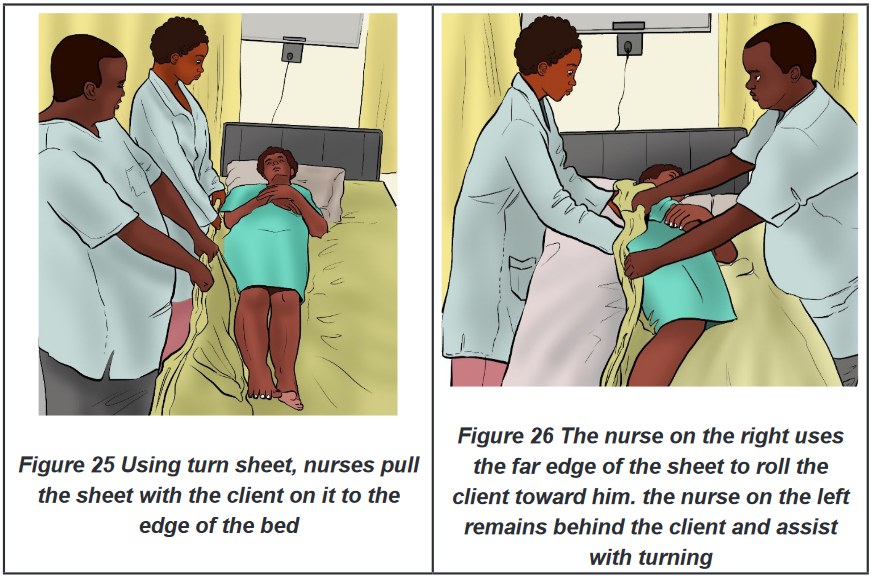
BOX 2.5.
Positioning, moving, and transferring clients reduce the potential for disuse
syndrome. Disuse syndrome is a term for the physical decline and other
problems that arise when the human body is deprived of physical activity.Self-assessment 2.5.
Mr. MUNYAKAYANZA, is hospitalized altered patient who is at risk of
developing bedsores, nurse decided to change position every two hours. Mr.
MUNYAKAYANZA is not breathing well, and his abdomen is distended.
1) What are the possible positions for Mr. MUNYAKAYANZA and explain
why?2) What are the contraindicated positions for Mr. MUNYAKAYANZA and
explain why?
After two weeks, Mr. MUNYAKAYANZA condition is being improved, he has
requested a nurse to help him for going outside on sunlight. However, he can
turn in the bed and sit but cannot walk.3) How a nurse will a nurse help Mr. MUNYAKAYANZA to move to the
sunlight and explain why?4) What are indications and contraindications of the chosen technique?
2.6. Application of local heat and cold
Learning activity 2.6.
Mr. NDAYISABA, an athletes who sustained a sprain (sprain: twist of the
ligaments of (an ankle, wrist, or other joint) violently that causes pain and
swelling) while running, the nurse AKAZUBA wanted to calm down the pain
and to prevent the progress of swelling by applying ice bags to the area. The
ice bag will cause vasoconstriction.
1) How do you think the vasoconstriction can lead to the reduction of
swelling?
2) What do you think are other alternatives to use in spite of ice bag?2.6.1. Definition of local heat and cold application
Heat application: is an application of warmed object, above body temperature, on
a body part to increase blood flow or provide relief of pain. While Cold application
refers to the placement of cold object cooler than skin, on the surface of the skin.
Heat and cold can be applied to the body in both dry and moist forms. Heat or cold
can be applied generally or locally. General application of heat or cold is used
when a very high or very low body temperature puts the patient’s health at risk or
makes the patient very uncomfortable. Local application of heat or cold is very
commonly used, and there are many different therapies. Common uses are to treat
sprains muscle pulls, arthritic joints, or local infections.2.6.2. Purpose of Local heat and cold application
Heat and cold stimuli create different physiological responses. The choice of heat
or cold therapy depends on local responses desired for wound healing as shown in
the below table.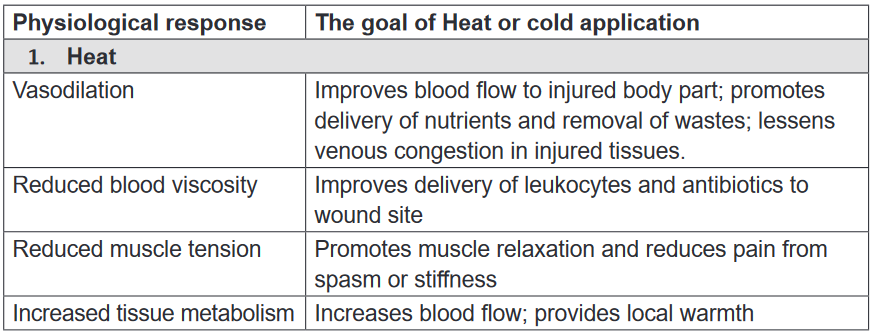
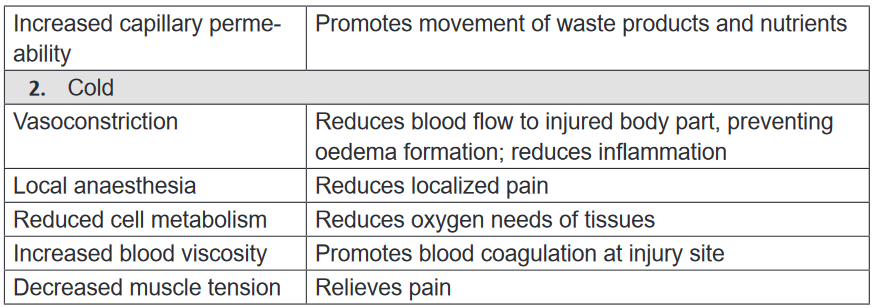
2.6.3. Principles of heat or cold applications
The following are principles of heat and cold applications:a) Heat application principles
• Measures the temperature of moist heat applications by putting at the back
of your palm.
• Do not apply very hot application, because it may cause burn
• Measure the patient temperature; Lower temperature is used for those at risk,
if it is too hot for the patient add cold water.
• Cover dry heat applications with cloth/ towel before applying them and be
sure that you are applying at the right location
• Do not let the person increase the temperature of the application.
• Carefully watch the time. Heat should not be applied for more than 30 minutes4
• Expose only the body part where the cold is to be applied.b) Cold application
• Measure the temperature of moist cold applications. It should not be freezing
cold
• Very cold applications can damage tissue
• Be sure about the exact location for the cold application
• Cover dry cold application with cotton or soft cloth before applying them.
• Carefully watch the time. Cold should not be applied for more than 30 minutes.
• Observe the skin for any problem, discontinue immediately if patient
experience: Pain, numbness or burning, Excessive redness, Blisters, Pale,
white or gray skin, Blue Patch and Shivering.2.6.4. Indication and contraindication of local heat and cold
application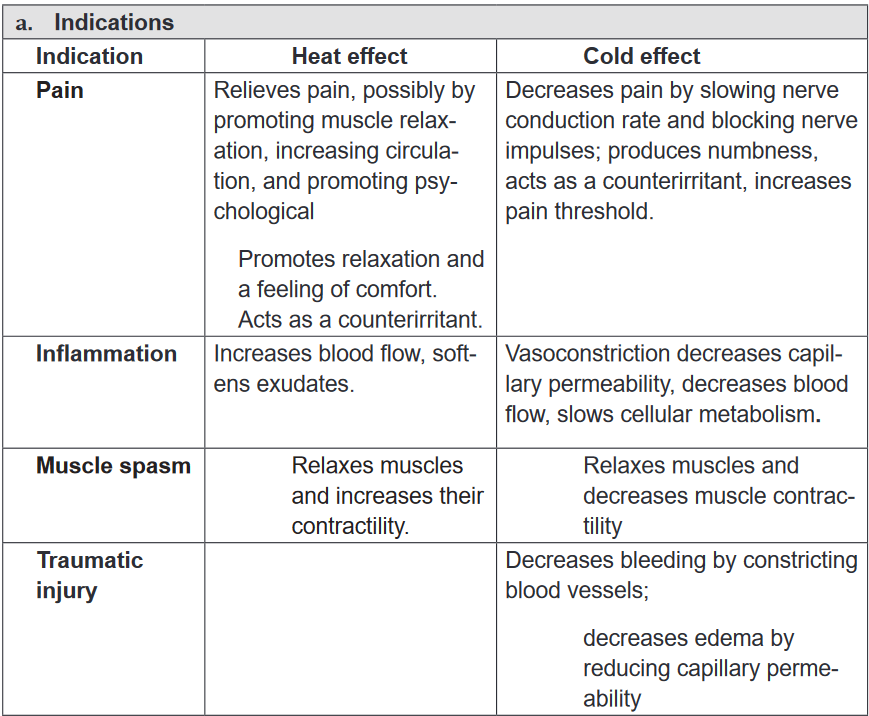
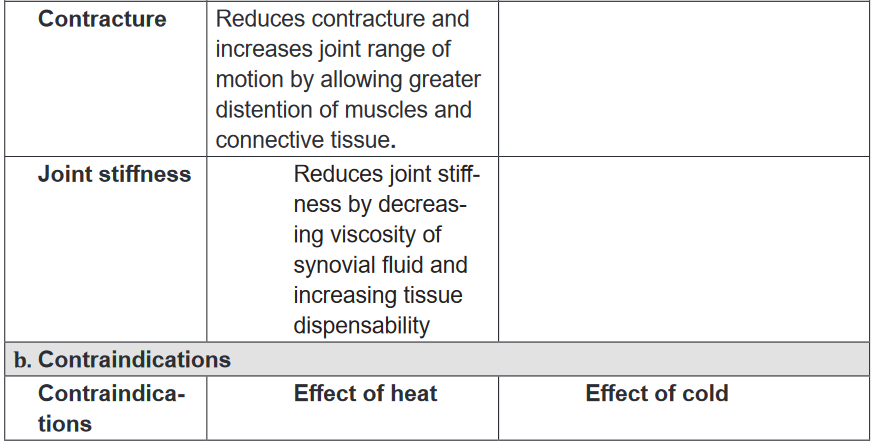
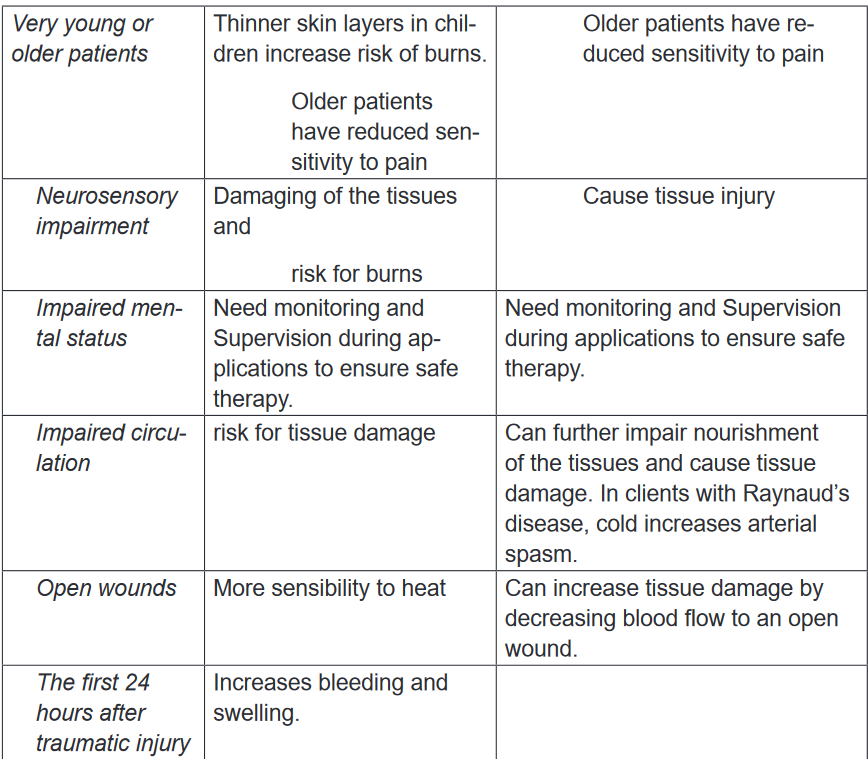
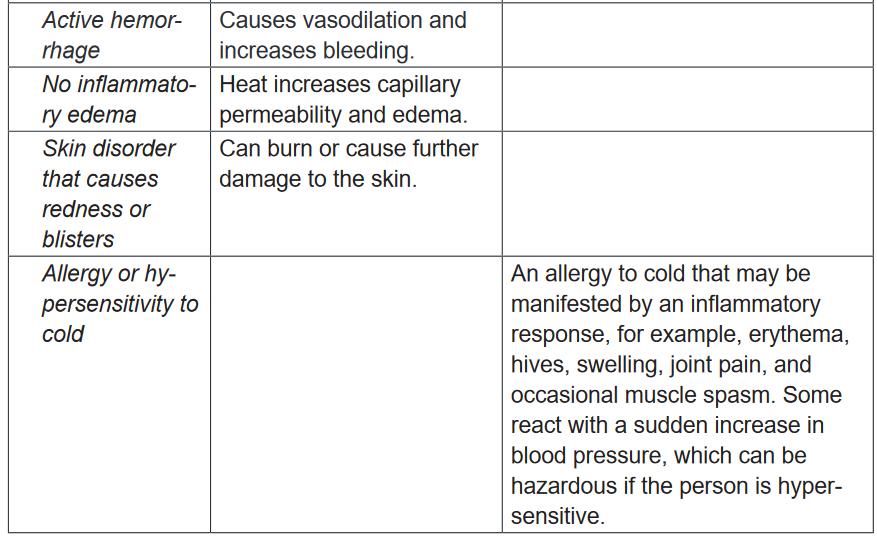
2.6.5. Techniques of local heat and cold application
Heat or cold should be applied after assessing the patient’s physical condition for
signs of potential intolerance to heat and cold. First observe the area to be treated.
Assess the skin, looking for any open areas such as alterations in skin integrity
(e.g., abrasions, open wounds, edema, bruising, and bleeding, or localized areas
of inflammation) that increase the patient’s risk of injury. The health care provider
commonly orders heat and cold applications for traumatized areas, the baseline
skin assessment provides a guide for evaluating skin changes that can occur
during therapy. Include in your assessment the neurological system for sensation
(to understand if the patient senses extremes of cold or heat) and the patient’s
mental status to be sure that he or she can correctly communicate any issues with
the hot or cold therapy.a) Heat application
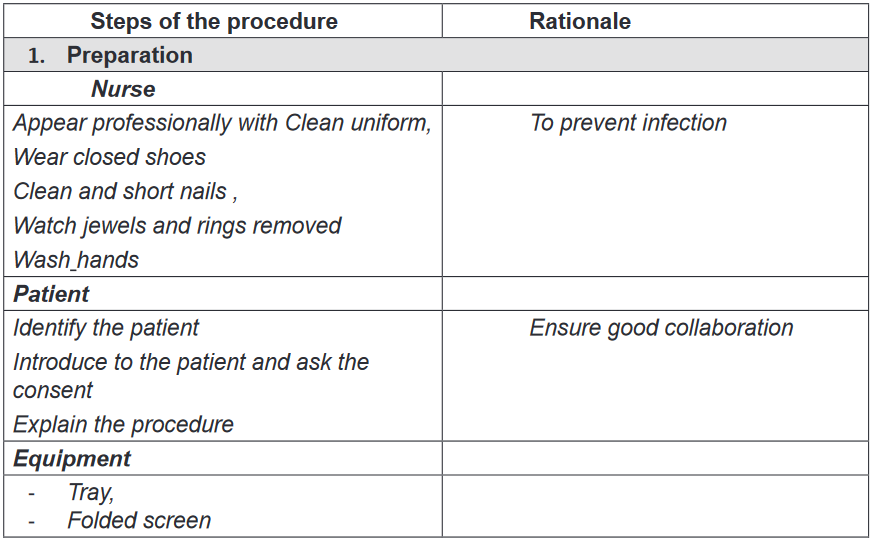
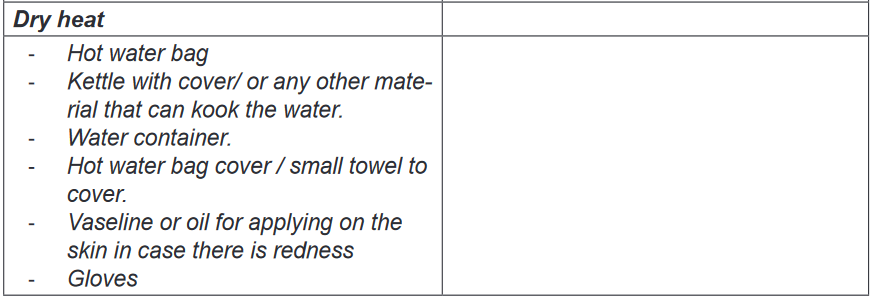
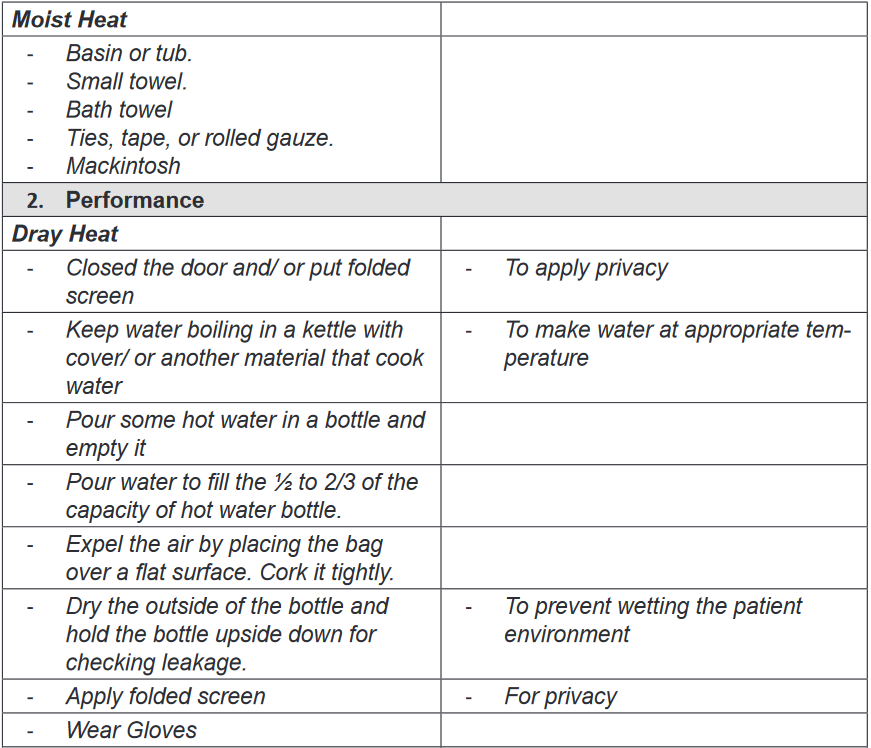
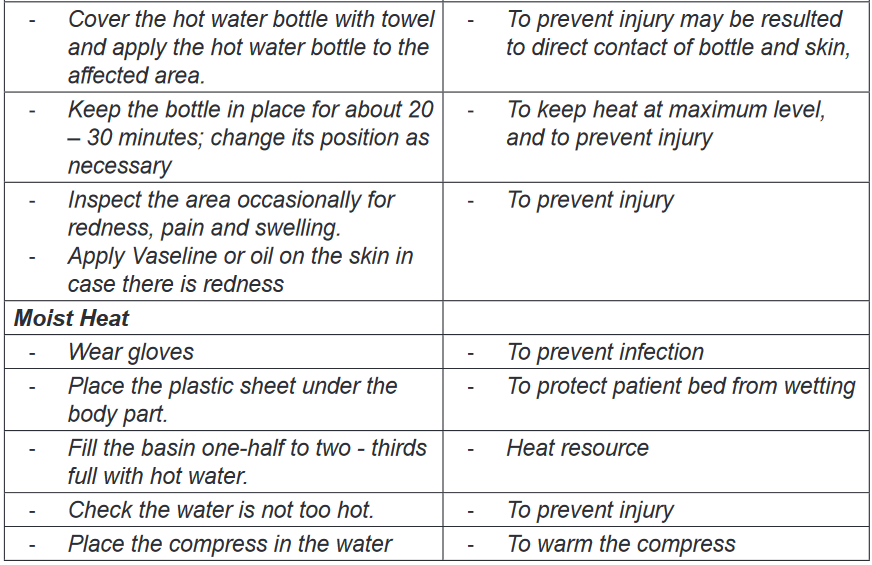
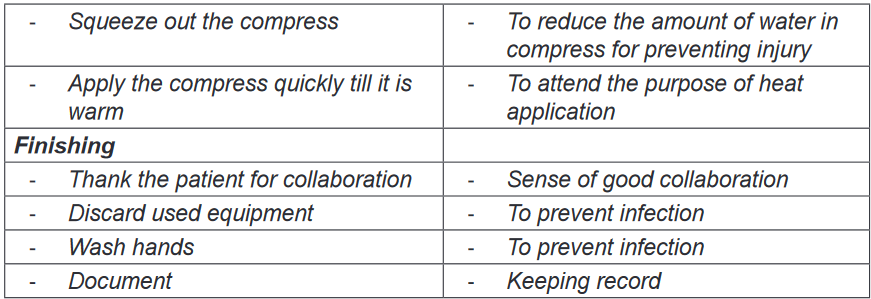
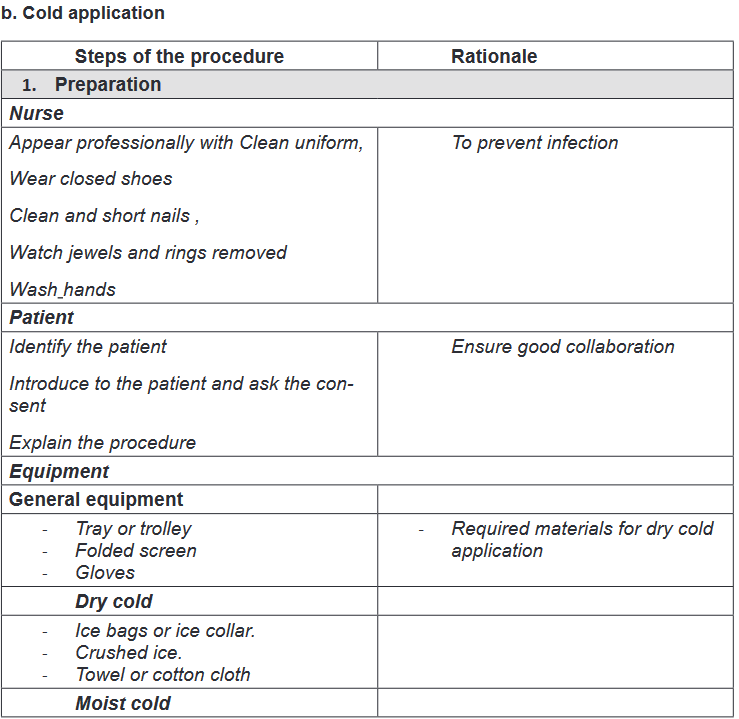
Self-assessment 2.6.
1) Explain the indications and contraindications of the heat application
2) Explain the relationship between the following terms
a) Vasoconstriction and swelling
b) Vasodilatation and inflammation2.7. Assisting the patient to eliminate
Learning activity 2.7
Regular elimination of body waste products is essential for normal body
functioning; the body eliminates its waste mainly through the urinary and the
gastro-intestinal systems. The metabolic reactions and other homoeostatic
processes lead to wastes which should be evacuated and if not eliminated,
they can alter the homeostasis lead to body malfunctions. Patients who are not
able eliminate independently or not able to control it (for example in case of
incontinence) should be assisted.
1) With reference to the above text and the knowledge from biology, explain
different ways of human body waste elimination
2) Think about possible consequences that may arise if the gastro-intestinal
system elimination is disturbed
3) Think about the patient with urinary incontinence, what could be possible
the consequences2.7.1. Introduction
a) Bowel elimination
The digestive system has many functions; ingestion, mastication, deglutition,
digestion, absorption and elimination. Elimination of the waste products of
digestion is the passage of fecal material that remains in the colon following the
digestion and absorption of nutrients and fluids which are required for maintenance
of metabolic health. The excreted waste products are referred to as faces or stool.
Normal feces are characterized by: brown color, soft formed consistency, tubular
shape as in the rectum, tolerable odor depending on diet and normal fecal content.
The normal bowel elimination frequency is 1-3 times a day to 3 times a week.Many factors affect defecation such as different stages of life (new-born, infant,
toddler, preschool children and adolescent adult and elder adult), Diet, fluid intake
and intolerance, physical activity and psychological factors such as anxiety and
depression. Physical disability, certain medications, gastrointestinal infection and
disease processes can also affect defection. Nurses are frequently involved in
assisting people with elimination problems. These problems can be embarrassing
to the individual and can cause considerable discomfort.Most problems of elimination are: Constipation which is defined as fewer than
three bowel movements per week. This infers the passage of dry, hard stool or the
passage of no stool. Fecal impaction is a mass or collection of hardened faces in
the rectum. Impaction results from prolonged retention and accumulation of fecal
material. Diarrhea is a problem of elimination that refers to the passage of liquid
faces and an increased frequency of defection.Encopresis also called fecal incontinence is an elimination problem that refers
to the loss of voluntary ability to control fecal and gaseous discharges through the
anal sphincter. Flatulence is an elimination problem that consist of presence of
excessive gas in the intestines and leads to stretching and inflation of the intestines
(intestinal distention) If excessive gas cannot be expelled through the anus, it may
be necessary to insert a rectal tube to remove it.b) Urinary Elimination
The urinary tract system is made of kidney, ureters, bladder and urethra; the pathway
trough which urine flows and is eliminated from the body. Urinary elimination depends
on the effective functioning of the upper and lower urinary tract. Micturition or
voiding, or urination refer to the process of emptying the urinary bladder. Urine
collects in the bladder until pressure stimulates special sensory nerve endings in
the bladder wall called stretch receptors.
Fundamental of Nursing | Associate Nursing Program | Senior 4110
They are many factors that affect the volume and characteristics of the urine
produced and the manner in which it is excreted such as: developmental
factors(infant, preschooler, school age children, adult, older adult), psychosocial
factors that stimulate micturition reflex includes privacy, normal position, sufficient
time, occasional running water. Fluids and food intake affect voiding. Other factors
that affect voiding are medication, muscle tone, pathological conditions that affect
urinary tract system and surgical and diagnostic procedures.Altered urine production is characterized by Polyuria which is the production of
abnormally large amounts of urines by kidneys, often several liters more than the
person’s usual daily output. Oliguria and Anuria are used to describe urinary output.
Oliguria is low urine output usually less than 500ml a day. Anuria refers to a lack
of urine production.
Altered urinary elimination is characterized by: urinary frequency that refers to
voiding at frequent intervals; that is more than six times per day. Nocturia is a
condition where a person wakes more than once during the night to void. Urgency
is the sudden strong desire to void. There may or may not by a great deal of urine
in the bladder, but person feels a need to void immediately.Dysuria is altered urinary elimination characterized by voiding that is either painful
or difficult. Enuresis is involuntary urination in children beyond age when voluntary
bladder control is normally acquires usual by 5 years of age. Urinary incontinence
is involuntary urination. Urinary retention is when emptying the bladder is impaired,
urines accumulates and the bladder becomes over distended.Neurogenic bladder is an altered urinary elimination characterized by impaired
neurological function that interfere with the normal mechanisms of urine elimination
resulting in lack of perceiving bladder fullness and inability to control urinary
sphincters. The bladder may become flaccid and distended, or spastic, with frequent
involuntary urination.2.7.2. Use of urinal
a) Indications and contraindications
In case patient cannot move of from the bed due to different conditions such as
lower limb fracture, or other conditions preventing him to move from the bed;
urinal, a device that help people to urinate while in bed, can be used to collect urine
while patient on bed. Urinals are indicated to people who have conscious control
of micturition and movement of their arms to urinate without the help of nurse.
However, it is contraindicated to people who are unconscious, not having control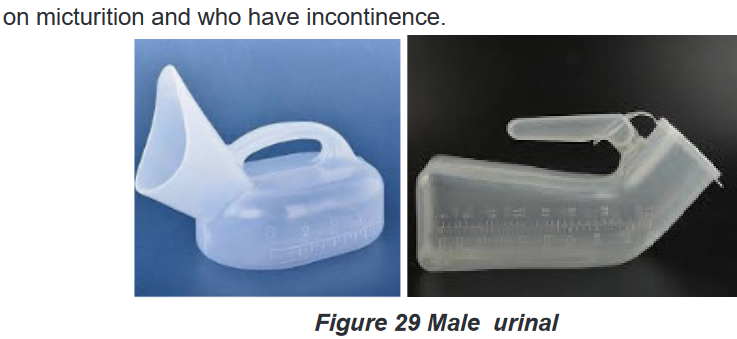
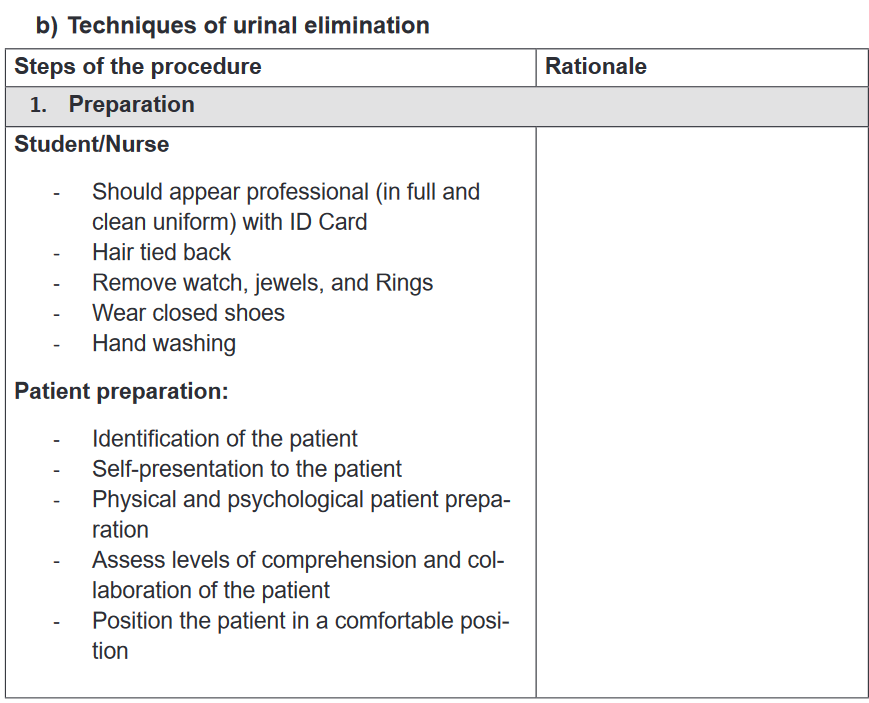
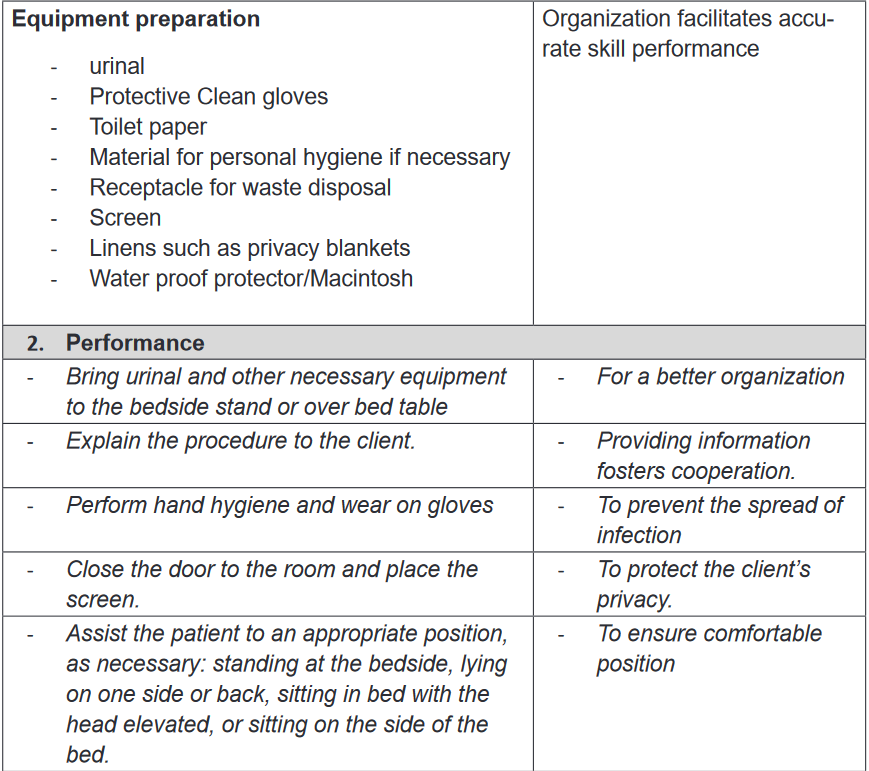
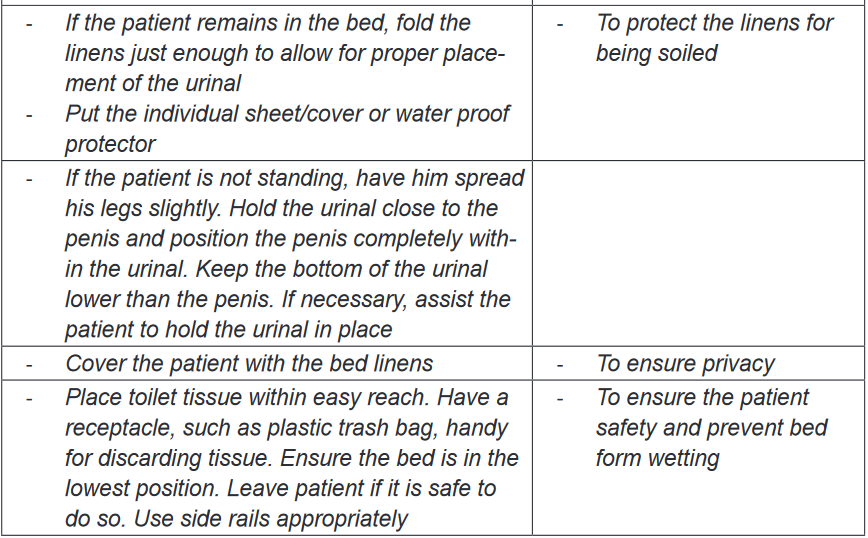
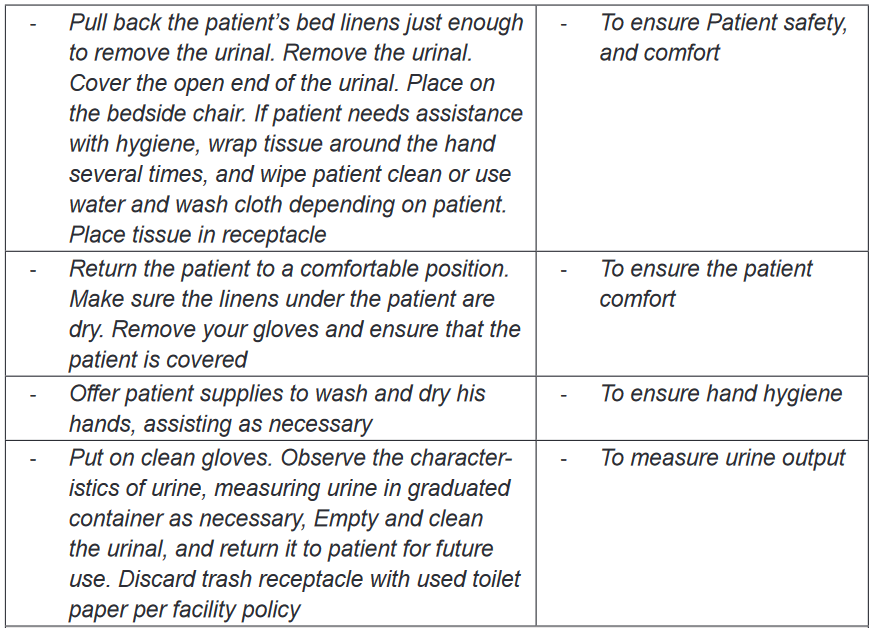
2.7.3. Use of bed pan
a) Definition of bed pan
A bed pan is a container used in hospital settings to assist bed ridden patient for
urination and defecation. A bed may be made in metal Stan steel or plastic material.
They are two different types of bed pans: regular and fracture.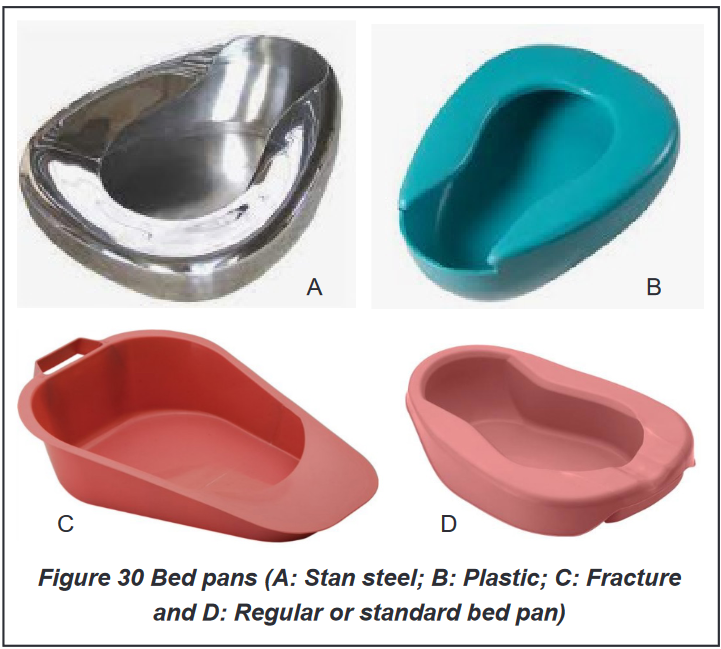
Indications of the bed pan use
Same as the urinal, bed pan can be used when client cannot walk to the bathroom;
patient with hip and lower extremity fracture, debilitating illness or profound fatigue,
high fall risk and increased injury potential, obstetrical and gynecological and patient
with fracture and patient who have had surgery that make them unable to move.
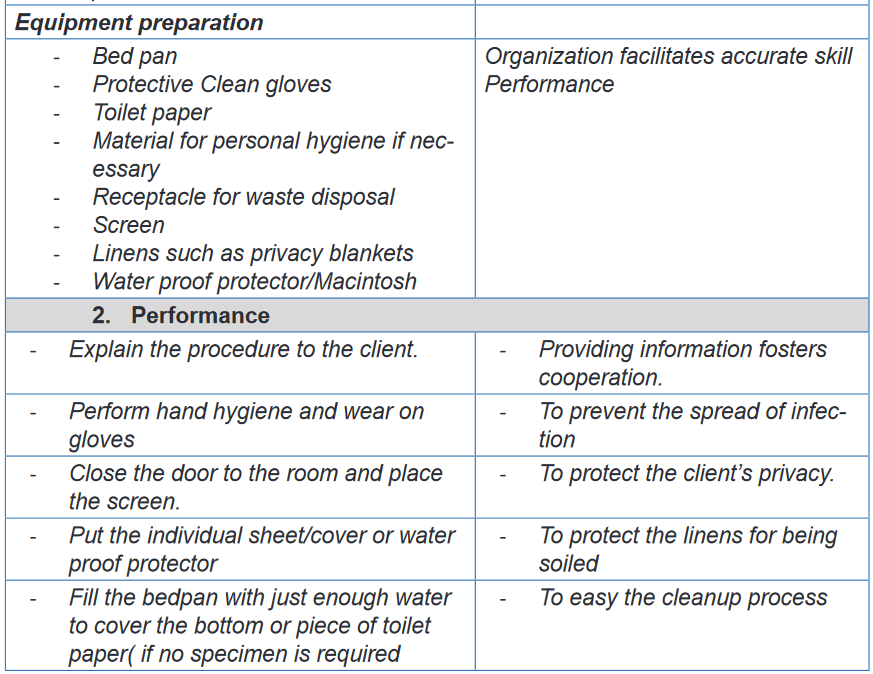
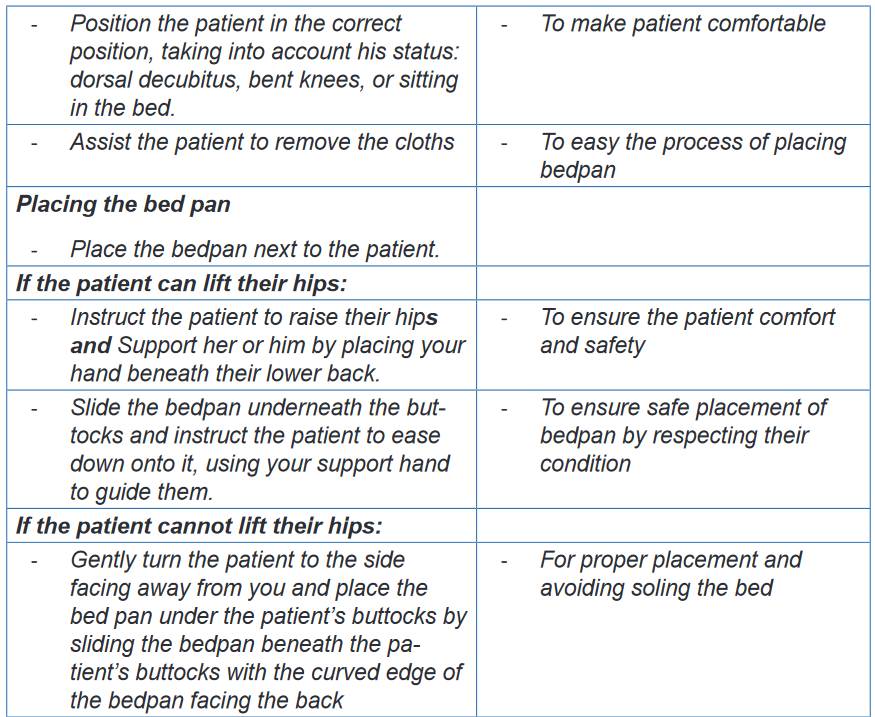
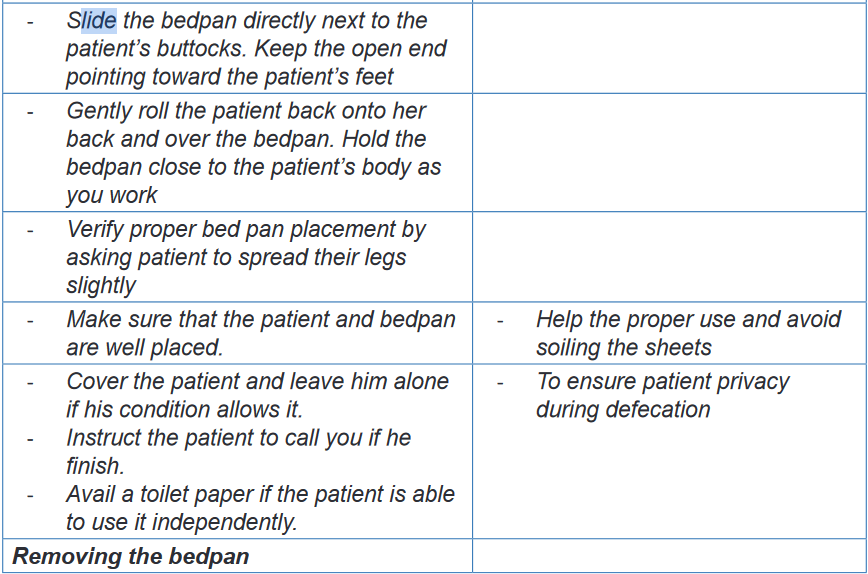
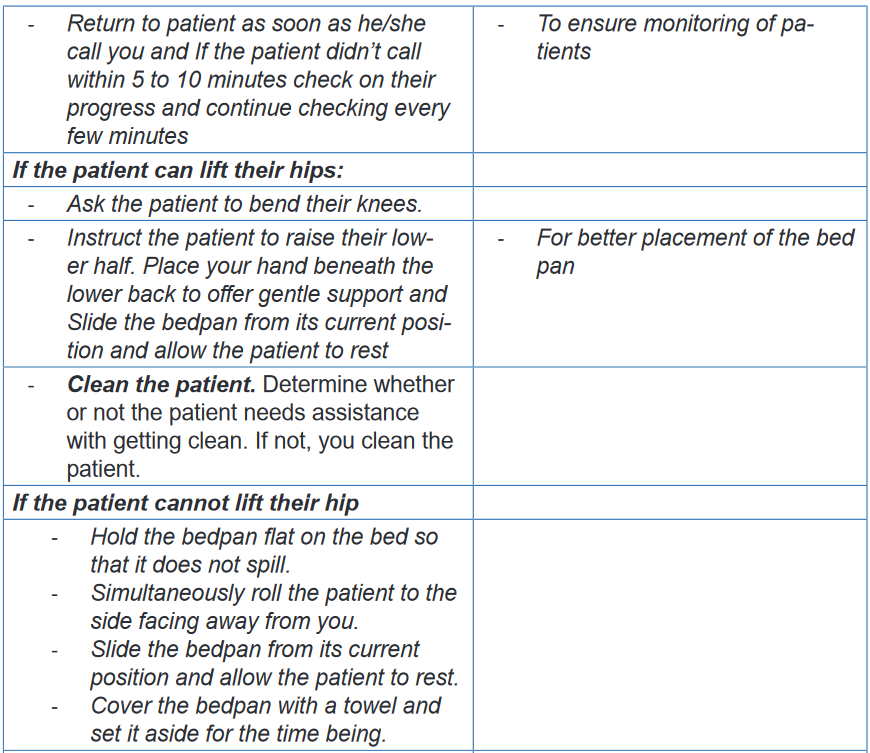
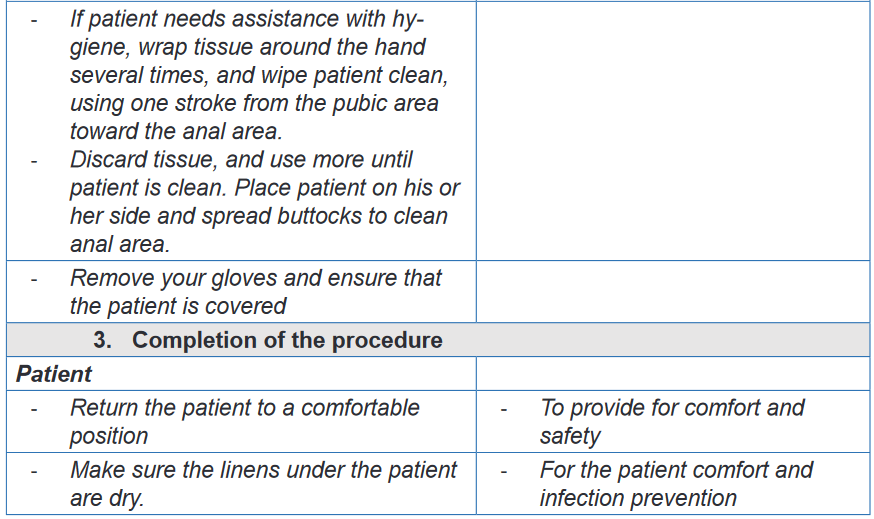
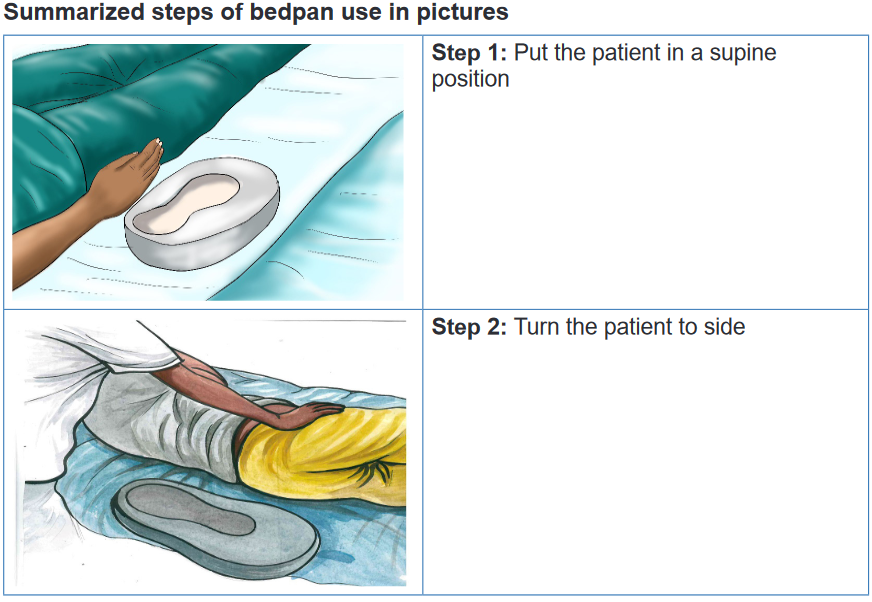
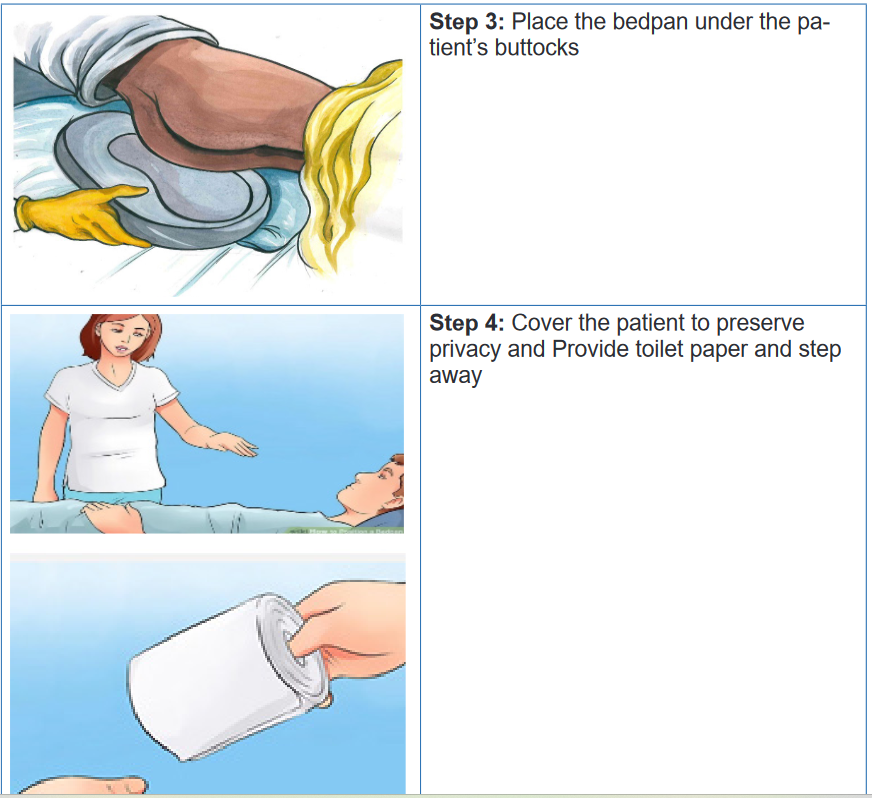
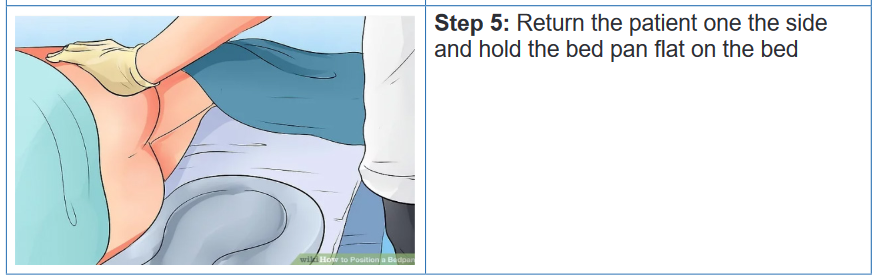
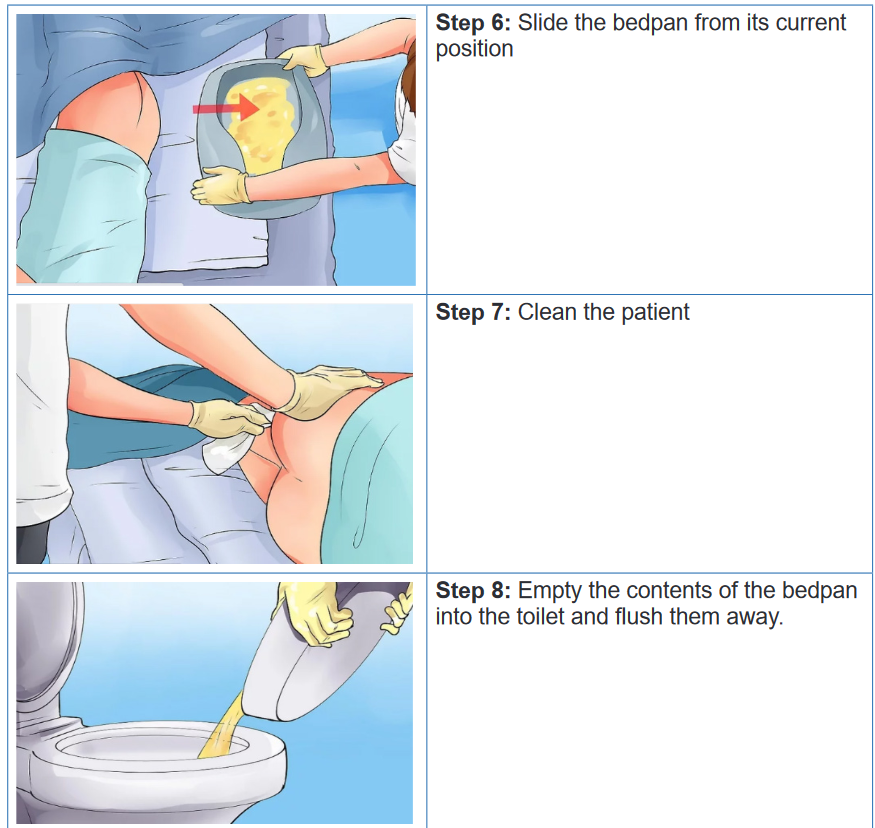
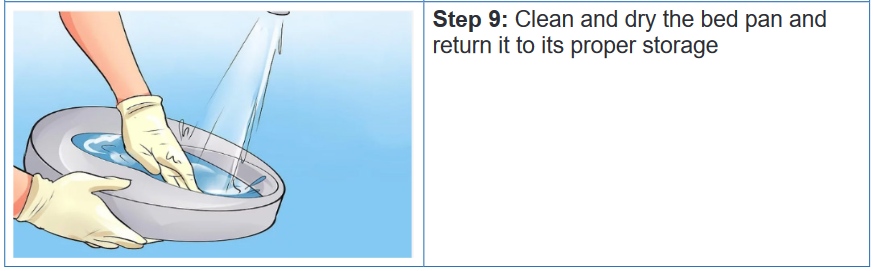
2.7.4. Enema
a) Definition and Types of enema
An enema is a a procedure in which liquid is injected into the rectum, to expel its
contents or to introduce drugs or permit X-ray imaging.. The purpose of an enema is to cleanse the lower bowel, to evacuate the stool
or flatus, or to instill medication. The enema solution should be at 37.7°C (100°F)
because a solution that is too cold or too hot is uncomfortable and causes cramping.
Enemas are classified into four groups: cleansing, carminative, retention, and
return-flow enemas.i. Cleansing enema
The goal of cleansing enemas is to remove feces. This type of enema is indicated in
case of constipation, patient preparation for surgery and some diagnostic test (i.e.,
colonoscopy). Normal saline is Isotonic considered as safe to use. Cleansing
enemas have two sub category: high or low. A high enema requires large volume
(i.e., 500 to 1,000 mL) for adult and is provided to cleanse as much as possible the
colon. The client changes the positions from the left lateral to the dorsal recumbent
and then to the right lateral position during administration so that the solution can
follow the large intestine. The low enema requires a small volume (90 to 120 mL)
and is used to clean the rectum and sigmoid colon only. The client maintains a left
lateral position during administration.ii. Carminative enema
A carminative enema is given mainly to expel flatus (intestinal gas). The solution
instilled into the rectum remove gas. For an adult, 60 to 80 mL of fluid is instillediii. Retention enema
A retention enema tends to introduce the oil or medication into the rectum and
sigmoid colon. The liquid is retained for a relatively long period for 1 to 3 hours. The
goal is to soften the faces, lubricate the rectum and anal canal, hence facilitating
passage of the fecesiv. Return-flow enemas
A return-flow enema, also called a Harris flush, is occasionally used to expel flatus.
Alternating flow of 100 to 200 mL of fluid into and out of the rectum and sigmoid
colon stimulates peristalsis. This process is repeated five or six times until the flatus
is removed and abdominal distention is relieved.
b) Indications and Contra-indications of enema
Enema is indicated to evacuate the bowel before surgery, X-ray or for bowel
examinations such as an endoscopy and to treat severe constipation. The enema
is contraindicated when phosphate or sodium is in high concentration in the blood,
or when calcium is low in the blood. Enema is also contraindicated in the following
condition: dehydration, anal cancer, Laceration or wounds on anus, Hemorrhoid,
Diarrhea, Intestinal occlusion or perforation and Appendicitisc) Complications of enema
A wrongly administered enema can damage tissue in the rectum/colon and
cause bowel perforation and, if the device is not well sterilized can cause the
infections. Long-term, regular use of enemas can cause electrolyte imbalances.
Other effect of enemas can include bloating and cramping.d) Administering enema (evacuating enema/return flow enema)
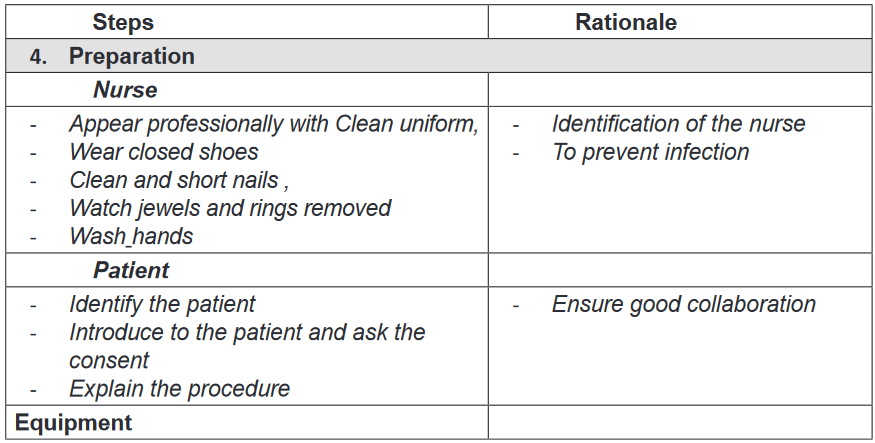
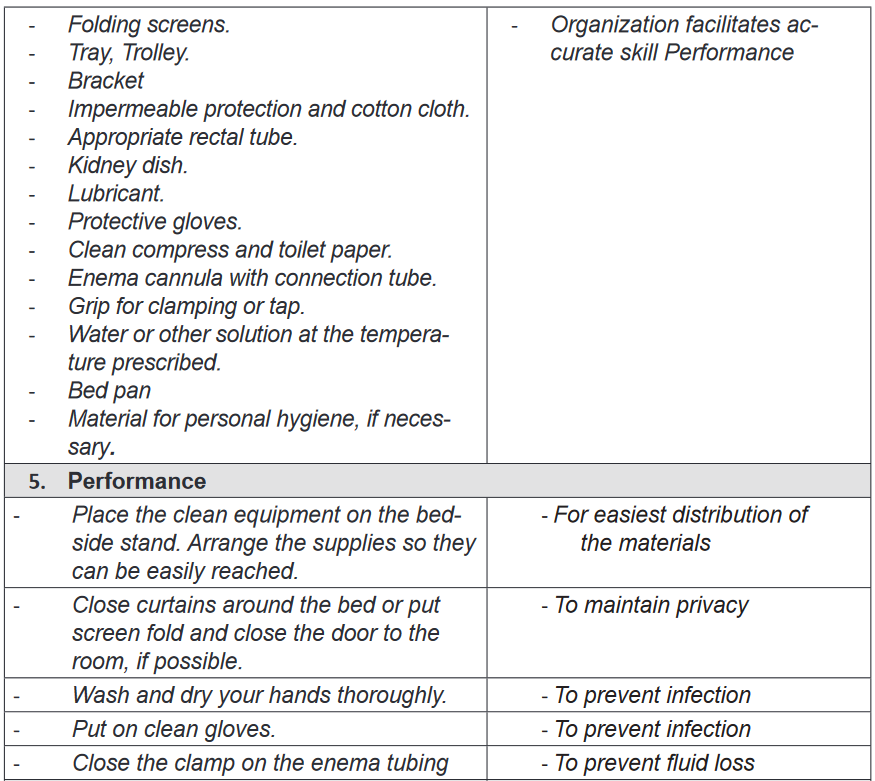
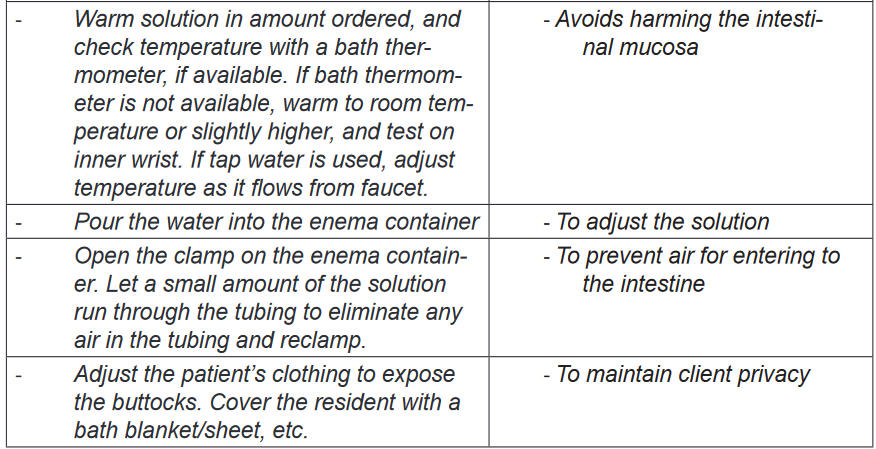
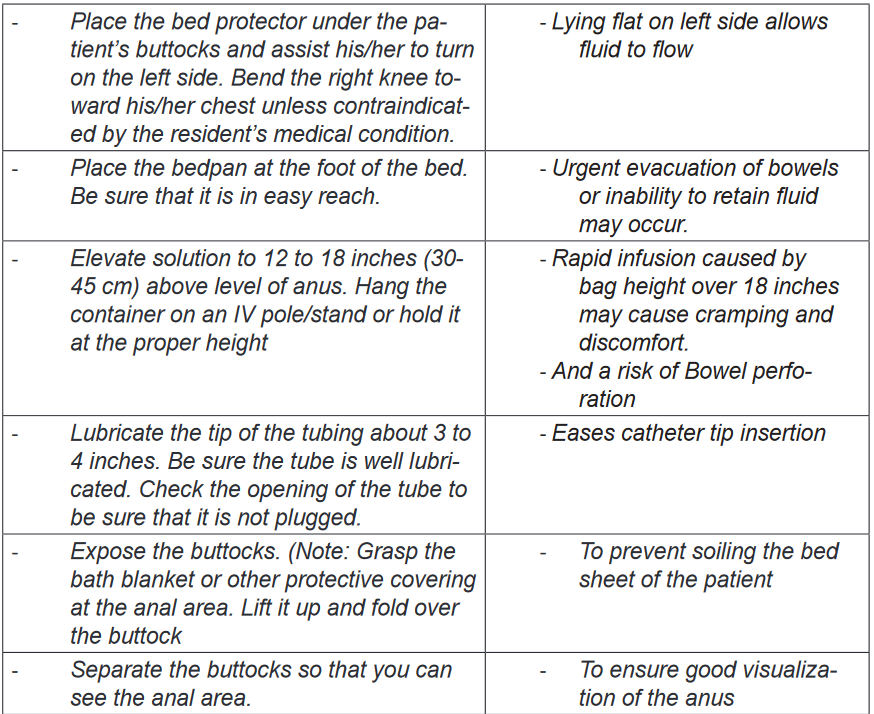
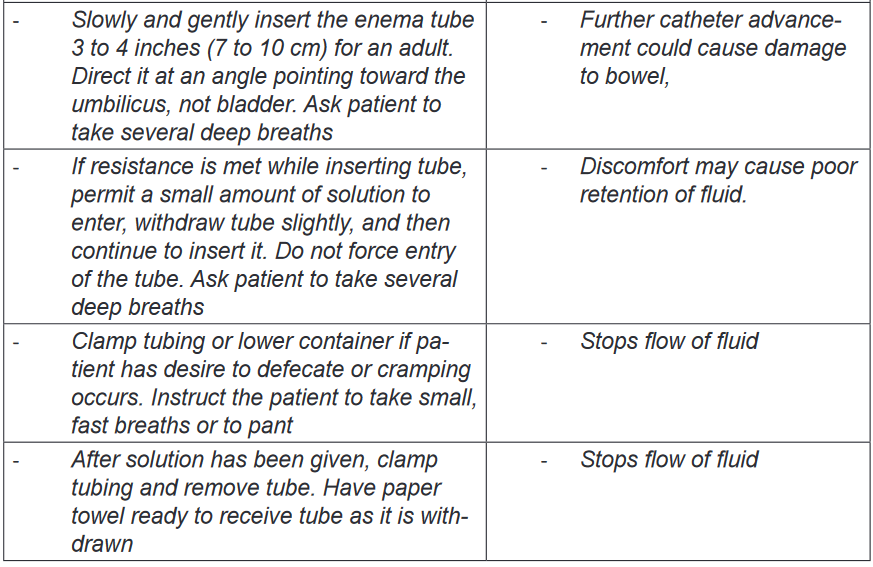
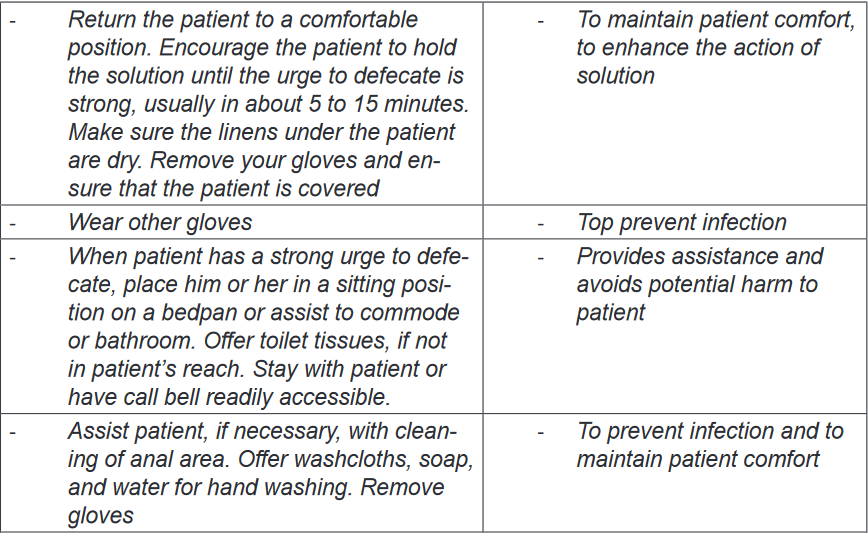
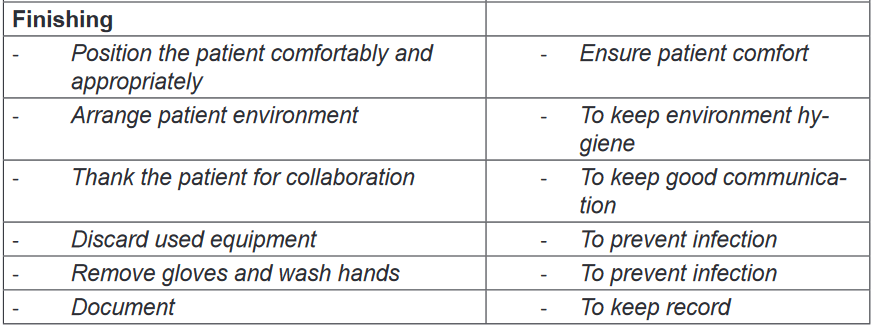
Nursing Alert
• During the procedure the pulse and blood pressure should be monitored.
If the pulse drops and/or the blood pressure rises, the procedure must be
stopped.
• Assess for presence of feces using Bristol stool score (Figure 31 Bristol
stool score) and record.
• In Scybala-type stool (hard, smaller lumps), remove a lump at a time until no
more fecal matter can be felt and place in receptacle.
• In a solid mass, push finger into the middle of the fecal mass and split it,
remove small sections until no more fecal matter can be felt and place in
receptacle. Do not attempt to hook and drag feces as this can damage the
bowel wall.
• If the fecal matter is more than 4cm in diameter and cannot be broken up,
then the procedure should be stopped and medical advice is required.
• If the feces are hard and dry, consider inserting two glycerin suppositories
30 minutes before commencing the procedure.
• If feces are too soft to remove effectively, consider leaving the patient for
another 24 hours to enable further re-absorption of water content and review
fiber content of diet or prescribe appropriate bulking agent.
• Stop the procedure if the patient complains of feeling unwell, having pain or
bleeding, or if patient asks you to discontinue.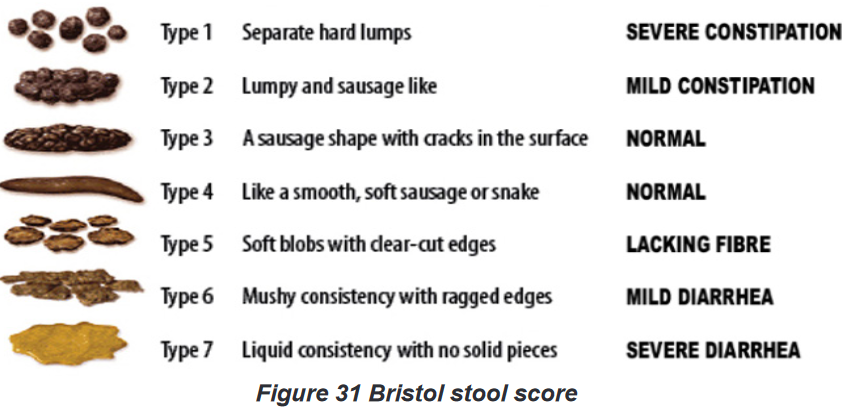
2.7.7. Hygiene Care of ostomies (gastrostomy, ileostomy, colostomy).
A stomy (ostomy) is an opening for the gastrointestinal or urinary tract onto the skin
of the abdomen in the purpose of helping patient with elimination of urines or feces.there are many types of intestinal ostomies: A gastrostomy is an opening through
the abdominal wall into the stomach it is mainly indicated for the purpose of feeding
the patient; A jejunostomy opens through the abdominal wall into the jejunum;
an Ileostomy opens into the ileum; and A Colostomy is an opening through the
abdominal into the colon (ascending, descending or transverse).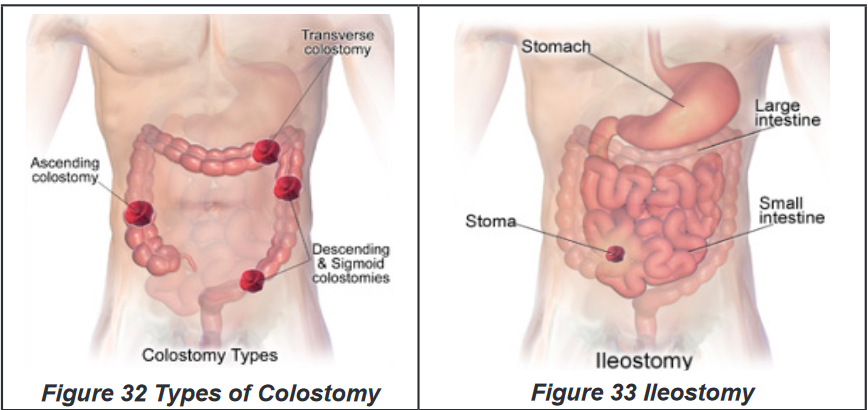
Techniques of providing hygienic care to colostomy or ileostomy: Changing
a colostomy bagPurpose and indications
This procedure is done for the purpose of hygiene and infection prevention of the
patient and is indicated to bedridden patient with colostomy and ileostomy.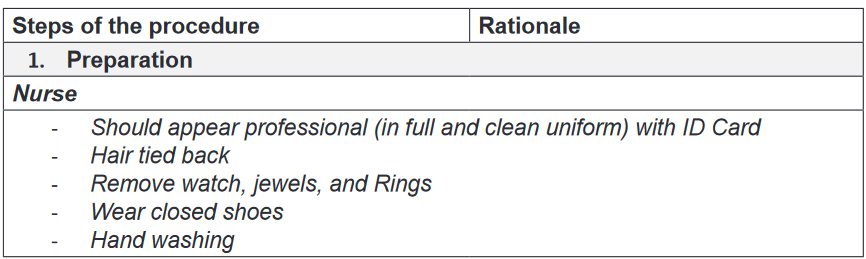
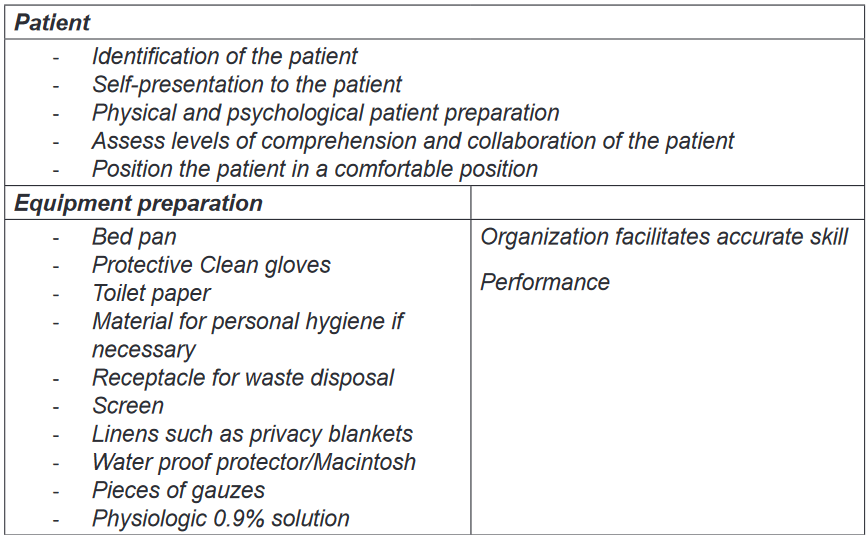
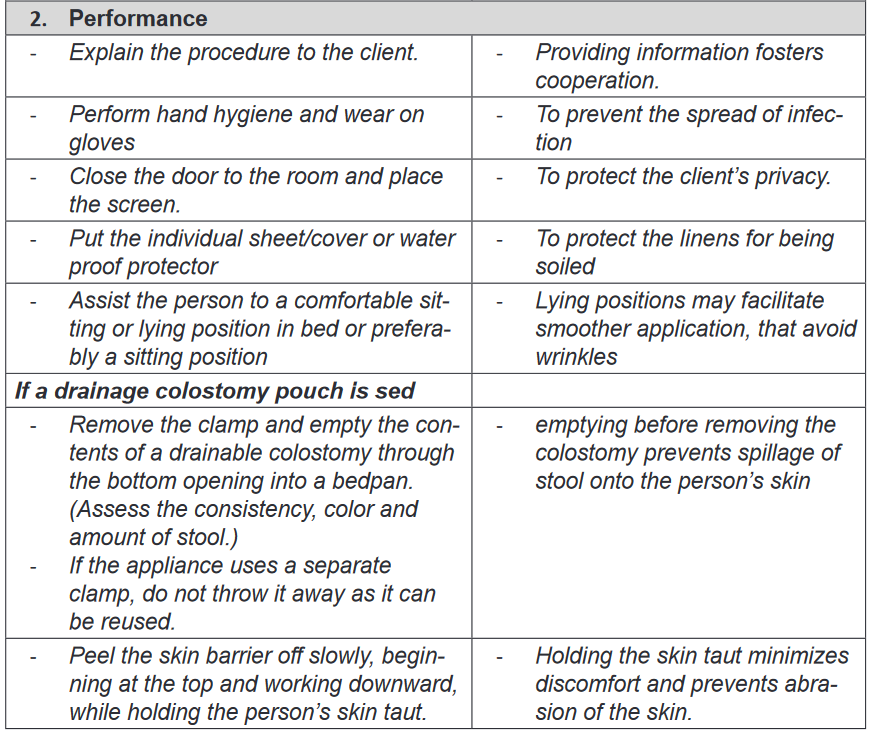
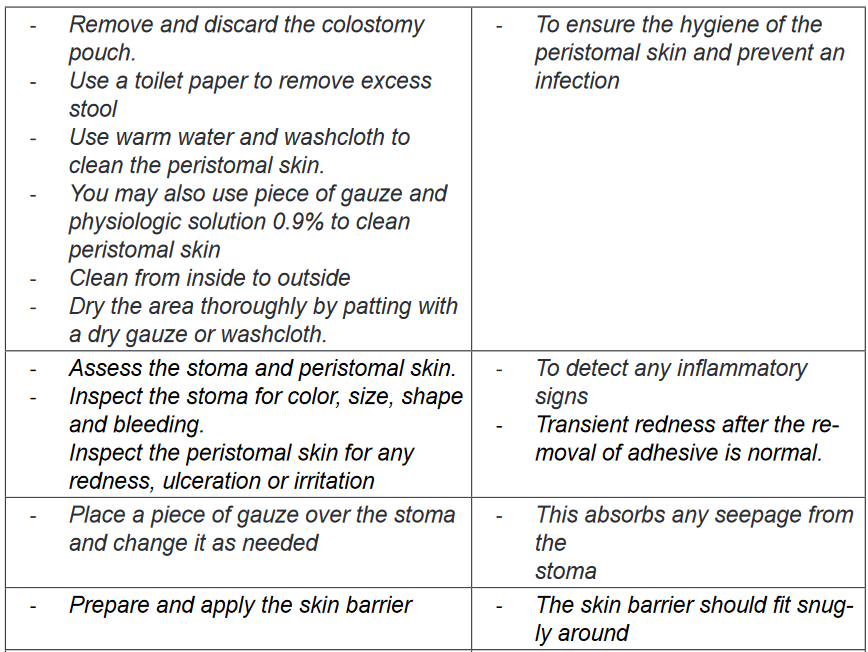
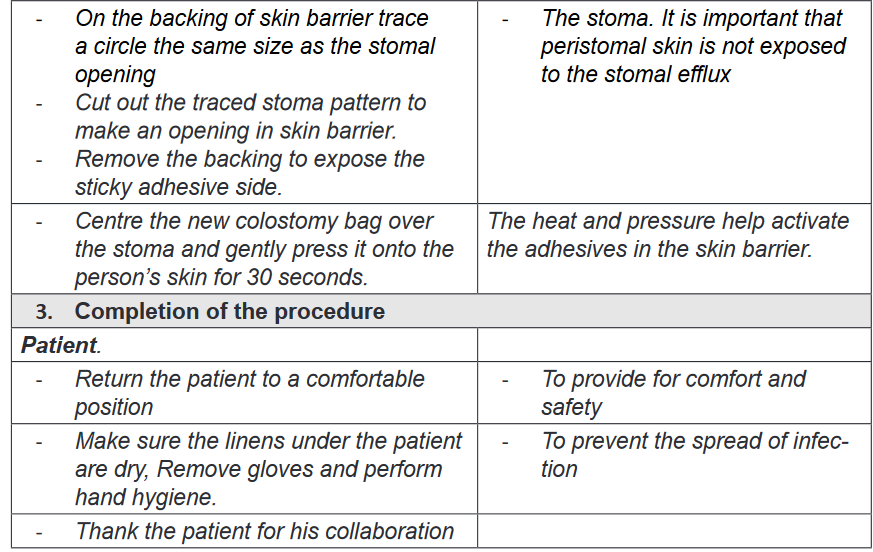
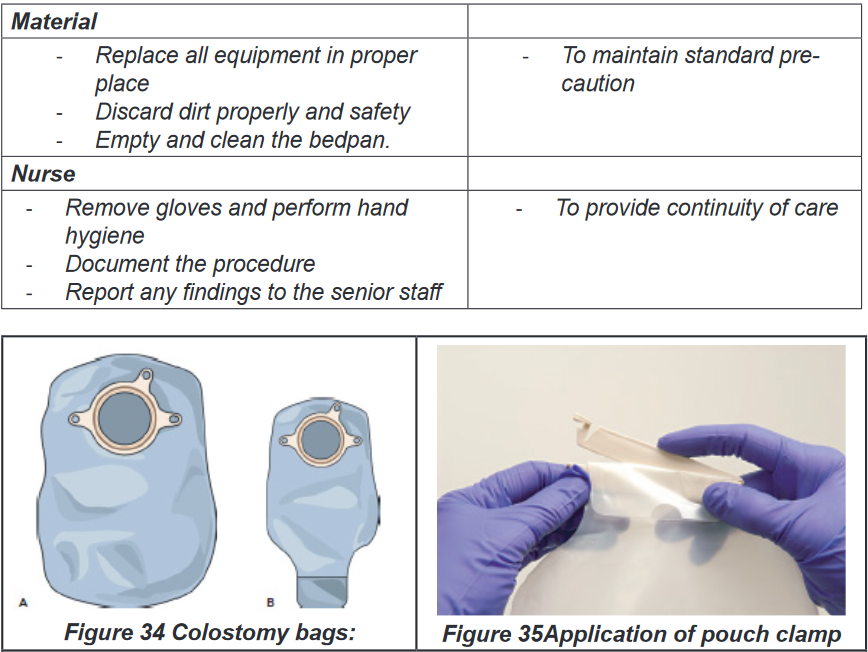
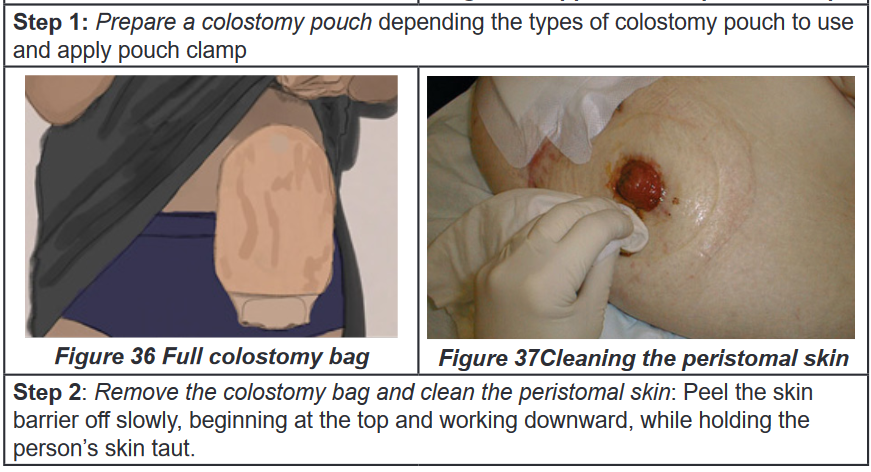
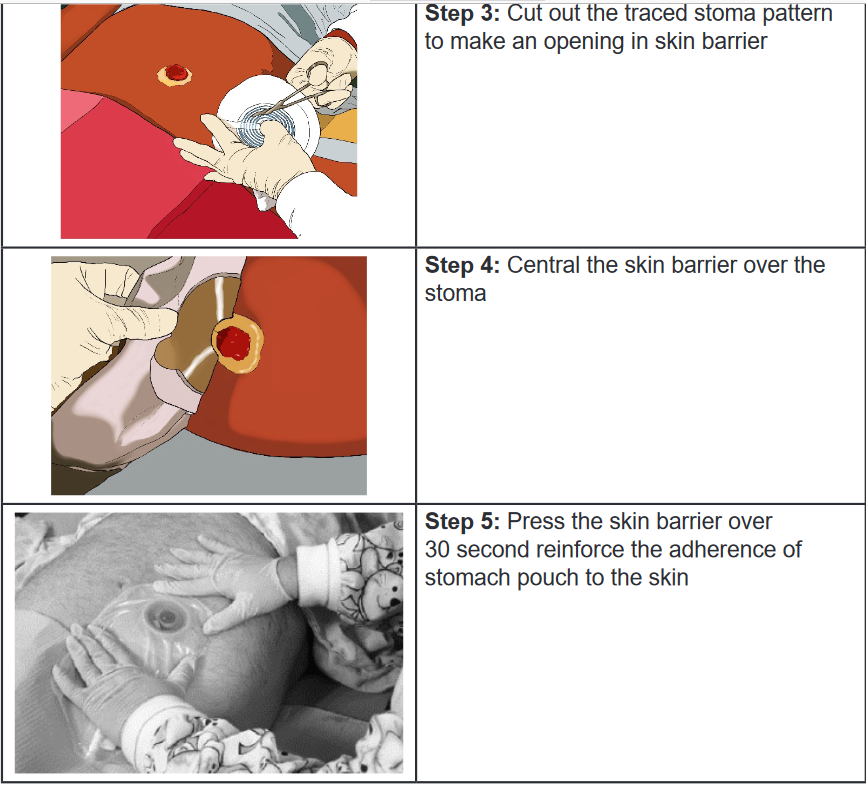
Self-assessment 2.7.
1) When caring for male clients at the healthcare facility who require
assistance with urinary elimination, for which of the following clients
should the nurse use a urinal?
a) Clients who can ambulate
b) Clients who are weak
c) Clients who are unable to walk
d) Clients who are confined to bed2) A nurse is caring for a client with severe pain in the abdomen and
constipation resulting from fecal impaction. Which of the following
interventions should the nurse perform to facilitate easy insertion within
the rectum when removing the fecal impaction?
a) Lubricate the fore finger
b) Place the client in the Sims’ position
c) Lubricate the rectal tube
d) Warm the cleansing solution.3) A physician has ordered the nurse to administer an oil retention enema
to a client for easier expulsion. For how long should the nurse ask the
client to retain the cleansing solution within the large intestine?
a) At least 1 hour
b) At least 10 minutes
c) At least 5 minutes
d) At least half an hour.4) All of the following are devices for elimination except
a) Wheel chair
b) Urinal
c) Bed Pan
d) Diaper5) Define the following bowel diversions:
a) Stoma
b) Ileostomy
c) Colostomy6) list the complications of excessive rectal manipulation
7) Identify the primary action of enema
8) What is the purpose of using diaper for adult patients.
End unit assessment 2
Question I
Bathing is a hygienic practice during which a cleaning agent (such as soap) is used
to remove sweat, oil, dirt, and microorganisms from the skin. Answer the following
questions, which involve the nurse’s role in assisting clients with bathing.
A nurse is caring for an elderly client who has undergone rectal surgery. The
client is averse to bathing daily. The nurse needs to ensure that body areas
subject to greatest soiling or that are sources of body odors are cleaned and
infections do not occur
1) What kind of bath should the nurse suggest to the client?
2) What care should the nurse take when providing perineal care to the client?Question II
Many factors affect ventilation and, subsequently, respiration. Positioning and
teaching breathing techniques are two nursing interventions frequently used to
promote oxygenation. Answer the questions related to nursing intervention to
promote oxygenation.A nurse is caring for a client who is brought to the health care facility with
breathing difficulty. The client is diagnosed to have hypoxia.
In what position should the nurse place the client to promote better breathing?Question III
Nursing care activities such as positioning, moving, and transferring clients
reduce the potential for disuse syndrome. Nurses can become injured if they
fail to use good posture and body mechanics while performing these activities.
Answer the following questions, which involve the nurse’s role in preventing
work-related injuries.A nurse is caring for an elderly client with a fractured leg following a fall. When
caring for this client, the nurse should take precautions to prevent injuries to
him- or herself
1) What care should the nurse take before planning to turn and move the
client?
2) What should the nurse do as part of planning to move the client?
Question IV
Asepsis means practices to decrease or eliminate infectious agents, their
reservoirs, and vehicles for transmission. It is the major method for controlling
infection. Answer the following questions, which involve the various aspects of
asepsis that a nurse should follow while caring for clients.
A nurse practices medical and surgical asepsis to accomplish care for a client
suffering from an infection. There are other clients around who should be
protected from the spread of infection.
1) What are the principles or measures the nurse should follow to break the
chain of infection?
2) What are antimicrobial agents?
3) Which antimicrobial agents should the nurse use and why? Define the
role of each type of agentQuestion V
Heat and cold have various therapeutic uses and each can be used in several
ways. Examples include an ice bag, collar, chemical pack, compress, and
Aquathermia pad. Answer the following questions, which involve a nurse’s role
in the application of a compress.
A nurse is caring for a 2-year-old-client who is being treated for viral fever at the
health care facility. The nurse uses a cold compress for the child.
1) What is the purpose of a cold compress?
2) How should the nurse apply the compress to the client?Question VI
1) Identify the risk factors that predispose a patient to pressure ulcer
formation.
a)
b)
c)
d)
e)
2) Staging systems for pressure ulcers are based on the depth of tissue
destroyed. Briefly describe each stage
I.
II.
III.
IV.
V.UNIT 3: VITAL SIGNS AND PARAMETERS
Key unit competence:
Interprets correctly the measured vital signs and parametersIntroductory activity 3
PERSON A
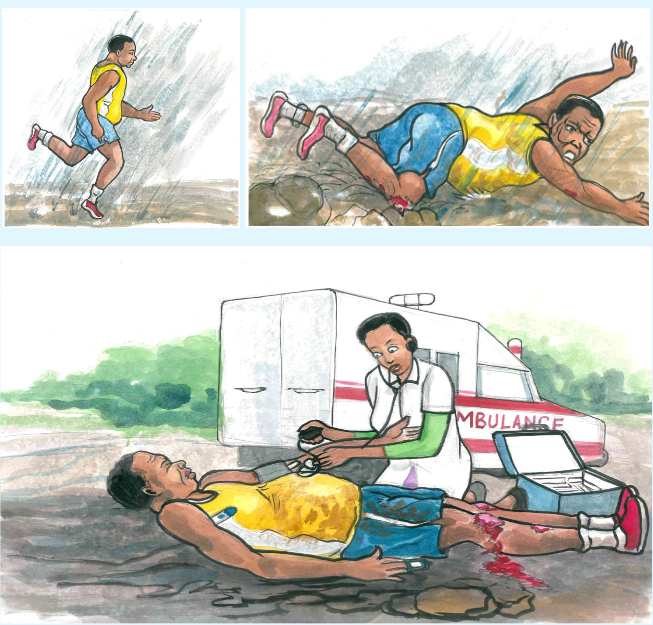
1) By observing these pictures above, what do you think has happened to
the person A?
2) What can you conclude about the health condition of this injured person?
3) According to your observation, what do you think is the nurse doing to
the person A?
4) In your view, what do you think can happen to the person A in case
these actions being done by the nurse are not done?3.1. Introduction to vital signs
Learning activity 3.1.
Do searching of the Fundamentals of Nursing book and read the vital signs unit
and come up with a summary of the following:
1) Definition of vital signs
2) The cardinal vital signs
3) Times to assess the vital signs
4) Guidelines for vital signs assessmentVital signs are the fundamental measurements of life signs. The term vital signs
(VS) suggests assessment of vital or critical physiological functions. Vital signs
provide important information about the interrelationship between body systems.
The vital signs reflect changes in function that otherwise might not be observed.
Vital signs that are within normal limits reflect a person’s physiological wellbeing,
whereas abnormal vital signs may be an early warning of clinical deterioration.The cardinal vital signs are body temperature, pulse, respirations, and blood
pressure. Oxygen saturation is also commonly measured at the same time as the
traditional vital signs. An alteration in vital signs signals a change in physiological
function and the need for medical or nursing intervention.a) Uses of vital signs
Very often the vital signs are used: To establish the diagnoses of the patients:
The disruption of one or several vital signs can orient the diagnosis because it can
be the first sign of disease; to prescribe treatments and for medical follow-
up: They permit to have a control on the patient’s general state. That means that
they are used to evaluate the success of the implementation and good evolution of
prescribed treatment (recovery, relapse of the illness); and to establish nursing
care planb) Times(moments) to assess vital signs
When and how often to assess a specific patient’s vital signs are chiefly nursing
judgments, depending on the patient’s health status. A patient’s vital signs may be
recorded on a routine basis (every 8 hours for most hospitals), however if there is a
change in the patient’s condition then the vital signs may need to be recorded more
frequently depending on the physician orders or according to nurse judgment. Below,
are examples of times (moments) to assess vital signs though the list is not exhaustive: On admission to a health care facility
When a person has a change in health status or reports symptoms such as
chest pain or difficulty breathing.
Before, during and after surgery or an invasive procedure.
Before and/or after the administration of a medication that could affect the
respiratory or cardiovascular systems.
Before and after any nursing intervention that could affect the vital signs
(e.g. ambulating a person who has been on bed rest or when a person is
receiving a blood transfusion).
Following an incident, accident or injury in the health care setting (e.g. when
a person has fallen or has been administered an incorrect medication).c) Guidelines for assessing vital signs
Vital signs are part of the assessment data base. You include them in a complete
physical assessment or obtain them individually to assess a patient’s condition.
Establishing a database of vital signs during a routine physical examination serves
as a baseline for future assessments. Guidelines for assessment of vital signs
include:
Use of functional and appropriate equipment in regard to the size and age
of the patient.
Select equipment based on the patient’s condition and characteristics
Being familiar with normal ranges of vital signs for different ages.
Always compare the patient’s usual range of vital signs with later findings.
Determine the patient’s medical history, therapies, and prescribed
medications. Some illnesses or treatments cause predictable changes in
vital signs.
Control or minimize environmental factors that affect vital signs.
Use an organized, systematic approach when taking vital signs. Each
procedure requires a step-by-step approach to ensure accuracy.
Use vital sign measurements to determine indications for medication
administration. For example, give certain cardiac drugs only within a range
of pulse or BP values. Analyze the results of vital sign measurements. Vital signs are not interpreted
in isolation. You need to also know related physical signs or symptoms and
be aware of the patient’s ongoing health status.
Communicate significant changes in vital signs to the patient’s health care
provider or the charge nurse. Document findings and compare with baseline
measurements to identify significant changes.
Instruct the patient or family caregiver in vital sign assessment and the
significance of findings.
Vital sign measurements can require removing clothing or exposing areas.
Provide patient privacy while being sensitive to cultural norms w h e n
measuring vital signs.Vital signs serve different role. Vitals signs can orient the diagnosis because it can
be the first sign of disease. They are also used to evaluate response to intervention.Self-assessment 3.1.
1) List the vital signs you know
2) What do vital signs serve for?
3) What is the right time to measure the vital signs?
4) Why is it important for the nurse to know the patient’s usual range of
vital signs?3.2. Body temperature
3.2.1. Body temperature overviewLearning activity 3.2.1.
Use the provided book of Fundamentals of Nursing to read the materials on
body temperature under the vital signs unit and make a summary note of the
following:
1) Definition of body temperature
2) Difference between core and surface temperature
3) Normal values of body temperature
4) Factors affecting body temperature
5) Routes of body temperature assessmenta. Concept of Body Temperature
Body temperature is defined as the balance between the heat produced by
the body and the heat lost from the body, measured in heat units called degrees
either Fahrenheit or Celsius. There are two kinds of body temperature: core
temperature and surface temperature. The core temperature which remains
relatively constant is the temperature of the deep tissues of the body, such as the
abdominal cavity and pelvic cavity. The surface temperature is the temperature
of the skin, the subcutaneous tissue, and fat. It rises and falls in response to the
environment.The normal core body temperature is a range of temperatures. No single value
can be considered “normal” since the body temperature fluctuates as a result of
differences in metabolism. The normal range for adults is considered to be between
36°C and 37.5°C (96.8°F to 99.5°F) with the average being 98.6°F(37°C). The core
temperature is generally 1°F to 2°F (0.6°C to 1.2°C) higher than surface (skin)
temperature. This normal temperature range is maintained by keeping a balance
between heat production and heat loss.Box 3.2.
To convert Fahrenheit to Celsius: subtract 32 from Fahrenheit reading
and multiply by 5/9.
C=(F-32°)×5/9
Example104°-32°)×5/9=40°C
To convert Celsius to Fahrenheit: Multiply the Celsius reading by 9/5
and add 32.
F=(C×9/5)+32
Example: (40°C ×9/5)+32=104°F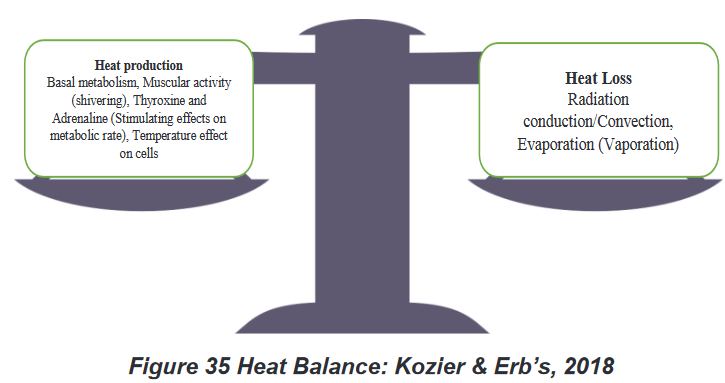
b. Factors affecting body temperature
A variety of internal and external factors affect body temperature. Nurses should
be aware of physiological factors that affect a person’s body temperature so that
they can recognize normal temperature variations and understand the significance
of body temperature measurements that deviate from normal. The common
factors are environment, time of day, gender, age, physical activity and exercise,
medications, food or liquid intake, stress, and illness. Age: Infants have an immature thermoregulatory mechanism and their
temperature is greatly influenced by the environment and must be protected
from extreme changes. Elderly people have decreased thermoregulatory
controls and are also more sensitive to extremes of environmental temperature
changes. Elderly individuals are particularly at risk for hypothermia for a variety
of reasons, such as poor activity, limited metabolism and poor diet, as well
as poor temperature-regulating mechanisms. Many older people, particularly
those over 75 years old, are at risk of hypothermia (temperature below 360C) The action of hormones: At ovulation, a woman’s body temperature may
increase by about 0.30C to 0.60C, due to the influence of progesterone. Just prior
to ovulation the estrogen peak may cause a slight decrease in body temperature.
Thyroxin, adrenaline and noradrenalin all increase body temperature. Rest and sleep: The metabolism slows down during these periods. The
temperature can go down from a few tenth degrees. Time of the day: Body temperature is lowest in the early morning, when
metabolic rate and heat production are at their lowest. The body temperatureis highest in the afternoon and early evening when we are active. Body
temperatures normally change throughout the day, varying as much as 1.00C
between the early morning and the late afternoon. Exercise and physical labor: The role of muscles is predominant in the
production of heat; the muscular activities can increase the metabolism 4 to 5
times to the initial value of rest. Therefore, the temperature can rise from 0.2 to1. 50C according to the activity. However, hard work or strenuous exercise can
increase body temperature to as high as 38.3 to 400 C measured rectally. Stress: Stimulation of the sympathetic nervous system can increase the
production of epinephrine and norepinephrine, thereby increasing metabolic
activity and heat production. The digestion: The combustion of the nutritious substances increases
the production of heat. The abundant meals increase the temperature by
the activation of the metabolism. On the other hand the fasting lowers the
temperature in the beginning, but if it is prolonged, it can increase it. Hot and
cold fluids can have mild effects on the oral temperature reading for 15 to 30
minutes after ingestion. The climate: The temperature of individuals living in tropical countries is of 1
degree more elevated than normal. Contrary in cold countries the temperature
is below the normal. If the patient has been outside in extremely cold weather
without suitable clothing, the body temperature may be low.
Body temperature is most accurate when measured at sites where there is a rich
blood supply. The common routes used to measure temperature are the axillary
(Figure 39 Axillary route) ,oral (Figure 40 Oral route), tympanic (Figure 41
Tympanic route), temporal artery(Figure 42 Temporal route), rectal (Figure 43
Rectal route) and skin routes. Rectal and tympanic membrane measurements
are used to represent core temperatures; oral and axillary measurements reflect
surface temperatures.Oral temperature is the most commonly used and probably the most convenient
method. Provided that it is done correctly, the oral temperature is a reasonably
accurate reflection of the body temperature. To accurately measure an oral
temperature, you must make certain the patient has not eaten, drunk, or smoked
within the last 15 to 30 minutes. After applying a disposable thermometer cover
sheath, the thermometer should be placed deep into the sublingual pocket under
the tongue.Rectal temperature readings are considered the most accurate, and they are the
true reflection of the core temperature of the body. However, rectal temperature is
contraindicated in many clinical situations; for example, people who are undergoing
rectal surgery, have diarrhea or diseases of the rectum, are immunosuppressed,
have a clotting disorder or have significant hemorrhoids. The rectal temperature is
approximately 1°F higher than the oral temperature.The axilla temperature is the preferred site for measuring temperature in newborns
because it is accessible and safe. It measures the surface temperature of the body,
and this method is not accurate if not correctly carried out. Properly carried out,
an axillary temperature is a reasonably accurate reflection of body temperature.
Axillary temperatures are lower than rectal temperatures. The axillary route is used
for patients who cannot hold the oral thermometer in place or for patients for whom
the oral route might pose a safety risk, such as a patient who is having seizures.The axillary route temperature is approximately1°F lower than the oral temperature.
The tympanic membrane is a frequent site for estimating core body temperature.
Like the sublingual oral site, the tympanic membrane has an abundant arterial
blood supply, primarily from branches of the external carotid artery.
Normal range of adult body temperature per site:
Orally 36,7oC to 37,2o C , average: 37oC
Axillary 35,6oC to 36,7o C, average: 36,5oC
Rectally 36,7oC to 37,8o C , average: 37,5oC
New born 36.1-37.7 (axillary)d. Advantages and disadvantages of sites for body temperature
measurement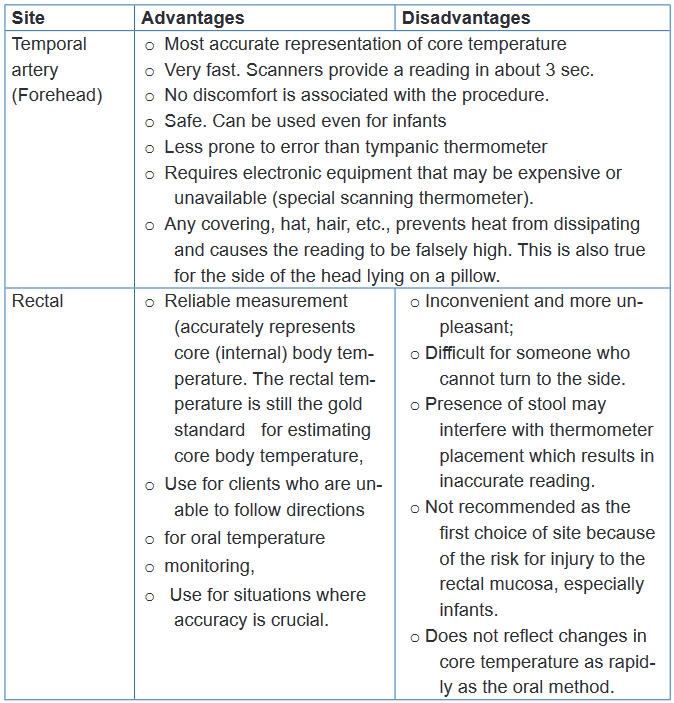
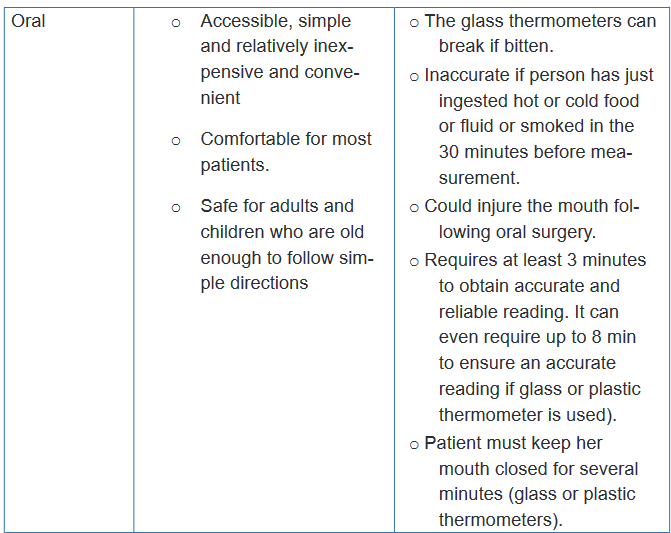
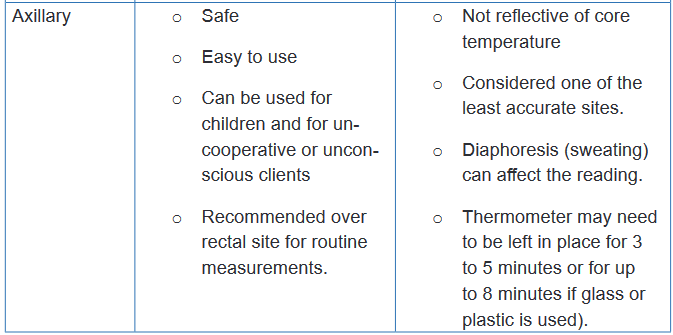
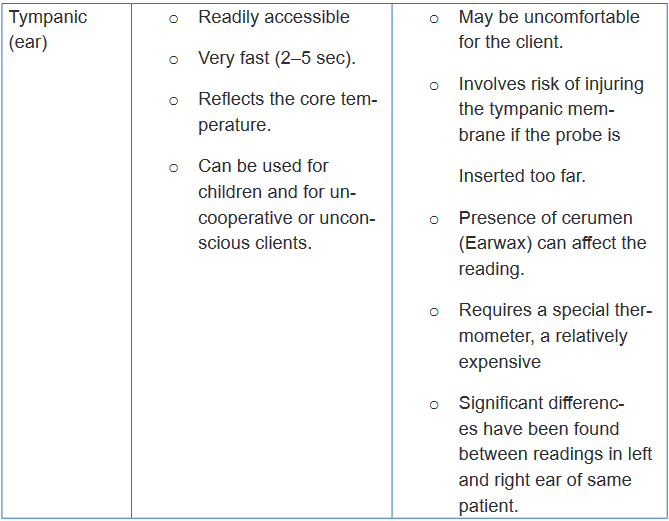
e. Pathological variations (Alterations) of body temperature
There are two primary alterations in body temperature: pyrexia, hyperthermia or
fever and hypothermia. Pyrexia or fever is a body temperature above the normal
range. A very high fever that is above 40oC such as 41oC is called hyperpyrexia.
The client who has fever is referred to as febrile; the one who has not is afebrile.Very high temperatures, such as 41 to 420C, damage the cells throughout the body,
particularly in the brain where destruction of neuronal cells is irreversible. Damage
to the liver, kidneys and other body organs can also be great enough to disrupt
functioning and eventually cause death.Hypothermia which is a core temperature below 95°F (35°C), slows body
metabolism. Mild hypothermia is treated with warm clothes or blankets and ingestion
of warm drinks such as broth or soup. Because up to 40% of body heat can be lost
through the head, coverings such as a hat or scarf can dramatically help reduce
heat loss.Every patient with a fever will not present signs and symptoms of fever in the
same manner. Some of the common signs and symptoms that may indicatefever include: Flushed face , dry hot skin, dry mucous membranes, elevated pulse
rate and rapid respirations, droopy eyes, increased irritability or restlessness,
photophobia, which means the eyes have increased sensitivity to light, thirst,
headache, myalgia (muscle aches), lethargy or drowsiness, diaphoresis, anorexia
and nausea. A patient with hypothermia often presents the following signs and
symptoms: Decreased body temperature, pulse and respirations, severe shivering
initially and feeling of cold and chills, pale, cool, waxy skin, hypotension, lack of
muscle coordination, disorientation, drowsiness progressing to coma, decreased
urinary output.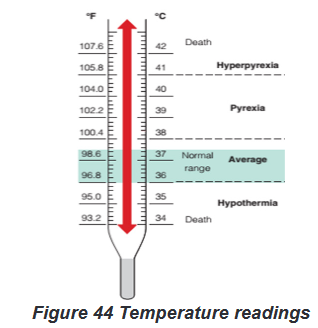
f. Nursing interventions for a patient with alterations of body
temperature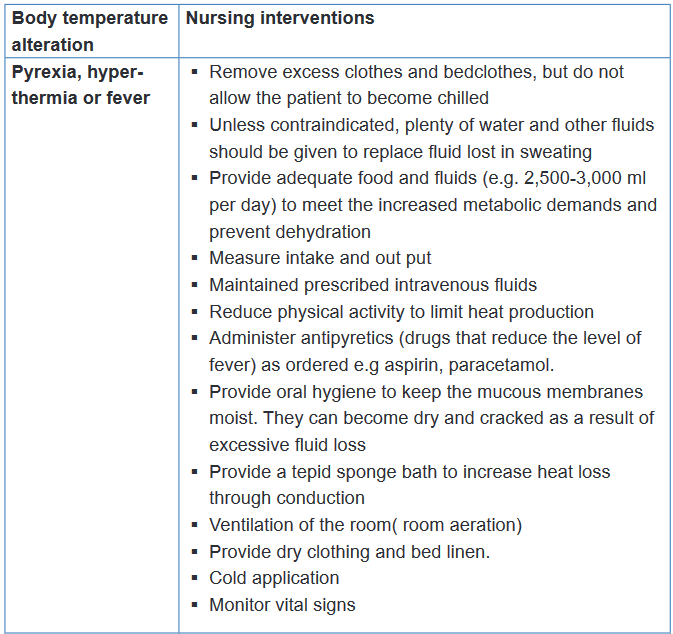
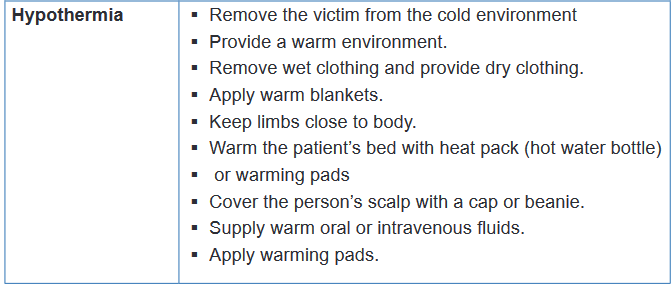
Self-assessment 3.2.1
1) What is the difference between core and surface temperature?
2) Among the following sites of body temperature assessment, which one is
the safest and most convenient site?
a) Oral
b) Tympanic
c) Axillary
d) Rectal
3) Mr. TA, 30 years old is hospitalized in a district hospital in room B
(Private room). During his assessment, the nurse notices that his body
temperature is 1030F.
a) How will the nurse interpret the body temperature of Mr. TA?
b) Based on the body temperature of Mr. TA, what will be the appropriate
nursing interventions by the nurse?3.2.2 Body Temperature measurement/assessment
Learning activity 3.2.2.
In small groups of four (4) learners per each, read firstly the required equipment
and all the steps of axillary, oral, rectal, tympanic membrane and temporal artery
body temperature assessments in the provided procedural guides. Secondly,
use the provided materials for axillary, oral, rectal, tympanic membrane and
temporal artery body temperature assessments and measure the axillary, oral,
tympanic membrane and temporal artery body temperature of your partner.
N.B. In a group of four learners, two learners will pair and everyone will measure
the body temperature (axillary, oral, tympanic membrane and temporal artery)
of his/her partner, write down the results , interpret them and communicate the
results to his/her partner. For the measurement of rectal body temperature, you
will measure it on the provided mannequins.a) Axillary body temperature assessment
To measure body temperature, several types of equipment and different procedures
might be used. To obtain an accurate measurement, choose an appropriate site,
the correct equipment, and the appropriate tool based on the patient’s condition. If
a temperature reading is obtained, it is better to document also the site used along
with the measurement.Various types of clinical thermometers may be used to assess the axillary body
temperature, including mercury glass thermometer, a plastic non-mercury
thermometer, electronic contact thermometer. Plastic non-mercury thermometers
have a digital readout, with oral, axillary, and rectal settings, requiring you to preset
the correct route before taking the temperature. Electronic contact thermometers
consists of a rechargeable battery-powered display unit, a thin wire cord, and
a temperature-processing probe covered by a disposable probe cover. This
thermometer can provide a reading in 2 to 60 seconds, depending on the model
and may be used to assess oral, axillary, or rectal temperatures. The mercury-
in-glass thermometer has been eliminated from health care facilities (no longer
advised) because of the environmental hazards of mercury.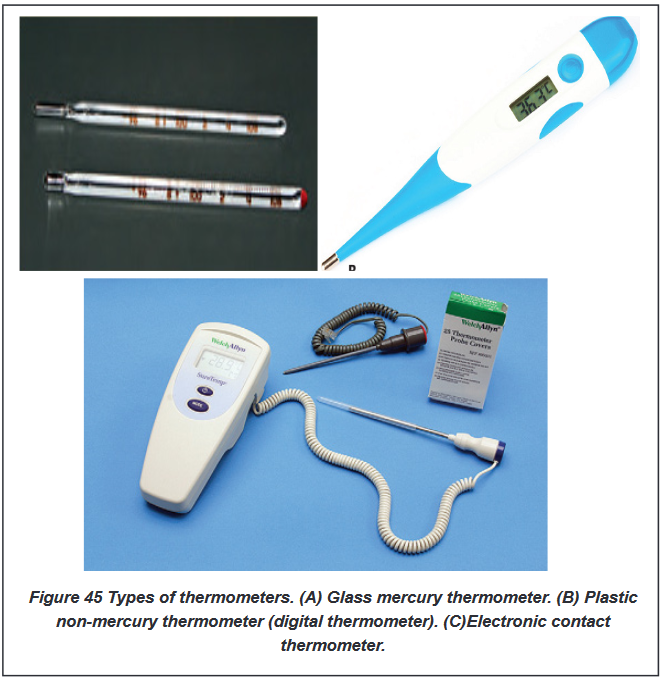
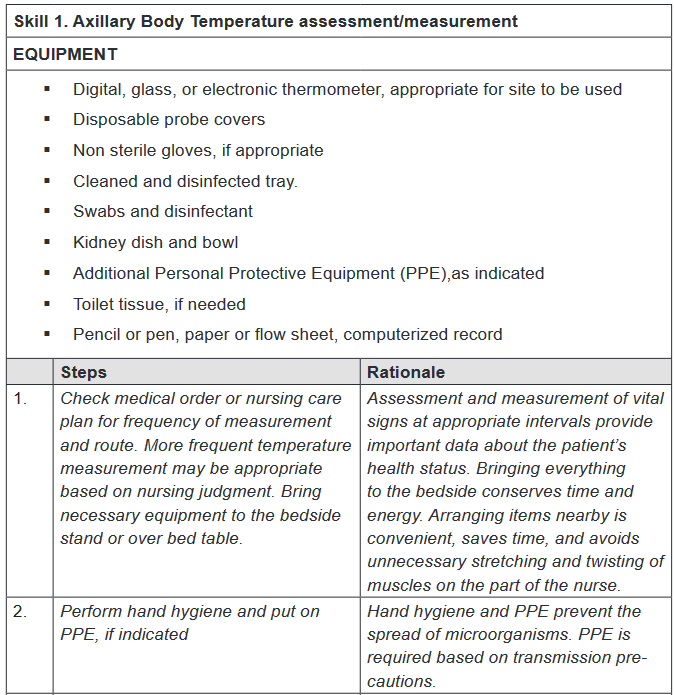
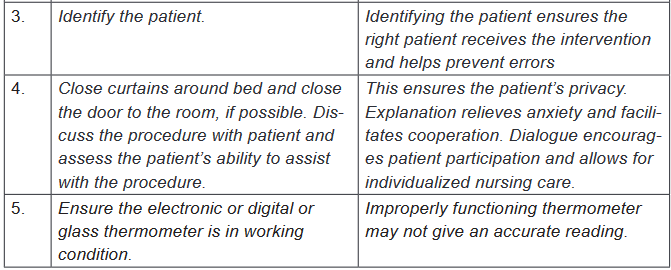
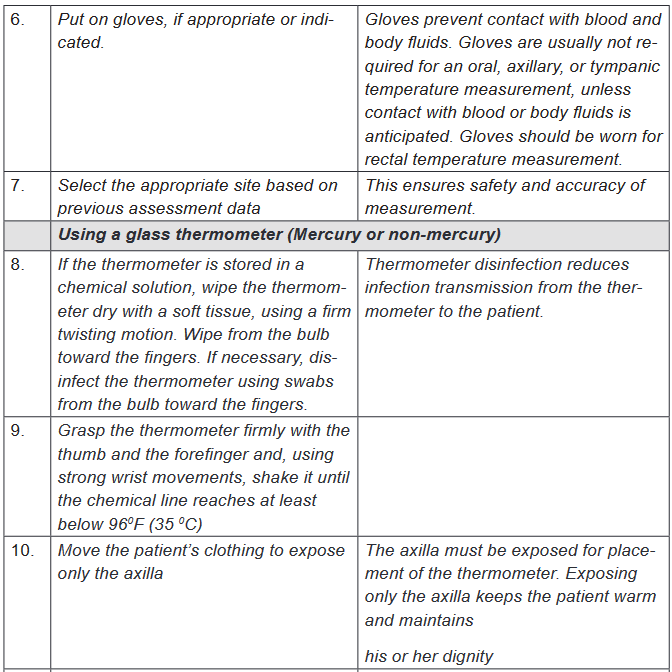
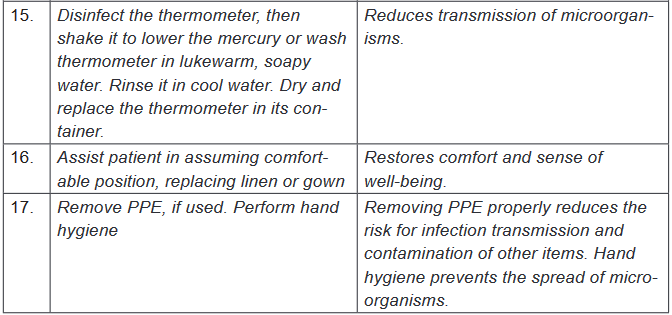
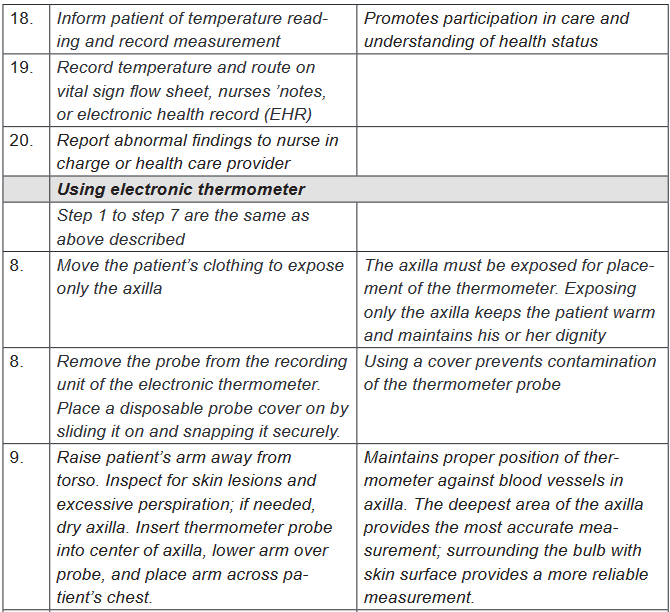
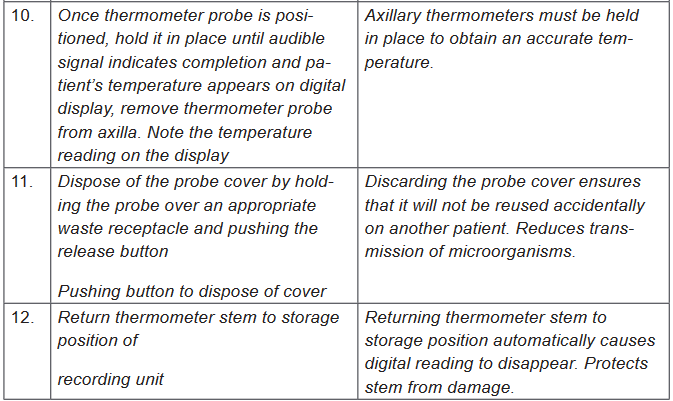
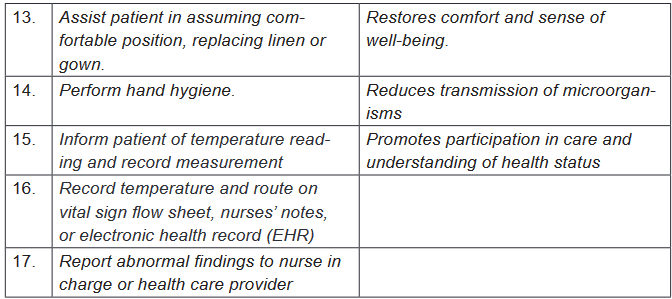
b) Oral body temperature assessment
Various types of clinical thermometers may be used to assess the oral body
temperature, including mercury glass thermometer (no longer advised), a plastic
non mercury thermometer (digital) and electronic contact thermometer.
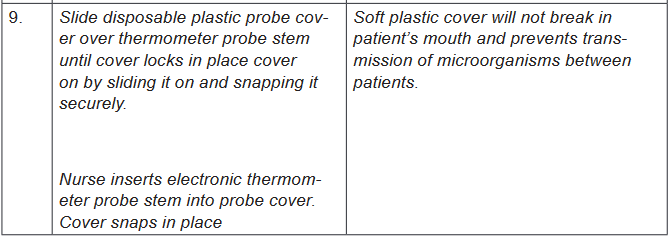
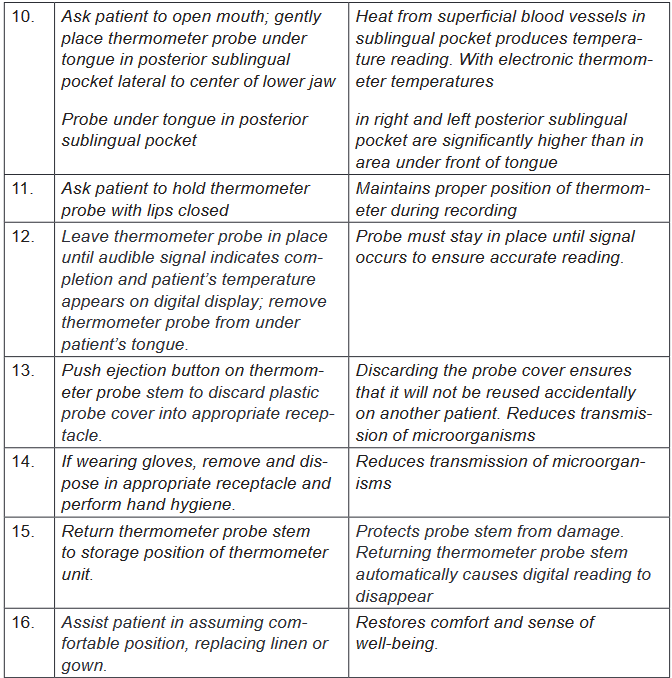
c) Rectal body temperature assessment
Various types of clinical thermometers may be used to assess the oral body
temperature, including mercury glass thermometer (no longer advised), a plastic
non-mercury thermometer (digital) and electronic contact thermometer.
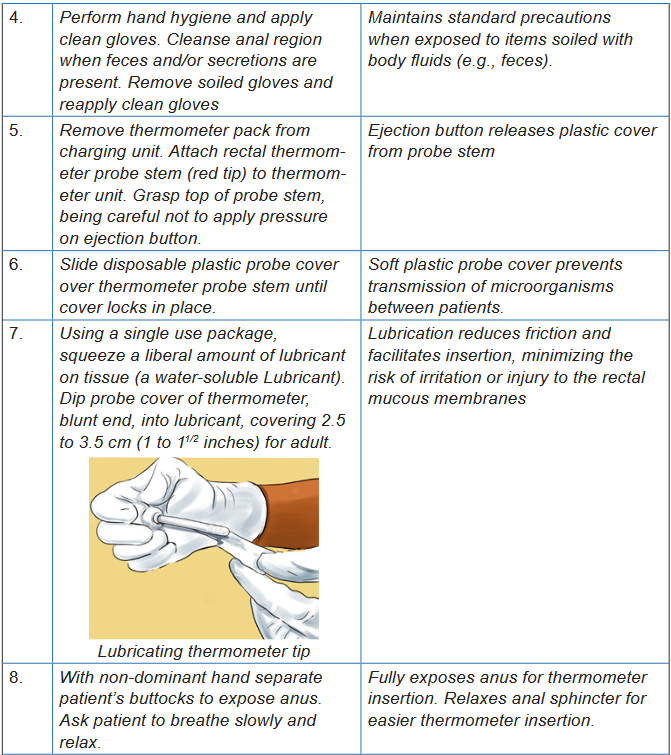
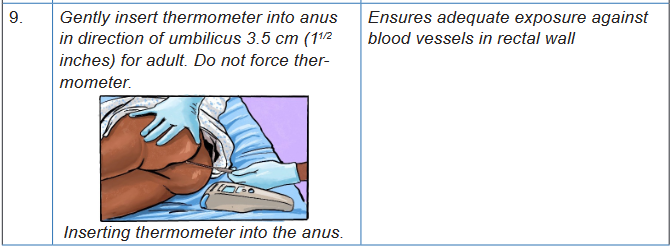
d) Tympanic membrane body temperature assessment
Infrared (tympanic) thermometer is used,. Infrared (tympanic) thermometers
(another form of electronic thermometer); is an otoscope-like speculum with an
infrared sensor tip which detects heat radiated from the tympanic membrane.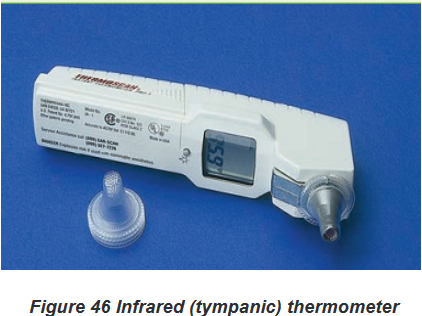
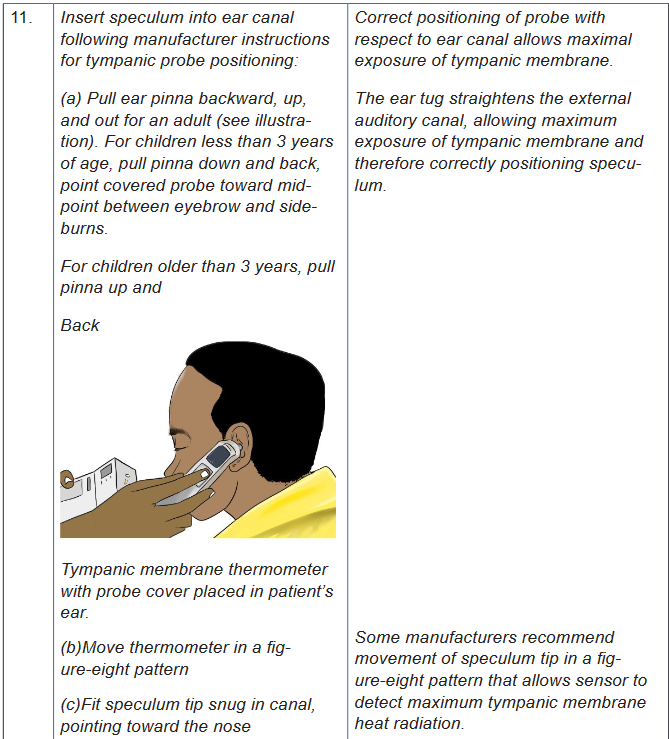
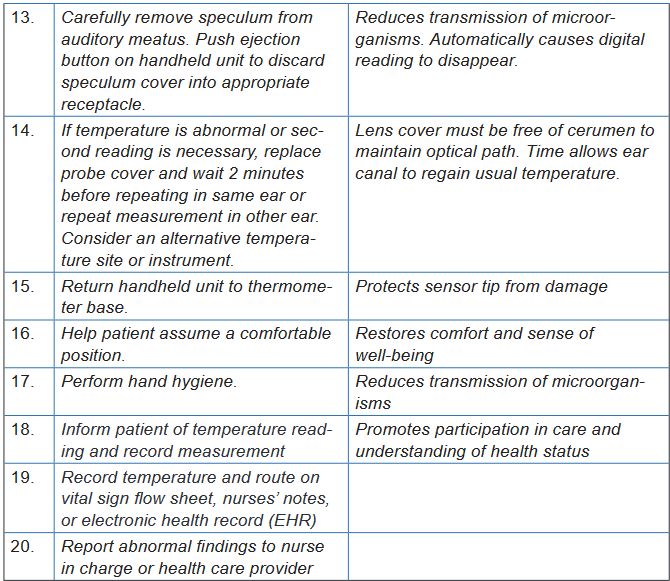
e) Temporal artery body temperature assessment
For a temporal artery thermometer (another form of electronic thermometer); a
handheld scanner with an infrared sensor tip detects the temperature of cutaneous
blood flow by sweeping the sensor across the forehead and just behind the ear.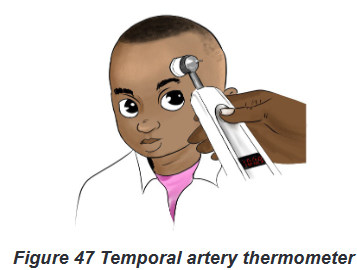
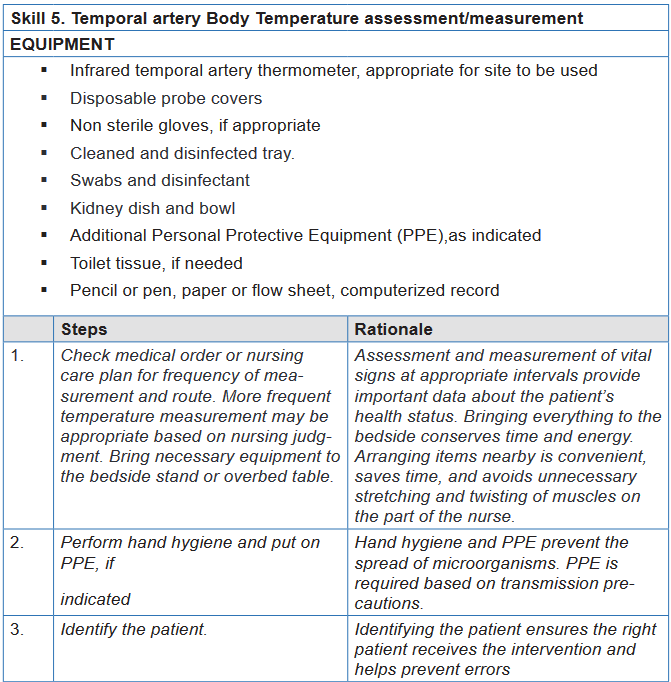
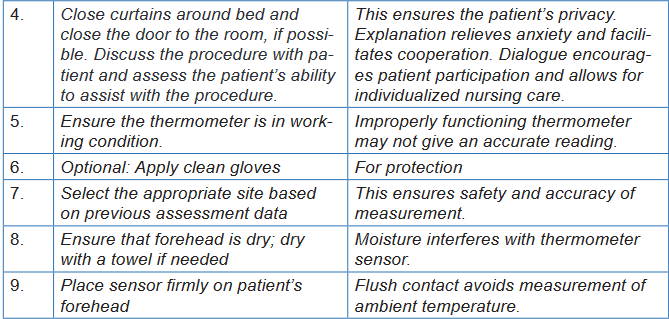
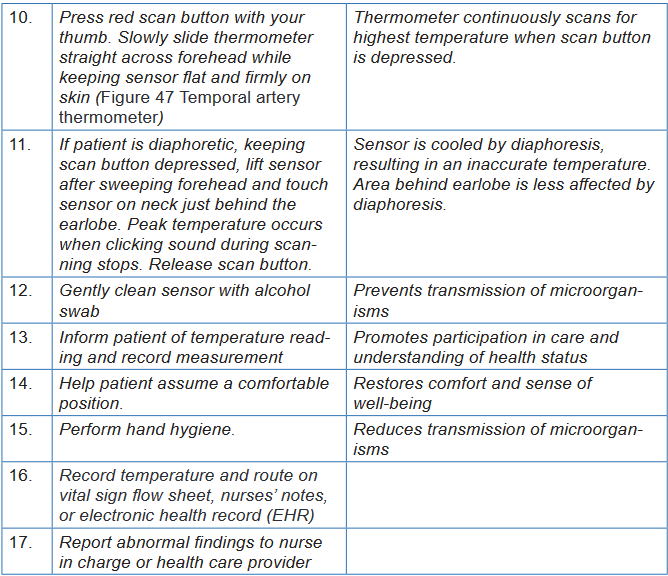
Self -assessment 3.2.2
Instructions:
For you to master the technique of temporal artery body temperature
measurement; go back to your previous groups of four ; let each learner
measures one more time the temporal artery body temperature. The teacher
will be facilitating and observing each student while carrying out the procedure.
After measuring temporal artery body temperature, do the following:
a) Record the temperature reading
b) Interpret the temperature reading.
c) Communicate the result to your partner.3.3. Pulsation/Pulse measurement
Learning activity 3.3.
For Overview
Use the provided book of Fundamentals of Nursing to read the materials on
Pulse under the vital signs unit and make a summary note of the following:
1) Definition of Pulse
2) Normal values and abnormal values of pulse
3) Factors affecting Pulse
4) Sites of pulse palpation
5) Different methods of Pulse taking or How to assess the pulse rate
6) Basic nursing interventions during abnormal pulse.For procedure
Using checklist provided and equipment for pulse taking (see checklist); read all
steps of pulse rate taking in order for you to measure correctly the pulse for your
partner.
1) Observe the images of pulse taking for your guidance. (Figure 48 to
Figure 55)
2) Form pairs of 2 students and each one of you measure a peripheral pulse
selecting the site of Radial artery used for routine assessment of vital
signs
3) Assess the pulse at the apex of the heart (apical pulse) or at a place
where an artery can be pressed by the fingers against a bone (peripheral
pulses).
4) Use Different methods of how to assess the pulse rate:
5) Write down the results for your partner; Interpret results of pulse showing
normal and abnormal values.3.3.1. Pulse overview
The pulse corresponds to the contractions or beats of the heart and is counted by
the number of beats per minute (bpm). The pulse is the rhythmic expansion of an
artery produced when a bolus of oxygenated blood is forced into it by contraction of
the heart. The pulse is the palpable bounding of blood flow noted at various points
on the body and is an indicator of circulatory status.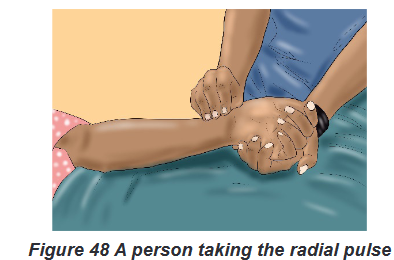
a) Normal and abnormal values of Pulse
i. Normal Pulse Rate
The normal range for healthy young and middle-aged adults is 60 to 100 beats/
min (bpm), with an average rate of 70 to 80 beats/min. The normal range of
pulse rate for adults is 60 to 100 bpm and is measured in beats per minute. Taking
the pulse is a quick and simple way to assess the condition of the heart, blood
vessels, and circulation. While assessing pulse rate as a nurse, you will assess
three characteristics of the pulse: Rate, Rhythm and Volume (strength).ii. Abnormal values of Pulse
A pulse less than 60 bpm is known as bradycardia; a pulse greater than 100
bpm is termed tachycardia.b) Pathological variations of Pulse
There are three abnormalities of Pulse: Tachycardia, Bradycardia and
DysrhythmiaThe first two abnormalities (Tachycardia, Bradycardia) are related to the pulse rate
and the third one (Dysrhythmia) is related to pulse rhythm.Tachycardia is an abnormally elevated HR (Heart Rate), above 100 beats/min in
adults. Bradycardia is a slow rate, below 60 beats/min in adults. In other words, a
pulse less than 60 bpm is known as bradycardia (brady = slow, cardia = heart); a
pulse greater than 100 bpm is termed tachycardia (tachy = rapid, cardia = heart).Dysrhythmia: is an abnormal rhythm when the intervals between beats vary
enough to be noticeable, and is called dysrhythmia.There are also abnormal rhythms which are a group of irregular beats that form a
pattern. An irregular heart rhythm can be very serious and may require additional
assessment by electrocardiogram (ECG), a procedure that traces the electrical
pattern of the heart.c) Factors Affecting Pulse Rate
Because the heart and blood vessels are regulated by the nervous system, conditions
that interfere with normal functioning of the nervous system also affect the pulse.Other factors that may cause variations in pulse rate, rhythm, or quality
include the following: Developmental level (Age): New-borns have a rapid pulse rate. The rate
stabilizes in childhood and gradually slows through old age:
o New-borns: 120–160 bpm
o 1–2 years: 90–120 bpm
o 3–18 years: 80–100 bpm
o Adults: 60–100 bpm
Gender: Adult women have a slightly more rapid pulse rate than do adult men.
Exercise, Meditation, rest, sleep: Muscle activity or exercise normally
increases the pulse rate but meditation, rest and sleep lower the pulse rate.
Food: Ingestion of food causes a slight increase in pulse rate for several
hours.
Stress, Emotions and hormones: Stimulate sympathetic nervous system,
increasing pulse rate.
Fever or Body temperature: The pulse rate tends to increase about 10
beats/ min for each degree Fahrenheit of temperature elevation. As body
temperature increases, each degree Fahrenheit results in speeding the
heart approximately 10 bpm. As the body cools, each degree results in
slowing the pulse by 10 bpm
Disease: Diseases, such as heart disease, hyperthyroidism, respiratory
diseases, and infections, are generally associated with increased pulse
rates. Hypothyroidism is associated with decreased pulse rates.
Blood loss: Small blood loss is generally well tolerated and produces only
a temporary increase in pulse rate but a large blood loss brings about an
increase in pulse rate to compensate for the decreased blood volume. Position changes: Standing and sitting positions generally cause a temporary
increase in pulse rate and decrease in blood pressure as a result of blood
pooling in the veins of the feet and legs. This decreases blood return to the
heart, decreasing blood pressure and subsequently increasing heart rate Medications: Stimulant drugs (e.g., epinephrine) increase pulse rate.
Cardiotonics (e.g., digitalis) and opioids (e.g., narcotic analgesics) or
sedative drugs decrease pulse rate. Hypoxia: Increases the pulse rate.
d) Sites of Pulse palpation
i. Peripheral Pulse Sites:
There are various other pulse sites where the pulse may be palpated by applying
gentle fingertip pressure over the artery against the underlying bone. These sites
are known as the peripheral pulses.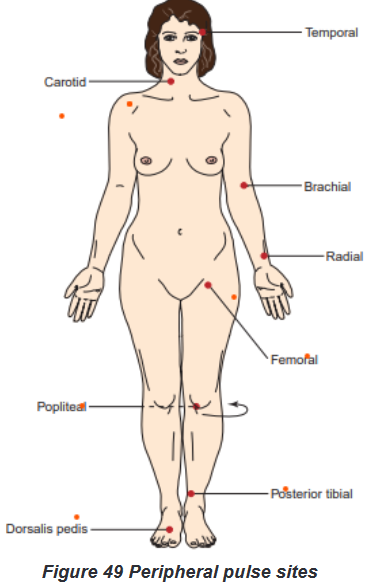
The peripheral pulse sites include the following: Temporal: can be used when
radial pulse is not accessible; Carotid: used in cardiac arrest and cardiopulmonary
resuscitation (CPR); Brachial: used to measure BP; can be used to assess pulse
rate in small children; Radial: routinely used for pulse rate assessment; Femoral:
used to determine circulation to the leg, cardiac arrest; Popliteal: used to determine
circulation to the lower leg; Posterior tibialis: used to determine circulation to the
foot and Dorsalis pedis: used to determine circulation to the foot.ii. Apical Pulse Site:
For Apical pulse; Nurses assess the pulse at the apex of the heart. Auscultate
(listen to) an apical pulse over the apex of the heart, as the heart beats.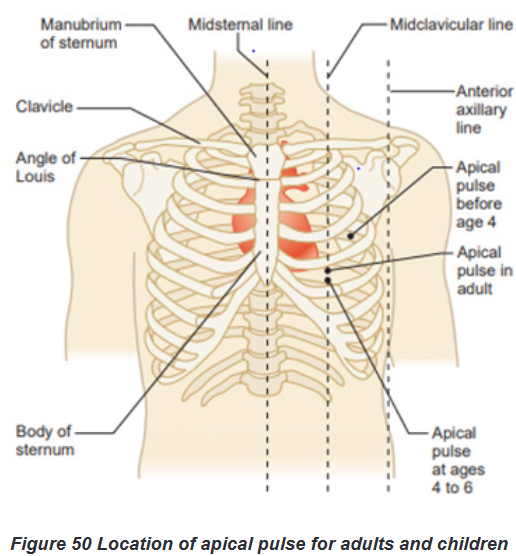
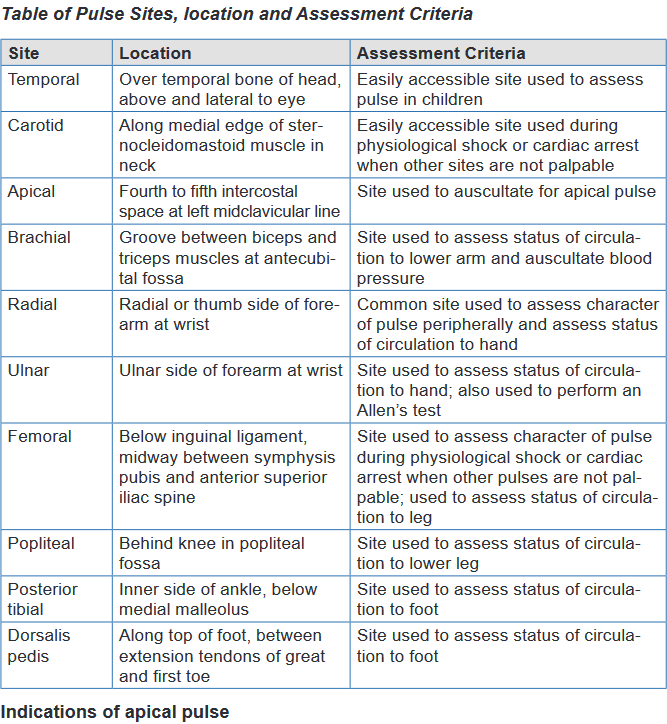
Indications of apical pulse
When cardiac output declines significantly, peripheral pulses weaken and
are difficult to palpate. The radial and apical locations are the most common
sites for pulse rate assessment If the radial pulse is abnormal or intermittent resulting from dysrhythmias or
if it is inaccessible because of a dressing or cast, assess the apical pulse. When a patient takes medication that affects the HR, the apical pulse
provides a more accurate assessment of heart function. The brachial or apical pulse is the best site for assessing an infant’s or
young child’s pulse because other peripheral pulses are deep and difficult
to palpate accurately.a. Nursing interventions during abnormal Pulse
Specific nursing activities and focused assessments for a patient with a dysrhythmia
depend on the cause of the problem and on specific orders from the physician. For
example, a client with a pulse rate of 50 beats/min is usually considered to have
bradycardia. However, such a slow resting heart rate would be perfectly normal for
a well-trained athlete.Some dysrhythmias are benign; that is, they are not dangerous to the client, and
they require no interventions. Nursing strategies that address dysrhythmias,
regardless of cause, include the following: Closely monitor the patient’s VS (Vital Sign): A reduced heart rate
may alter blood pressure and tissue perfusion. The extent of intervention
depends on the effect of the dysrhythmia on the client’s other vital signs. Monitor the patient’s activity tolerance: The degree of activity, orientation,
and level of fatigue while the dysrhythmia is present are indicators of the
patient’s ability to tolerate the dysrhythmia. Collect and assess laboratory data as prescribed: Cardiac function
depends on normal electrolyte balance, particularly potassium, calcium,
and magnesium levels. If a client is receiving medications that affect cardiac
rhythm, serum levels of these medications must be checked periodically. Help determine the cause of the dysrhythmia: Determine when the client
experiences the dysrhythmia. Are there precipitating or alleviating factors? Administer antidysrhythmic medications: These are prescribed to
control the heart rhythm Provide emotional support: The client experiencing a dysrhythmia may be
frightened by the experience. Explain all procedures to the client and family
members, and maintain a calm presence.
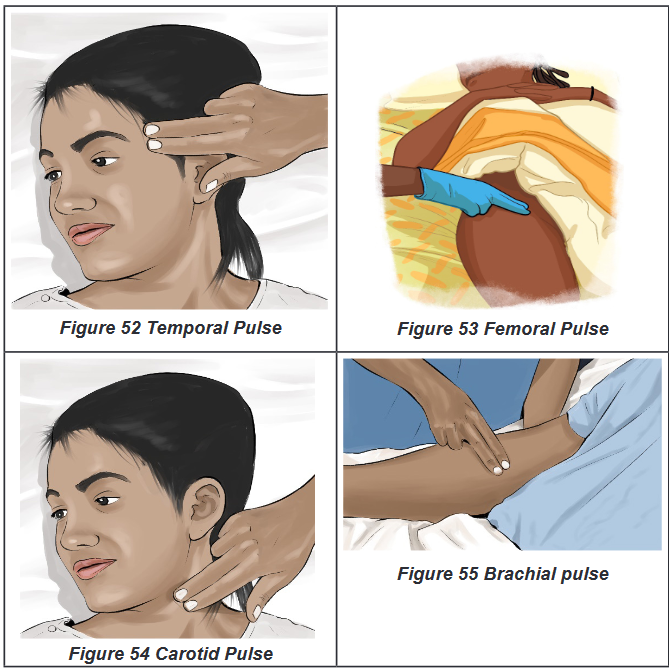
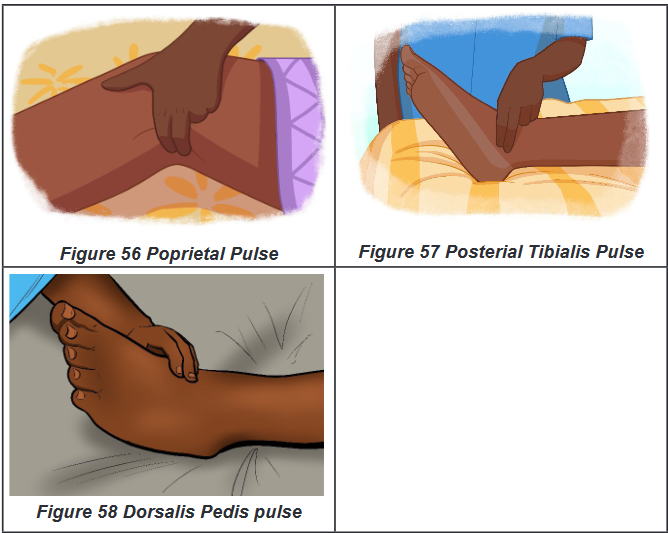
a) Assessment of pulse
To assess the pulse rate, count the number of beats per minute while palpating or
auscultating. Begin the count with one, rather than zero. For normal, healthy adults,
you can determine the rate of a regular heart rhythm by counting the pulse for 15
seconds and multiplying the result by 4. Research is conflicting, but some studies
indicate that a 30-second count is more accurate. If the pulse is irregular or slow,
always count for 1 full minute.i. Assessing Peripheral Pulses
Make sure the client is resting while you assess the pulse.
Count for 15 or 30 seconds if the pulse is regular; count for 60 seconds if it
is irregular.
Note pulse rate, rhythm, and quality.
Compare pulses bilaterally.ii. Assessing the Apical Pulse;
Assessing the apical rate requires a stethoscope and is done as follow:
Position the patient supine or sitting.
Palpate and place the stethoscope at the 5th intercostal space at the
midclavicular line.
Count for 60 seconds.
Note pulse rate, rhythm, and quality and the S1 and S2 heart sounds.Assessing for an Apical-Radial Pulse Deficit
Palpate and place stethoscope over apex of the heart.
Palpate the radial pulse.
Have two nurses carry out the procedure, if possible.
Count for 60 seconds, simultaneously.
Compare the pulse rate at both sites; calculate the difference.Pulse Amplitude
Pulse amplitude typically is graded as 0 to 4:
0 (absent pulse): pulse cannot be felt, even with the application of extreme
pressure
1 (thread pulse): pulse is very difficult to feel, and applying slight pressure
causes pulse to disappear • 2 (weak pulse): pulse is stronger than a thready
pulse, but applying light pressure causes pulse to disappear
3 (normal pulse): pulse is easily felt and requires moderate pressure to
make it disappear
4 (bounding pulse): pulse is strong and does not disappear with moderate
pressureImplementation using the procedural guide for peripheral pulse measurement
Equipment
Watch with second hand or digital readout
Pencil or pen, paper or flow sheet, computerized record
Nonsterile gloves, if appropriate; additional PPE, as indicated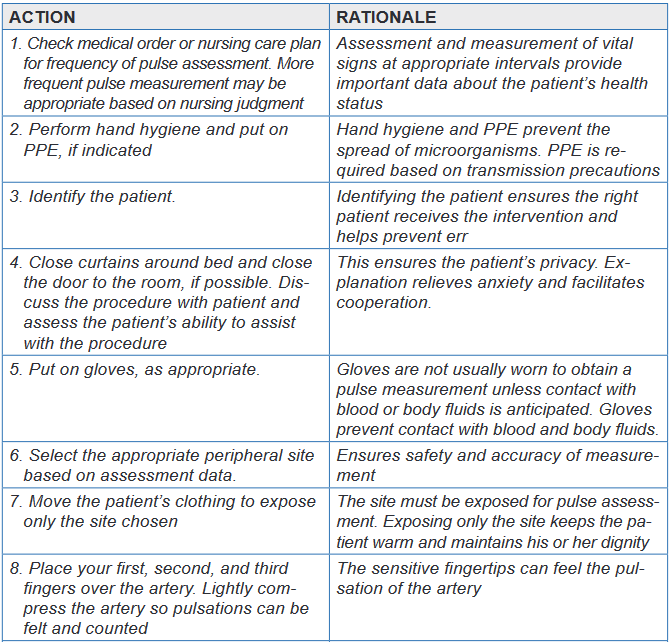
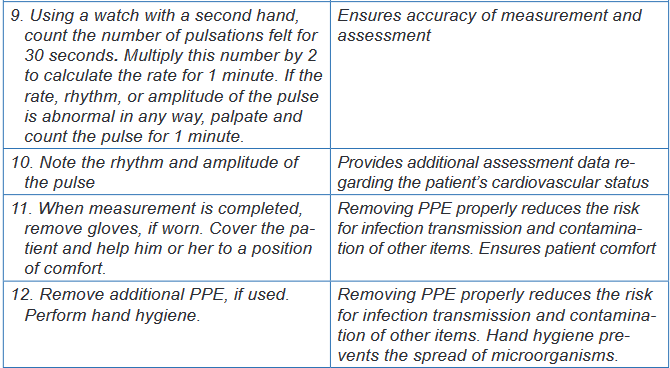
Evaluation
The expected outcomes are met when the patient’s pulse is assessed accurately
without injury and the patient experiences minimal discomfort.Unexpected situations and associated interventions
The pulse is irregular: Monitor the pulse for a full minute. If the pulse is
difficult to assess, validate pulse measurement by taking the apical pulse for
1 minute. If this is a change for the patient, notify the physician. The pulse is palpated easily, but then disappears: Apply only moderate
pressure to the pulse. Applying too much pressure may obliterate the pulse. In case you cannot palpate a pulse: Use a portable ultrasound Doppler
to assess the pulse. If this is a change in assessment or if you cannot find
the pulse using an ultrasound Doppler, notify the physician. If you can find
the pulse using an ultrasound Doppler, place a small X over the spot where
the pulse is located. This can make palpating the pulse easier because the
exact location of the pulse is known.Special considerations
General Considerations
The normal heart rate varies by age.
When palpating a carotid pulse, lightly press only one side of the neck at
a time. Never attempt to palpate both carotid arteries at the same time.
Bilateral palpation could result in reduced cerebral blood flow
If a peripheral pulse is difficult to assess accurately because it is irregular,
feeble, or extremely rapid, assess the apical rate.Infant and Child Considerations
For children younger than 2 years of age, assess the apical pulse.
Do not measure the radial pulse because it is difficult to palpate accurately
in this age group
Measure the apical rate if the child has a cardiac problem or congenital
heart defect.Self-assessment 3.4.
For overview
1) What are the normal values of pulse?
2) Explain the three abnormalities or variations of Pulse?
3) List the Eight peripheral pulse sites
4) Explain how to assess peripheral, and apical pulses?
5) Describe the seven Nursing strategies that address dysrhythmias,
regardless of causeFor procedure
For you to master the technique of Pulse rate taking; going back to your previous
groups of two; let each student takes one more time the pulse of his /her partner.
The teacher will be facilitating and observing each student while carrying out
the procedure.
1) Record the results
2) Interpret them.
3) Communicate results to your partner.3.4. Blood Pressure
Learning activity 3.4.
Section (a): For over view
Use the provided book of Fundamentals of Nursing and read the materials
on blood pressure under the vital signs unit and make a summary note of the
following:
1) Definition of blood pressure
2) Difference between systolic and diastolic blood pressure
3) Determinants of blood pressure
4) Normal values of blood pressure
5) Factors affecting blood pressure
6) Alterations of blood pressure
7) Nursing interventions for a patient with alterations of blood pressureSection (b): For measurement
In small groups of four (4) learners per each, read firstly the required equipment
and all the steps of blood pressure assessment in the provided procedural
guide. Secondly, use the provided materials for blood pressure measurement
and measure the blood pressure of your partner. N.B. In a group of four
learners, two learners will pair and every one will measure the blood pressure
of his/her partner, write down the results and interpret them.3.4.1. Blood Pressure overview
Blood pressure is the force exerted on the walls of an artery created by blood
as it flows through the arteries.Blood flows throughout the circulatory system because of pressure changes,
moving from an area of high pressure to an area of low pressure. Under high
pressure the left ventricle contracts and ejects blood into the aorta which creates
the peak pressure known as systolic pressure. When the ventricles relax, the
blood remaining in the arteries exerts a minimum pressure know as diastolic
pressure. Thus, Diastolic pressure is the minimal pressure exerted against the
arterial wall at all times. In other words, systolic blood pressure is the pressure
exerted by the blood flow on the arterial wall at the time of the systole: that means
that when the left ventricle of the heart contracts throws blood in the circulation, the
arteries are then to their maximum of tension. And diastolic blood pressure is the
pressure exerted by blood on the arteries during the diastole. That means that at
the time of the laxity of the ventricle (at rest).Blood pressure is measured in millimeters of mercury (mm Hg) and recorded as a
fraction: systolic pressure over the diastolic pressure. According to the National
Heart Foundation of Australia (2013), normal blood pressure for a healthy adult
is usually less than 120/80 mm Hg (i.e. systolic blood pressure less than 120 and
diastolic blood pressure less than 80 mm Hg). The difference between the diastolic
and the systolic pressures is called the pulse pressure. A normal pulse pressure
is about 40 mm Hg but can be as high as 100 mm Hg during exercise. A consistently
elevated pulse pressure occurs in arteriosclerosis. A low pulse pressure (e.g. less
than 25 mm Hg) occurs in conditions such as severe heart failure.a) Normal values of blood pressure
The systolic pressure varies between 90 and 140 mm Hg (adult), for men
aged of 45 years and more, it can go up to 150mmHg.
The diastolic pressure, it is between 60 and 90 mm Hg (adult)
The pulse pressure can vary from 30 to 50 mm Hg
Newborn: 65-90/ 30-60 mmHg (systolic/ diastolic)
Infants: 65-125/ 40-90 mmHg (systolic/ diastolic)
Children: 80-120/ 45-85 mmHg (systolic/ diastolic)
Adolescents: 95-135/50-70 mmHg (systolic/ diastolic)b) Determinants of blood pressure
Arterial blood pressure is the result of several factors: the pumping action of the heart,
the peripheral vascular resistance (the resistance supplied by the blood vessels through
which the blood flows), the blood volume, blood viscosity and elasticity of vessels. The pumping action of the heart: Cardiac output is the volume of blood
pumped into the arteries by the heart during 1 minute. When the pumping
action of the heart is weak, less blood is pumped into arteries, and the blood
pressure decreases. When the heart’s pumping action is strong and the volume
of blood pumped into the circulation increases, the blood pressure increase.
The cardiac output for an adult at rest is 4 to 6 liters of blood each minute. The peripheral vascular resistance: if the caliber (lumen) of the peripheral
vessels is abnormally small, the blood pressure increases, inversely if the
caliber is very large the blood pressure decreases. The blood volume: The volume of blood circulating within the vascular system
affects BP. Most adults have a circulating blood volume of 5000 ml. Normally
the blood volume remains constant, when it decreases, for example in case of
hemorrhage, the blood pressure is low. If it increases (blood transfusions), the
blood pressure rises. The blood viscosity or consistence of the blood: more blood is viscous
(thick); more the blood pressure will be raised. Because the resistance is
increased. The hematocrit, or percentage of red blood cells in the blood,
determines blood viscosity. When the hematocrit rises and blood flows slowly,
arterial blood pressure increases. The heart contracts forcefully to move the
viscous blood through the circulatory system. The elasticity of vessels: the vessels with a reduced elasticity, offer more
resistance to the blood passage. Therefore, if the resistance increases, the
blood pressure will be increasedc) Factors affecting blood pressure
Among the factors influencing blood pressure are age, exercise, stress, ethnicity,
obesity, gender, medications, obesity, diurnal variations, medical conditions and
body temperature. Age: The blood pressure varies with the age. It is usual to note a progressive
increase of blood pressure with the age. In elderly people, elasticity of the
arteries is decreased. The arteries are more rigid and less yielding to the
pressure of the blood. This produces an elevated blood pressure for the
elderly. Exercise: Physical activity increases both the cardiac output and hence
the blood pressure, thus a rest of 20 to 30 minutes following exercise is
indicated before the blood pressure can be reliably assessed. Stress: Anxiety, fear, pain, and emotional stress result in sympathetic
stimulation. Stimulation of the sympathetic nervous system increases
cardiac output and vasoconstriction of the arterioles, thus increasing the
blood pressure. Anxiety raises BP as much as 30 mmHg. Sex/ Gender: After puberty, females usually have lower blood pressures
than males of the same age, this difference is thought to be due to hormonal
variations. After menopause, women generally have higher blood pressures
than before. For men, the maxima are from 125 to 140 mm Hg whereas for
women of the same age it is less elevated at 115 to 130. For the minima, it
is generally the same for two sexes. Diurnal variations: Pressure is usually lowest early in the morning, when
the metabolic rate is lowest, then rises throughout the day and peaks in the
late afternoon or early evening. Disease process: any condition affecting the cardiac output, blood viscosity,
and/ or compliance of the arteries, has a direct effect on the blood pressure. Position: A person in lying down position normally the blood pressure is
low, while in standing or seated position the blood pressure is high. Medications: many medications may increase or decrease the blood
pressure. Obesity: pressure is generally high in some overweight and obese people
than in people of normal weight.d) Pathological variations or alterations of blood pressure
The two common alterations of blood pressure are hypertension and hypotension.i. Hypertension
Hypertension is a blood pressure that is persistently above normal. In other words,
hypertension is defined as systolic blood pressure (SBP) greater than 140mmHg
and diastolic blood pressure (DBP) greater than 90mmHg. Hypertension is often
asymptomatic disorder characterized by persistently elevated blood pressure.
Factors such as obesity, cigarette smoking, excessive alcohol intake, elevated
blood cholesterol, lack of physical exercises and continued exposure to stress are
risk factors for hypertension.Hypertension cannot be diagnosed/confirmed unless an elevated blood pressure
is found when properly measured twice with well-maintained equipment at different
times, it is usually asymptomatic and is often a contributing factor to myocardial
infarctions and stroke. An elevated blood pressure of unknown cause is called
primary hypertension. An elevated blood pressure of known cause is called
secondary hypertension.
Classification of Blood Pressure for Adults ages (18yearsand older)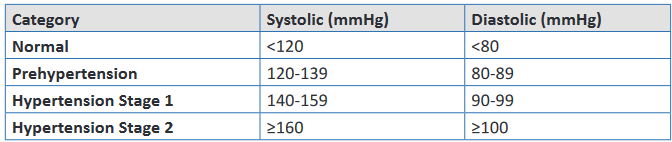
Nursing interventions for a patient with hypertension:
Put the patient in supine position
Assure calmness around him and to reassure maximum relaxation.
Give glucose solution drip
Give diuretic if the high blood pressure is very important
Continue observation
Treat cause
Refer to the hospital center if you are in health center or seek for medical
advice.ii. Hypotension
Hypotension is a blood pressure that is below normal. It is an SBP less than
90mmHg.For most individuals hypotension is an abnormal finding associated with an
illness (e.g., hemorrhage or myocardial infarction). Hypotension occurs when
arteries dilate, the peripheral vascular resistance decreases, the circulating
blood volume decreases, or the heart fails to provide adequate cardiac
output. Signs and symptoms associated with hypotension include pallor, s k i n
mottling, clamminess, confusion, dizziness, chest pain, increased heart
rate, and decreased urine output. Hypotension is usually life threatening and
needs to be reported immediately to the patient’s health care provider.Nursing interventions for a patient with hypotension
Put the patient in Trendelenburg
Give physiological solution drip of preference or Ringer Lactate
Continue observation
Treat cause
Refer to the hospital if you are in health center or alert the physician when
you are at the hospital3.4.2. Blood Pressure measurement
Blood pressure is measured with a blood pressure cuff, a sphygmomanometer
and a stethoscope. The blood pressure cuff consists of the bladder; that is, a rubber
bag that can be inflated with air. It is covered with cloth and has two tubes attached
to it. One tube connects to a rubber bulb that inflates the bladder. A small valve
on the side of this bulb traps and releases the air in the bladder. The other tube is
attached to a sphygmomanometer. The sphygmomanometer indicates the pressure
of the air within the bladder. There are two types of sphygmomanometers: aneroid
and digital (electronic).The aneroid sphygmomanometer is a calibrated dial with a needle that points to the
calibrations. Most clinical settings use digital (electronic) sphygmomanometers;
however, manual blood pressure measurements are more reliable and
accurate than electronic blood pressure devices, which need to be calibrated
regularly for accuracy. All health care facilities should have manual blood pressure
equipment available for use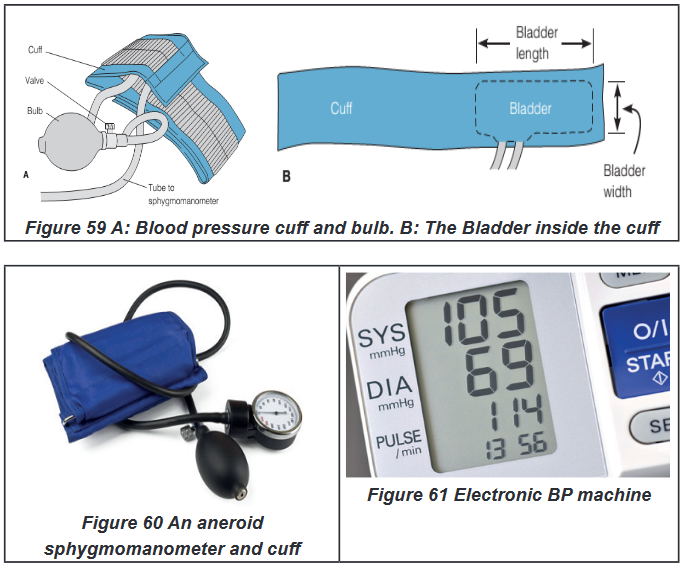
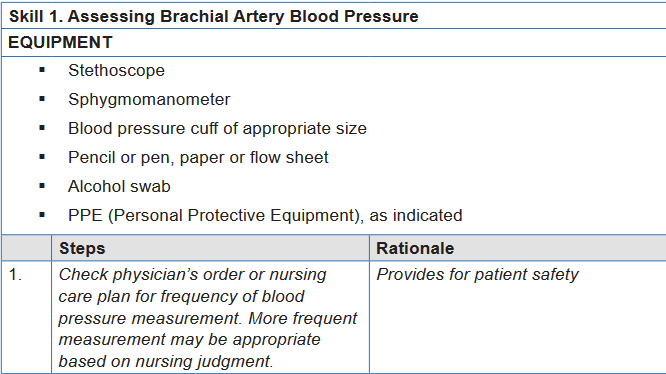
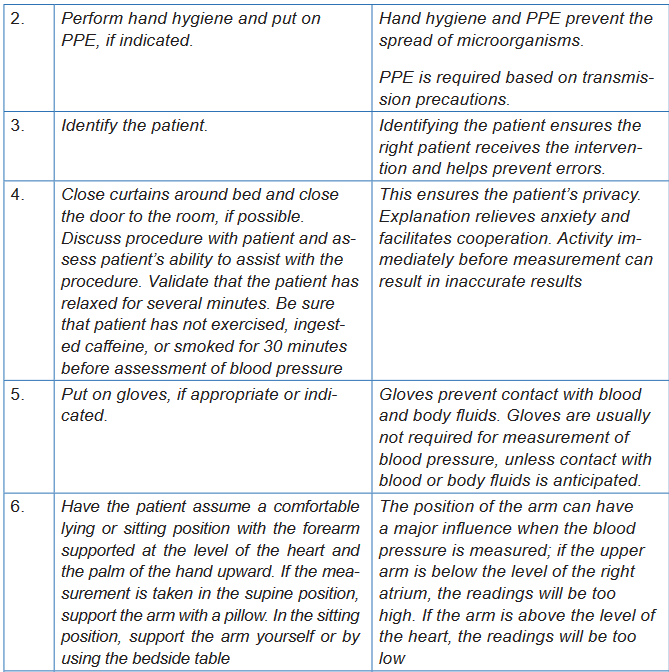
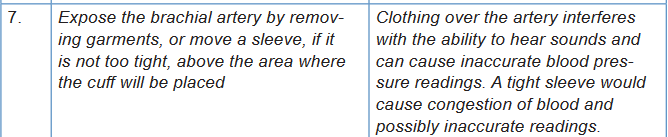
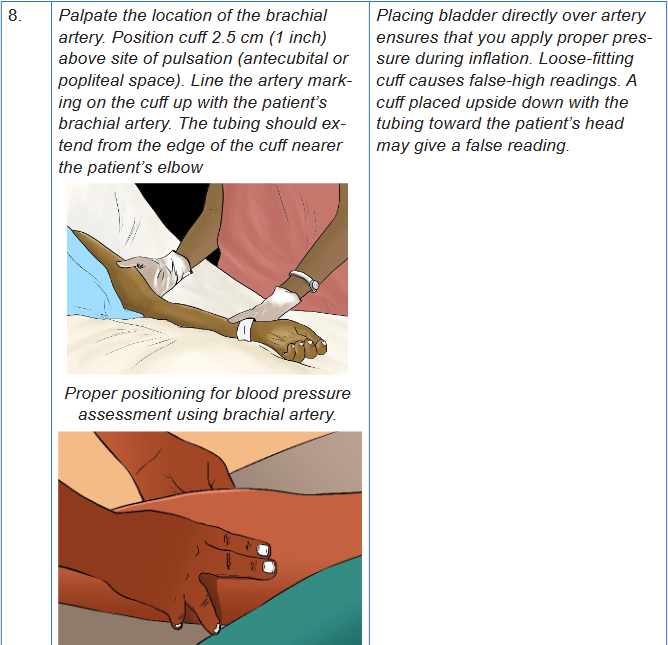
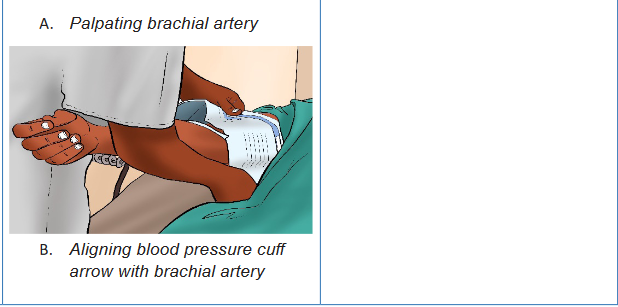
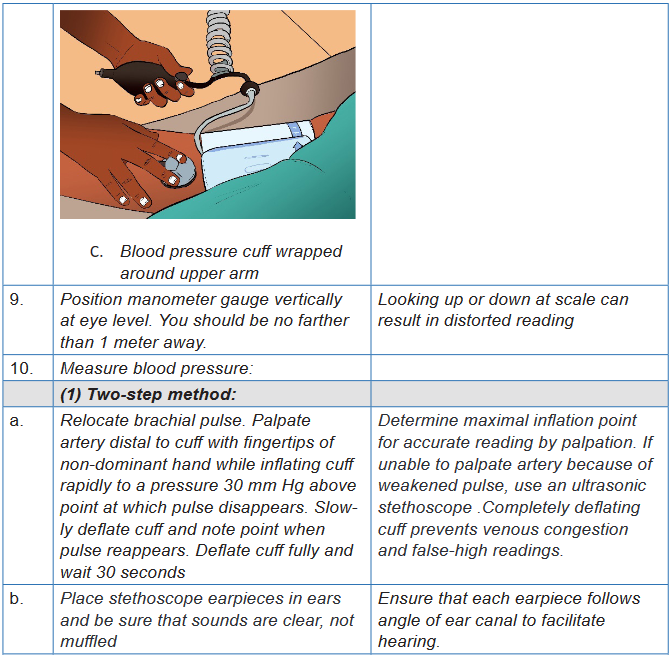
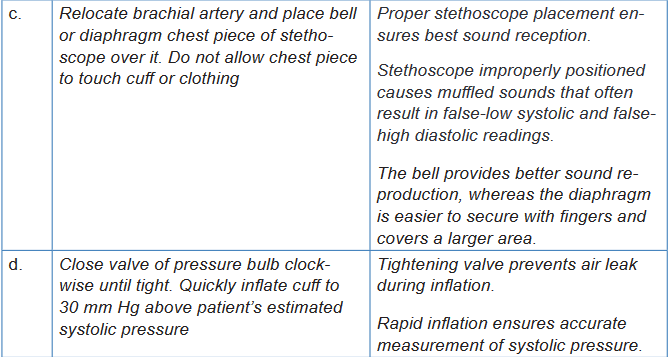
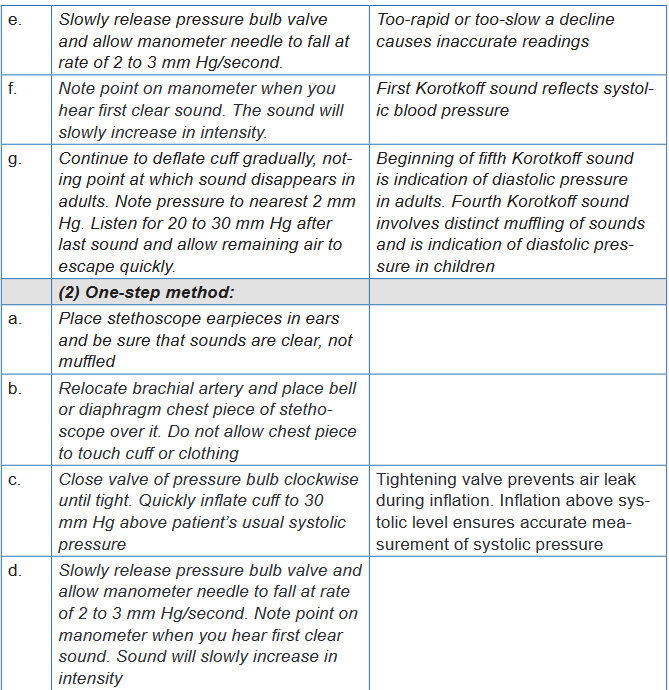
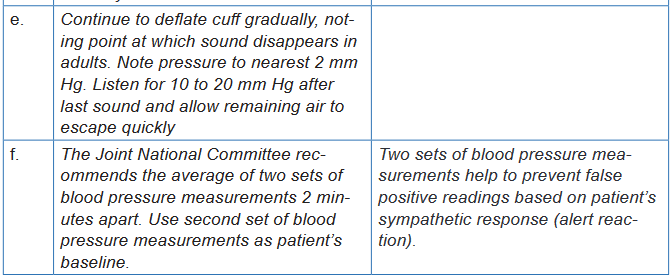
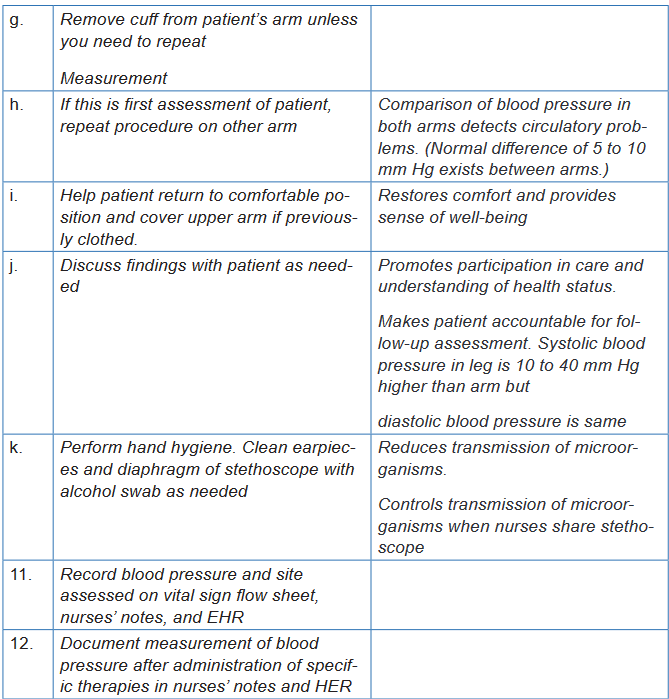
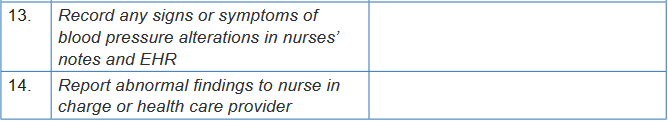
Self -assessment 3.4.
For Blood pressure overview:
1) What is the difference between systolic and diastolic blood pressure?
2) What are the five determinants of blood pressure?
3) The following blood pressures in mmHg, taken 6 months apart, were
recorded from adult patients screened by the nurse at the health center.
Which patient should be referred to the physician for hypertension
evaluation?
Patient 1: 120/80, 118/78, 124/82
Patient 2: 128/84, 124/86, 128/88
Patient 3: 148/82, 148/78, 134/86
Patient 4: 154/78, 118/76, 126/84
4) Explain why the blood pressure increases with age?For Blood pressure measurement:
For you to master the technique of blood pressure measurement; go back to
your previous groups of two; let each student measures one more time the
blood pressure of his /her partner. The teacher will be facilitating and observing
each student while carrying out the procedure.
1) Record the results
2) Interpret the results.
3) Communicate results to your partner.3.5. Respiration
Learning activity 3.5.
For overview
Use the provided book of Fundamentals of Nursing to read the materials on
Respiration under the vital signs unit and make a summary note of the following:
1) Definition of Respiration
2) Normal values and abnormal values of Respiration
3) Pathological variations of Respiration
4) (Risk) Factors affecting Respiration
5) Sites of pulse
6) Different methods of Respiration taking or How to assess the Respiration:
7) Basic nursing interventions during abnormal respiration or in case of
respiration alterations?For procedure
Using checklist provided and equipment for respiration rate taking (see checklist);
read all steps of pulse rate taking in order for you to measure correctly the
Respiration rate for your partner. Remember that you need a watch, a pen and
a sheet paper. Go back to your groups of 2 students and each one of you do
the following
• Observe this image of a nurse assessing respirations of the patient.
• Position your pair in the supine or sitting position and
• Measure his/her respiration rate and vice-versa
• Compare your results.
3.5.1. Respiration Overview
Respiration is the interchange of oxygen (O2) and carbon dioxide (CO2) between
the atmosphere and the body and involves both external respiration and internal
respiration.External respiration is the exchange of these gases between the lungs’ alveoli and
the blood found in the capillaries that surround the alveoli.Internal respiration is the process of exchanging gases between the circulating
blood and the tissue cells that make up the body.The movement of air into and out of the lungs is known as ventilation. The
mechanics of respiration involve the act of breathing in, termed as inhalation or
inspiration, and breathing out, described as exhalation or expiration.a. Inspiration
To effect inspiration, the medulla sends an impulse via the phrenic nerves to the
diaphragm muscle and along the intercostal nerves to the intercostal muscles,
telling the muscles to contractThe contraction of the diaphragm causes it to flatten and move downward, while
the contraction of the inter-costal muscles results in pulling the ribs upward and
outward, enlarging the chest cavity.b. Expiration
Once the medulla stops sending the motor impulses to inhale, the intercostal and
diaphragm muscles begin to relax, once again shrinking the thoracic or chest
cavity to the smaller, pre-inhalation state and compressing the lungs. The elastic
connective tissue of the alveoli recoils somewhat like a rubber band, forcing the air
that is mostly CO2 out of the alveoli so that it can be exhaled and returned to the
atmosphere.c. Rate
Each respiration consists of one inspiration and one expiration. Observe the rise
and fall of the chest or abdomen to count the rate.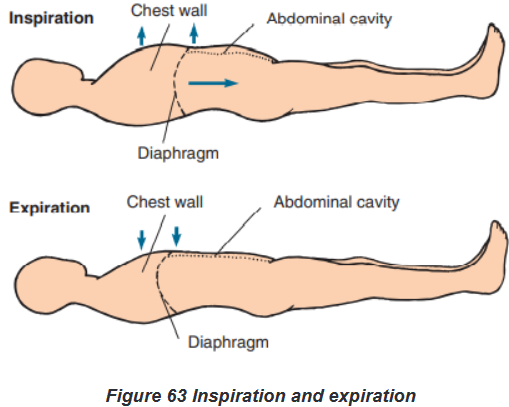
d. Normal and Abnormal values
The normal rate for adults is between 12 and 20 bpm. When the rate, depth,
rhythm, pattern, and respiratory effort fall within normal parameters, the term
eupnea is used to describe the respirations.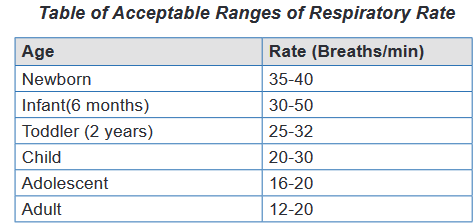
Bradypnea describes a respiratory rate below 12 respirations per minute; when
the rate exceeds 20 respirations per minute, the term is tachypnea. These are
abnormal values. When the breathing rate slows, it results in a decreased intake
of O2 that can result in a deficiency of O2 in the tissues and cells. When respirations
cease or are absent, this is known as apnea. You have only a brief window of 3 to
5 minutes in which to restore respirations before brain damage and death occur.Other things to consider when assessing respiration rate
Assess respiration for:
Rate per minute
Depth
Rhythm
Pattern
Respiratory effortRespiratory Effort
Respiratory effort refers to the amount of work required to breathe. Normally, the
act of breathing is effortless and is performed unconsciously. An individual who is
having labored or difficult breathing is said to be having dyspnea. Another sign
of difficult breathing is use of the accessory respiratory muscles: the neck and
abdominal muscles. It is important to assess which activities result in dyspnea,
document findings in the patient’s record, and report such findings to the supervisor.Some patients find it too difficult to breathe unless positioned in an upright position,
such as sitting or standing. This condition is known as orthopnea. In other words,
we define “Orthopnea” as an abnormal condition in which a person must sit or
stand to breathe deeply or comfortablye. Factors affecting Respiratory rate
Because the heart and lungs work together to provide circulation of nutrients and
oxygen, the factors that affect the heart rate generally affect the respiratory rate as
well. For example, as fever raises the pulse rate, it will also increase the respiratory
rate. Breathing speeds up in an attempt to meet the body’s increased metabolic
needs and to remove excess heat. For every 1°F rise in body temperature, the
respiratory rate increases approximately four breaths per minute. The table below
presents further factors that affect the respiratory rate.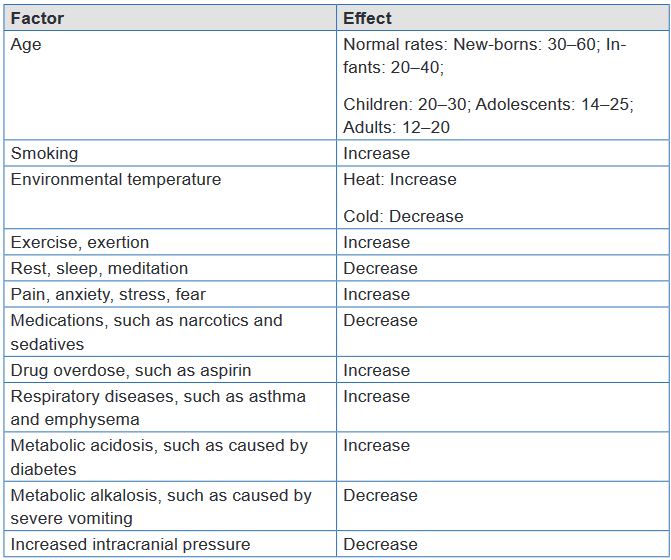
f. Pathological (abnormal) variations of Respiration rate
Some patients find it too difficult to breathe unless positioned in an upright position,
such as sitting or standing. This condition is known as orthopnea. In other words,
we define“Orthopnea” as an abnormal condition in which a person must sit or stand to
breathe deeply or comfortably.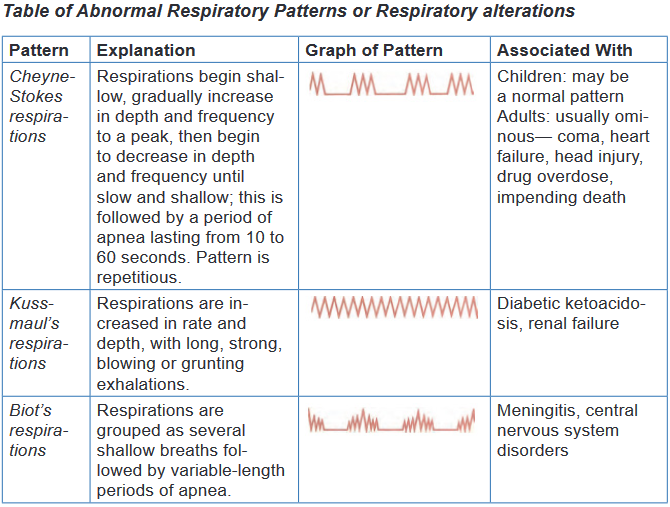
g. Sites of Respiration rate taking
The rate is usually measured when a person is at rest and simply involves counting
the number of breaths for one minute by counting how many times the chest rises.
Note depth of respirations by observing degree of chest wall movement while
counting rate. In addition, assess depth by palpating chest wall excursion or
auscultating posterior thorax after you have counted rate. See Fig.5-8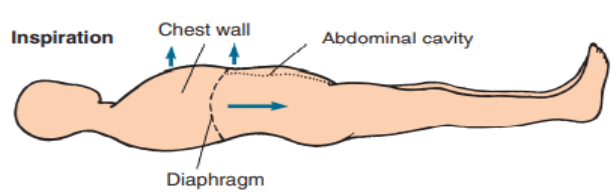
h. Basic Nursing interventions in case of respiratory alterations
In cases of: Apnea: You have only a brief window of 3 to 5 minutes in which to restore
respirations before brain damage and death occur. Call for help to start
Cardio Pulmonary resuscitation (CPR) Dyspnea: Patients with dyspnea experience more distress when lying flat.
Placing the patient in a semi-Fowler or Fowler position facilitates a better
respiratory pattern. Maximal lung expansion can be achieved by having
the patient assume a sitting position, leaning forward over a raised bedside
table with arms resting on the table, in what is called the tripod position.
People who have difficulty ventilating all areas of their lungs, those whose
gas exchange is impaired or people with heart failure may benefit from
oxygen therapy to prevent hypoxia3.5.2. Measurement of respirations
a) Methods of Respiration taking /How to assess Respiration
The only equipment required to assess respiration is a watch.
BOX 3.5.2.
N.B. Because individuals can voluntarily control their breathing for short
intervals of time:
• It is better to assess the respirations without the patient’s awareness.
• This may be accomplished by positioning the patient’s arm across his or
her chest or abdomen.
• Feel for the radial pulse and hold the pulse site while you assess first the
respirations and then the radial pulse. It will appear that you are simply
taking the patient’s pulse, and this will help to distract the patient from
concentrating on his or her breathing.
• While pressing two fingers against the pulse site, count the respiratory
rate for 30 seconds and multiply times two for a 1-minute rate, and then
continue to palpate the radial pulse site to assess the pulse rate.
• If the patient is critically ill or respirations deviate in any manner from
the norm, assess for a full minute.
• Without special equipment, you can only observe the rise and fall of
the chest to provide a subjective measurement of the depth, usually
described as shallow, normal, or deep.b) Respiratory rate assessment procedure
The checklists that will help student to acquire the skills of respiration rate taking
by following all steps and procedures are hereby provided: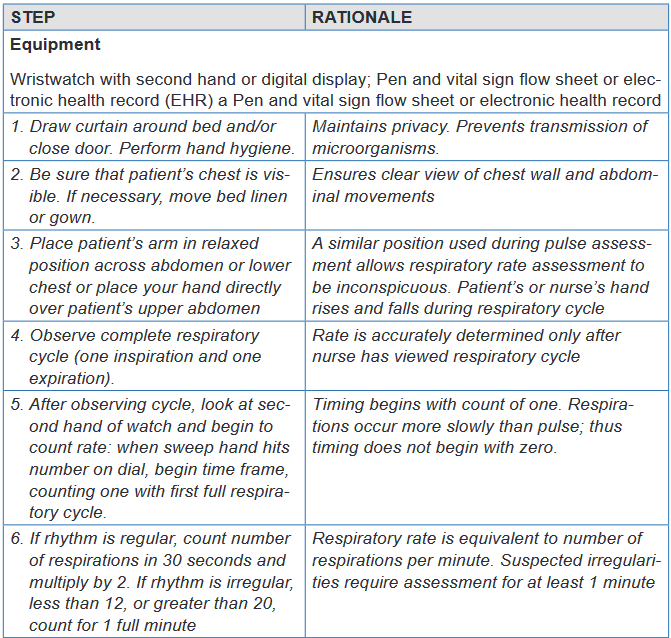
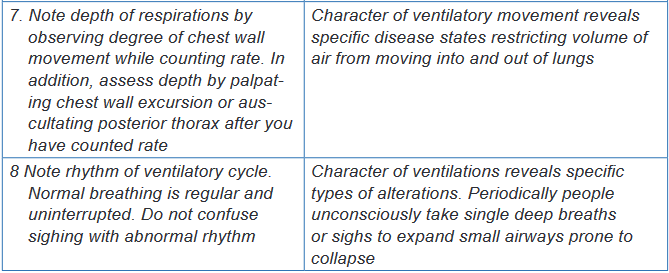
Self -assessment 3.5.
For Overview
1) What are the normal values or acceptable ranges of respiration rate for:
new-born, Infant (6 months), Toddler, Child, adolescent and Adult?
2) Explain the following terms:
a) Bradypnea and tachypnea;
b) Apnea, dyspnea, orthopnea
3) Name at least four abnormal Respiratory patterns
4) Identify at least five factors affecting Respiratory rate.
5) Provide the definition of the terms: Respiration, External respiration and
Internal respiration
6) Indicate the sites used for Respiration rate takingFor Measurement Procedure:
Instructions:
For you to master the technique of Respiration rate taking; going back to your
previous groups of two; let each student takes one more time the respiration
rate of his /her partner.
The teacher will be facilitating and observing each student while carrying out
the procedure by doing the following:
1) Take correctly the Respiration rate of your partner
2) Record the results
3) Interpret them.
4) Communicate results to your partner.3.6. Oxygen saturation (Pulse Oximetry)
Learning activity 3.6.
In small groups of four (4) learners per each, use the provided Fundamentals
of Nursing book and read especially the material and procedural guide on
measurement of oxygen saturation (Pulse Oximetry) under vital signs unit.
After getting an overview information related to the meaning of pulse oximetry,
normal values, factors that may affect the oxygen saturation readings and the
equipment used to measure the oxygen saturation; two learners will pair and
every one will measure the oxygen saturation of his/her partner, write down the
results and interpret themPulse oximetry is the indirect measurement of oxygen saturation and is the
fifth vital sign. During ventilation, oxygen and carbon dioxide diffuse across the
alveolar capillary membrane. Each alveolus is a collection of air sacs surrounded
by a network of capillaries carrying arterial blood from the right ventricle. The
diffusion of these gases occurs in the alveoli and these gases diffuse from the area
of high concentration to the area of low concentration. There is a net movement of
oxygen from the air sacs into the alveolar capillaries, thereby increasing the oxygen
concentration of the blood in these capillaries. This arterial blood has a high carbon
dioxide concentration which diffuses from the alveolar capillaries into the air sacs.Oxygen is carried in the blood as either dissolved oxygen or as oxygen bound
to haemoglobin in red blood cells. The concentration of oxygen dissolved in the
plasma is represented as the partial pressure of arterial oxygen (PaO2). In
contrast, the saturation of arterial oxygen (SaO2) is a ratio of the oxygen bound
to haemoglobin compared with the oxygen-carrying capacity of the haemoglobin.After oxygen diffuses from the alveoli into the pulmonary blood, most of the oxygen
attaches to hemoglobin molecules in red blood cells. Red blood cells carry the
oxygenated hemoglobin molecules through the left side of the heart and out to the
peripheral capillaries, where the oxygen detaches, depending on the needs of the
tissues.A pulse oximeter is a non-invasive device that estimates a person’s arterial blood
oxygen saturation (SaO2) by means of a sensor attached to the person’s finger,
toe, nose, earlobe or forehead (or around the hand or foot of a neonate). The pulse
oximeter can detect hypoxaemia before clinical signs and symptoms such as
cyanosis (dusky/darker) skin colour and dusky nail bed colour) develop. Oxygen
saturation assessed using the invasive approach is documented as SaO2 (arterialoxygen saturation); oxygen saturation assessed by pulse oximetry is documented
as SpO2 (peripheral oxygen saturation or tissue oxygenation).The oximeter
calculates the pulse oxygen saturation (SpO2). SpO2 is a reliable estimate of SaO2.
More specifically, SpO2 is the percentage of oxygenated hemoglobin (hemoglobin
containing oxygen) compared with the total amount of hemoglobin in the blood.
Normally SpO2 is between 95% and 100%; however, in patients with extensive
respiratory disease such as chronic obstructive pulmonary disease (COPD), SpO2
greater than 90% may be an acceptable baseline.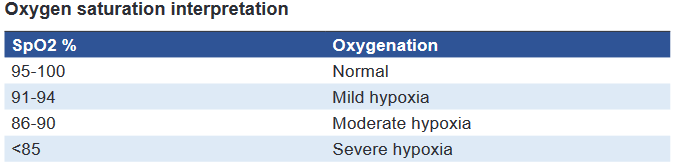
Note: Oximetry measurements should always be interpreted in conjunction with
other patient factors, including signs and symptoms of hypoxiaThe pulse oximeter’s sensor has two parts: (a) two light-emitting diodes (LEDs)—
one red, the other infrared—that transmit light through nails, tissue, venous blood,
and arterial blood; and (b) a photodetector placed directly opposite the LEDs (e.g.,
the other side of the finger, toe, or nose). The photodetector measures the amount
of red and infrared light absorbed by oxygenated and deoxygenated hemoglobin in
peripheral arterial blood and reports it as SpO2.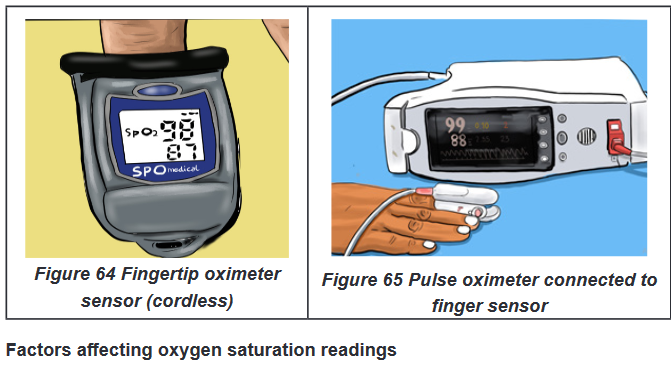
Hemoglobin. If the hemoglobin is fully saturated with oxygen, the SpO2will appear
normal even if the total hemoglobin level is low. Thus, the person could be severely
anemic and have inadequate oxygen to supply the tissues but the pulse oximeter
would return a normal value.Circulation. The oximeter will not return an accurate reading if the area under the
sensor has impaired circulation, such as occurs in peripheral vascular disease or if a
person is very cold. Other factors that result into reduction of pulse volume (reduction
of arterial pulsations) will also affect the oxygen saturation reading. Such factors
are peripheral vascular disease (atherosclerosis), hypothermia, pharmacological
vasoconstrictors (epinephrine, phenylephrine, and dopamine), low cardiac output
and hypotension, peripheral edema, tight probe (will record venous pulsations in
the finger that compete with arterial pulsations).Activity. Shivering or excessive movement of the sensor site may interfere with
accurate readings.Dark-colored nail polish or discoloration of the nail bed. False readings
typically arise when a person is wearing dark colored nail polish or if the nail bed
is discolored by a subdermal hematoma or other sources of nail bed discoloration,
such as nicotine stains.Carbon monoxide poisoning. Pulse oximeters cannot discriminate between
hemoglobin saturated with carbon monoxide versus oxygen. In this case, other
measures of oxygenation are needed.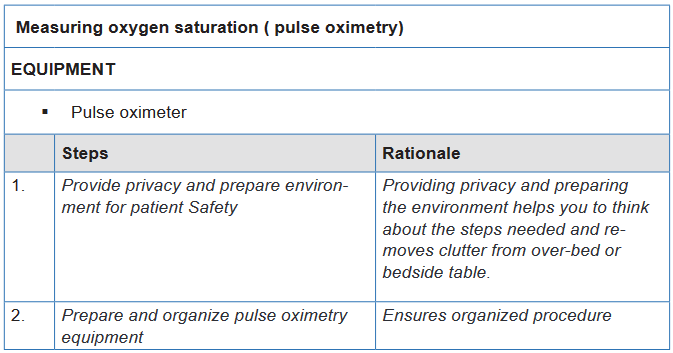
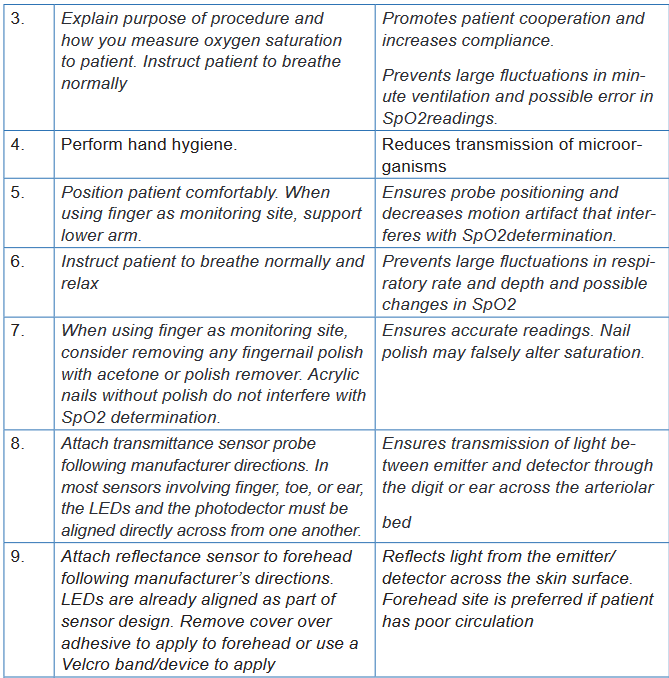
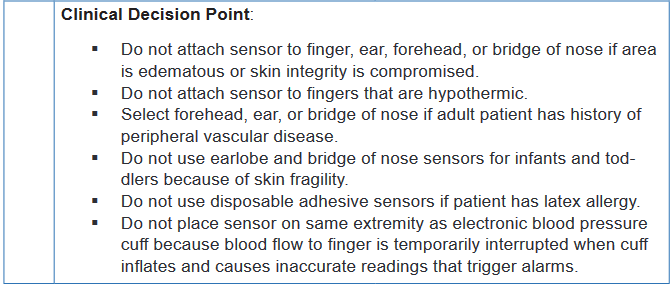
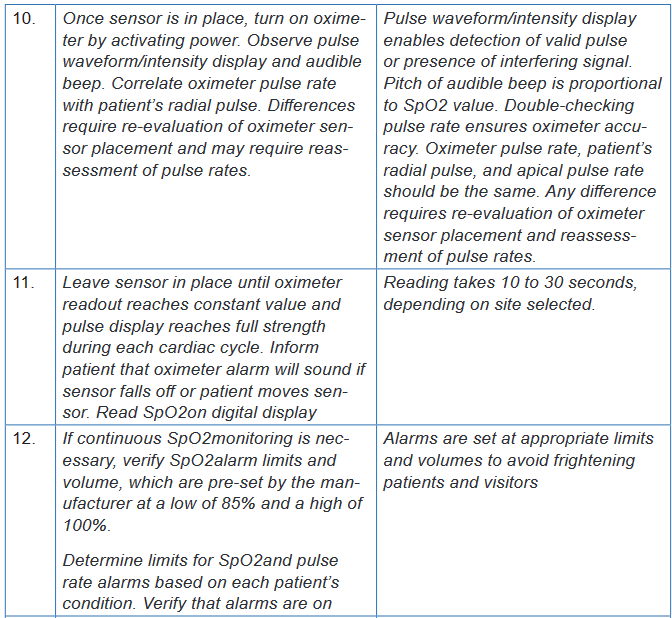
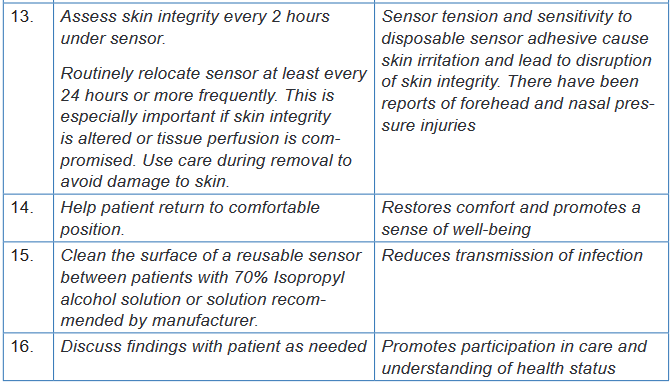
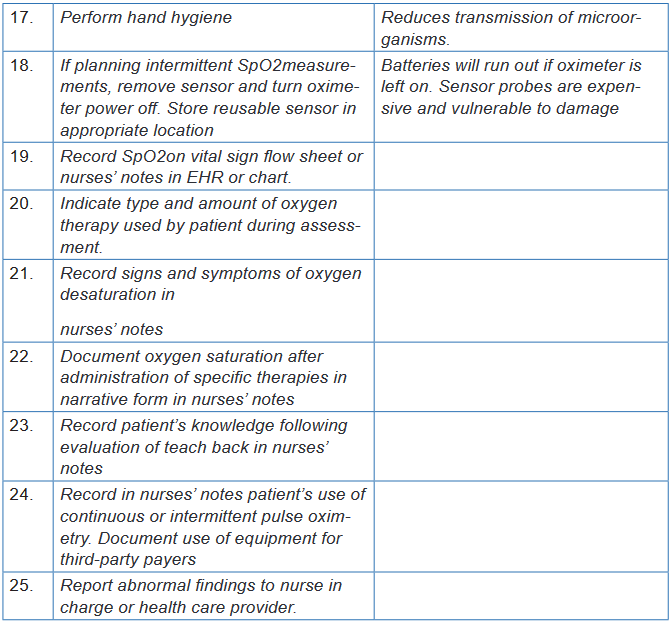
Self-assessment 3.6.
An Associate Nurse (AN) reports to the charge nurse that a patient’s pulse
oximeter machine continues to alarm with a reading of 88%. The charge nurse
enters the room and assesses for signs and symptoms of alterations in oxygen
saturation and finds none.
1) What action does the nurse take next?
1) Remove the current machine from service and ask the AN to use
another pulse oximeter device
2) Verify that the patient’s oxygen device and flow are correct
3) Verify that the oximeter sensor is intact and the skin under the sensor
is dry
4) Notify the health care provider immediately
2) What are the signs and symptoms of alterations in oxygen saturation?3.7. Parameters
Learning activity 3.7.
Observe the images above provided in your textbook under the vital signs
unit and parameters and after reading the sub-topic on Weight and Height
measurement; make a summary note of the following:
1) Definition of two parameters (Height and Weight)
2) Importance of Measuring Height and Weight
3) Specific reasons for weighing both a child and an adult
4) Identify material /equipment used to measure weight and HeightUsing procedural guide provided and equipment/Materials for Weight and
Height measurement; read all steps in order for you to measure correctly the
Weight and Height for your partner in the previous groups of two students. Go
back to your groups and each one of you do the following:
i. Position your partner in position
ii. Measure his/her Weight and Height and vice-versa
iii. Compare your results3.7.1. Weight and Height overview
Introduction and importance of weight and height
Measuring height and weight is as important as assessing the client’s vital signs.
Routine measurement provides data related to growth and development in infants
and children and signals the possible onset of alterations that may indicate illnessin all age groups. The client’s height and weight are routinely taken upon admission
to acute care facilities and during visits to prescribing practitioners’ offices, clinics,
and other health care settings.a) Weight
Weight is the quantitative expression of body that indicates the state of growth and
health measured in kg or grams.Materials/Equipment: A well weighing scale (for adults); Baby Weighing Machine
or Salter balance, a pen and weight recording flow sheetThe Purpose of weight measurement
The purpose is to obtain accurate weight of the patient, to aid in accurate diagnosis
of the patient’s condition, to evaluate the patient’s response to treatmentSpecific reasons for weighing
In a child: reasons are to follow up a good growth, to appreciate the nutritional
state, to follow the evolution of an illness, and to calculate some doses of medicineIn adult: reasons are to evaluate the patient’s general state, to help in the orientation
of the diagnosis, to inform on the evolution of the illness, to calculate doses of some
medicines, to follow up the evolution of treatment and to follow up the pregnant
womanb) Size/Height
It is the measurement from head to toe that indicates the state of growth and health
and is commonly expressed in centimeters (cm), or meters (m). In some countries;
measurement of height is also expressed in inches (in.), feet (ft).Guidelines:
The scale for measuring height, calibrated in either centimeters or meters,
is usually attached to a standing weight scale.
The metal rod attached to the back of the scale should be extended to
gently rest on top of the client’s head, and the measurement should be read
at eye level.
Have the patient’s shoes/slippers removed while taking height to avoid any
variations in the reading
If thick object is placed on the top of head at right angle to the scale indicating
the reading, note the bottom reading of the object.
The nurse should ask the client to stand erect on the scale’s platform.Equipment/Materials
A scale for measuring height
A standing weight scale.
The metal rod
Pen and Height recording flow sheetIndications:
Follow up of child growth
To measure the nutritional status.BOX 3.7.1.
Height increases gradually from birth to the pre-pubertal growth spurt. Girls
usually reach their adult height between the ages of 16 and 17 years, whereas
boys usually continue to grow until the ages of 18 to 20 years. The older adult
usually decreases in height as a result of a gradual loss of muscle mass and
changes in the vertebrae that occur in condition such as osteoporosis (a
process in which reabsorption exceeds accretion of bone).Use the patient’s weight and height measurements to calculate the patient’s
BMI. Weight in kilograms Body mass index height in meter (Additional
information to the teacher)Rationale: BMI is an indicator of total body fat stores in the general population
and provides a more accurate weight calculation than weight measurement
alone. In addition, it provides an estimation of risk for diseases, such as heart
disease, diabetes, and hypertension.3.7.2. Measurement of Weight and Height Procedures
a) Conditions required for weighing:
i. In adult:
The weighing scale must be well-designed and well controlled, that means
graduated on zero: very important!
It must be put on a plane surface
The patient must remove the shoes and must be undressed while only
keeping light clothes in order to reduce the weight He must stand up, free hands and does not hold any object
Weight must be taken regularly
ii. In childThe weight of a child can be taken, according to age with: Baby Weighing Machine
or Salter balance. If it is not available:
Weigh the mother and the child and to note the weight;
Weigh only mother
Then make the difference between the first weight and the second, what
corresponds approximately to the child’s weight.
c) Procedure for weight and height measurementi. Equipment /Materials:
A scale for measuring height
A standing weight scale.
The metal rod
Pen and Height recording flow sheetWhen measuring an infant’s height,
The nurse should place the infant on a firm surface.
Extend the knees, with the feet at right angles to the table.
Measure the distance from the vertex (top) of the head to the soles of the
feet with a measuring tape.N.B. The procedure usually requires two nurses, one to hold the infant still and
the other to measure the length. If the nurse needs to perform the measurement
without assistance, an object should be placed at the infant’s head, the infant’s
knees should be extended, and a second object should be placed at the infant’s
feet. Lift the infant and measure the distance between the two objects.For Adults measurement,
With shoes off, and standing erect
Measure the patient’s height using a wall-mounted measuring device or
measuring pole.
Compare height and weight with recommended average weights on a
standardized chart.Rationale: Ratio of height and weight is a general assessment of overall health,
hydration, and nutrition.Self-Self -assessment 3.7.
For Overview: Section (a)
1) Define the two parameters: Weight and Height/size
2) Explain the Purpose of weight measurement
3) What are the specific reasons for weighing both a child and an adult
4) List all materials used measuring Weight and Height both for Adult and
a childFor Weight and Height Measurement Procedure: Section (b)
Instructions:
For you to master the technique of Weight and Height measurement; going
back to your previous groups of two; let each student measures one more time
the Weight and Height of his /her partner. Be familiar with the use of the check-
list provided to you.End unit assessment 3
Question one
Mr. K is 25 years old male from a low income family. He consults the nearest
health center complaining of vomiting and diarrhea. During initial assessment
data collection, Mr. K tells to the nurse that it is the 3rd day having both vomiting
and diarrhea (vomiting: 4 times a day and diarrhea: 6 times a day), severely
nauseated and dizzy, tolerating sips of clear fluid. No past history of medications
and illnesses.
Think about these data from Mr. K and try to answer the following questions:
1) What infection control measures should the nurse implement?
2) What route should be used to measure body temperature for Mr. K?
3) Identify in the above case study the factors that may affect the pulse
and blood pressure of Mr. KQuestion two
During physical examination of Mr. K, the nurse measures his vital signs and
parameters and notes the following findings: Temperature: 102.20 F, Pulse: 120
bpm (radial), BP: 98/68 mmHg, RR: 22 bpm irregular rhythm, Sp02: 94%, Weight:
53kg, Height: 174cm. Reflect on these findings and respond to the following
questions:
1) Which findings are considered abnormal for Mr. K? What medical
terminologies are used to define/label the abnormal findings?
2) The nurse uses the two-step method of blood pressure assessment to
obtain accurate measurements for Mr. K. The nurse is explaining the
steps of this procedure to the associate nurse. Place the steps in correct
order:
a) Place stethoscope in ears and place the diaphragm of stethoscope
over the brachial artery
b) Palpate brachial artery while inflating blood pressure cuff 30mmHg
over the pulse disappearance.
c) Note point where you hear first Korotkoff sound.
d) Deflate cuff fully and wait 30 seconds
e) Apply blood pressure cuff 2.5cm above brachial artery.
f) Continue to deflate cuff until sound disappears.
g) Quickly inflate cuff to 30 mm Hg above patient’s estimated systolic
pressure
h) Slowly deflate cuff and note point when pulse reappears.UNIT 4: NOSOCOMIAL INFECTIONS CONTROL AND PREVENTION
Key Unit Competence
Apply correctly the infection prevention and control techniques for nosocomial
infections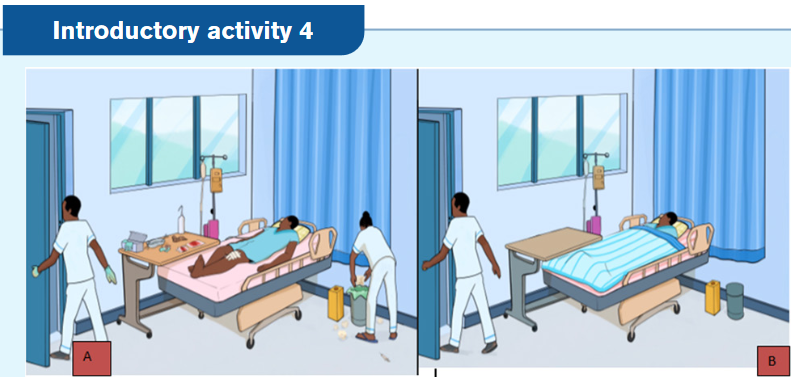
1) Is it perfect to maintain patient room A like this?
2) On your view, what should be done by the nurse room A and B if any?
3) What are potentials risks associated to this kind of patient arrangement A?
4) What do you predict to learn from this unit?4.1. Overview on nosocomial infections
Learning activity 4.1.
Observe the picture below:
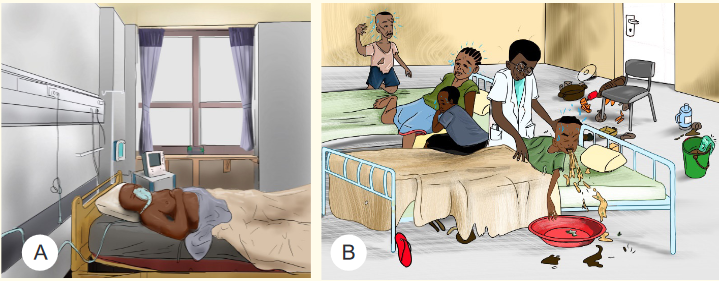
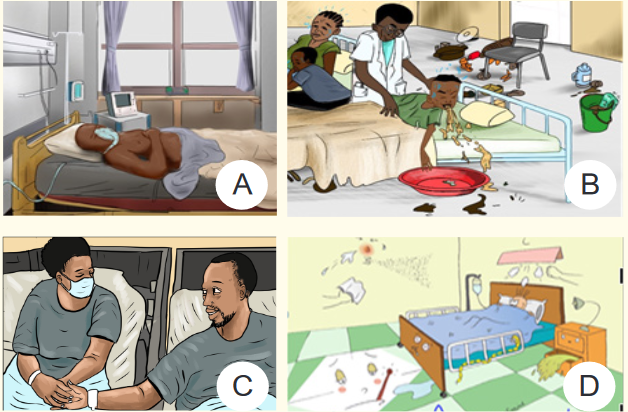
1) Analyze the pictures above and identify the probability of transmitting
diseases among them (A, B, C and D.)
2) Based on the picture above, what are the possible risk factors of nosocomial
infection for patient A and B?Nosocomial infection is a term that encompasses infections contracted in all health
care settings. Nosocomial infections also known as healthcare - associated infec-
tions (HCAI) or hospital acquired infections are defined as localized or system in-
fection, occurring at least 48 hours after hospital admission, that was not present or
incubating at the time of admission. They are those infections that occur in patients
or healthcare workers either as a direct result of healthcare intervention (such as
medical or surgical treatment) or from being in contact with a healthcare setting.4.1.1. Risk factors for nosocomial infections
The risk factors for nosocomial infection include hospitalized patients with under-
lying disease like diabetes, high blood pressure, HIV/AIDs, malnutrition, etc.; age
particularly elderly and young aged people, invasive devices and procedures
such as IV lines, surgery, intensive care; emergency hospital admission , previous
exposure to some drugs and previous hospital admission add to the risk.4.1.2. Causes of nosocomial infections
The most common pathogens that cause nosocomial infections are Staphylococ-
cus aureus, Pseudomonas aeruginosa, and E. coli. Nosocomial infections are not
just limited to bacteria; certain fungi such as Candida albicans and aspergillus, as
well as, viruses such as Respiratory Syncytial Virus and influenza have also been
implicated in a number of hospital acquired infections.4.1.3. Transmission of nosocomial infections
These infections are transmitted through direct or indirect contact from the hospital
staff, other patients or visitors; inadequately sterilized instruments; disease vector
carrying and transmitting an infectious pathogen, or blood; aerosol droplets from
other ill patients or even the food or water provided at hospitals.Direct-contact transmission involves a direct body surface-to-body surface con-
tact and physical transfer of microorganisms between a susceptible host and an
infected or colonized person, such as when a person turns a patient, gives a patient
a bath, or performs other patient-care activities that require direct personal contact.
Direct-contact transmission can also occur between two patients, with one serving
as the source of the infectious microorganisms and the other as a susceptible host.
Indirect-contact transmission involves contact of a susceptible host with a contam-
inated intermediate object, usually inanimate, such as contaminated instruments,
needles, or dressings, or contaminated gloves that are not changed between patientsSelf-assessment 4.1.
1) Define nosocomial infections
2) Explain the causes of transmission of nosocomial infections
3) What are risk factors of nosocomial infections?
4) Discuss the mode of transmission of nosocomial infections4.2. Concepts of Asepsis and Antisepsis
Learning activity 4.2.
Observe the picture below:
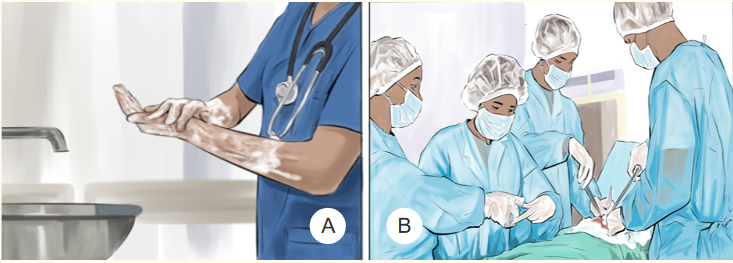
1) Observe the activity that is being done on the picture A and tell its importance.
2) Discover the kinds of clothes and items that the people in picture B are
wearing.
3) Why the people in the picture B are wearing like that?Regardless of where nurses practice, preventing the transmission of microorgan-
isms is a concern of all health care professionals. One way that nurses accomplish
this goal is by asepsis.Asepsis means the absence of germs, such as bacteria, viruses, and other micro-
organisms that can cause disease. Healthcare professionals use aseptic technique
to protect patients from infection.Antisepsis is the practice of using antiseptics (substance that stops or slows down
the growth of microorganisms) to eliminate the microorganisms that cause disease.4.2.1. Principles of Asepsis
The principles of asepsis include the following:
1. Use only sterile items within a sterile field;
2. Sterile (scrubbed) personnel are gowned and gloved;
3. Sterile personnel operate within a sterile field (sterile personnel touch only
sterile items or areas, unsterile personnel touch only unsterile items or areas);
4. Sterile drapes are used to create a sterile field
5. All items used in a sterile field must be sterile
6. All items introduced onto a sterile field should be opened, dispensed, and
transferred by methods that maintain sterility and integrity
7. A sterile field should be maintained and monitored constantly
8. Surgical staff should be trained to recognize when they have broken technique
and should know how to remedy the situation.4.2.2. Difference between Medical and Surgical asepsis
The term medical asepsis refers to practices performed to prevent the spread of
infection. It is also sometimes described as using clean technique. These practic-
es, or techniques, include performing hand hygiene, maintaining a clean patient
environment, using standard precautions, and using transmission-based pre-
cautions when necessary.Medical asepsis is different than surgical asepsis, which refers to maintaining
a sterile environment such as that found in operating rooms. Sterile technique
means performing procedures in such a way that no pathogens will enter the pa-
tient’s body when you insert tubes or give injections.4.2.3. Levels of asepsis (Cleaning, Disinfection and Sterilization)
a) Cleaning
Cleaning is the process of removing unwanted substances using water and soap,
such as dirt, infectious agents, and other impurities, from an object or environment.
Cleaning removes dirt, dust, crumbs, and germs from surfaces or objects. When
you clean, you will likely use soap (or detergent) and water to physically clean off
the surfaces and objects. This may not necessarily kill the germs. But since you
removed some of them, there are fewer germs that could spread infection.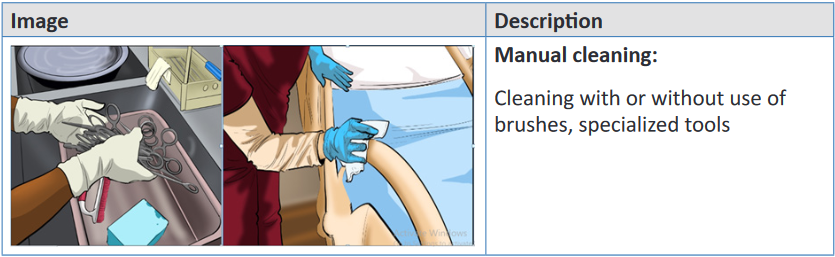
b) Disinfection
Disinfection is a process of using chemicals (disinfectants) to kill germs on surfaces
and objects. Some common disinfectants are bleach and alcohol solutions. You
usually need to leave the disinfectant on the surfaces and objects for a certain pe-
riod of time to kill the germs. Disinfecting does not necessarily clean dirty surfaces
or remove germs.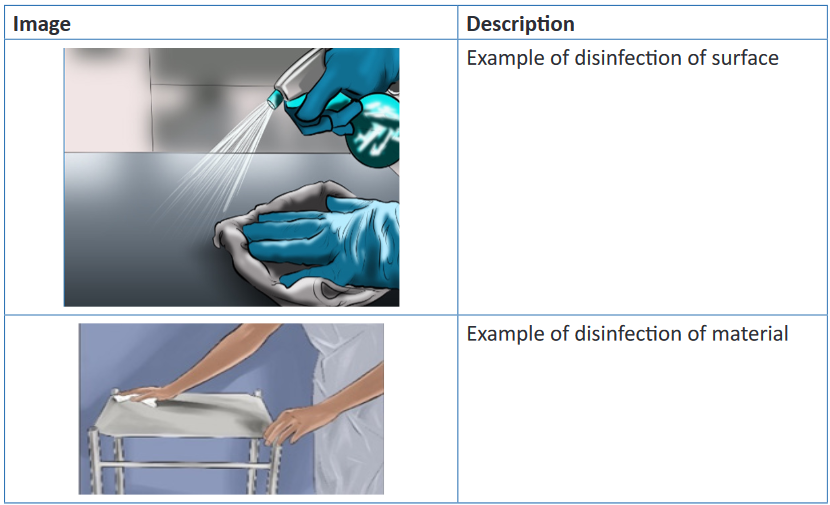
c) Sterilization
Sterilization refers to any process that removes, kills, or deactivates all forms
of life (in particular referring to microorganisms such as fungi, bacteria, spores,
unicellular eukaryotic organisms such as Plasmodium, etc.Note: After sterilization, an object is referred to as being sterile or aseptic.
Common methods of sterilization include physical methods and chemical
methods. Physical methods include dry heat, steam, radiation, and plasmas.Chemical methods include, for example, ethylene oxide, propylene oxide, chlorine
dioxide, ozone gases, and a variety of chemicals in liquid and vapor form, such as
glutaraldehyde, hydrogen peroxide, and peracetic acid.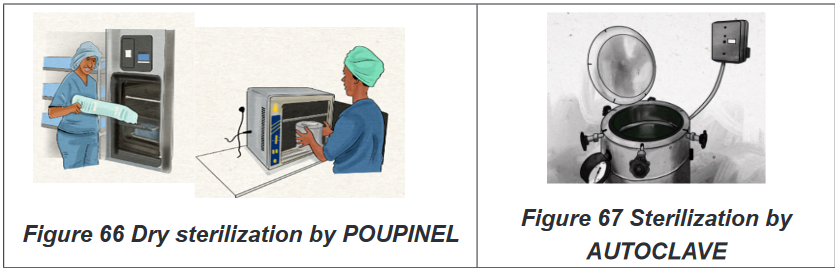
Self-assessment 4.2.
1) Differentiate asepsis and antisepsis
2) Describe the levels of asepsis4.3. Prevention and control of nosocomial infections
Learning activity 4.3.
You are working at hospital setting as associate nurse and you have a patient
suffering from malaria with high fever. He is receiving IM Arthesunate injection
and paracetamol tablets. After two days, the health professionals decided to
perform Covid19 test which become positive.
1) How are you going to behave in order to prevent you from contamination
when you are going to give the above said patient treatment?Prevention and control of infections are important concerns for all types of health
care agencies, and good infection control practices generate cost savings and im-
proved outcomes for patients.According to the World Health Organization (WHO), infection prevention and con-
trol (IPC) is a scientific approach and practical solution designed to prevent harm
caused by infection to patients and health workers.4.3.1. General information on WHO Standard precautions of
infection controlStandard precautions of nosocomial infection are the minimum set of actions
that are to be undertaken in every care environment and to be used for every care
procedure, every time. They are performed with all patients, whether or not an in-
fection has been diagnosed.They protect the health-care worker from possible transmission of illnesses spread
through contact with infected blood, such as hepatitis B, hepatitis C, and HIV. They
also protect patients from the possible spread of pathogens from one patient to
another.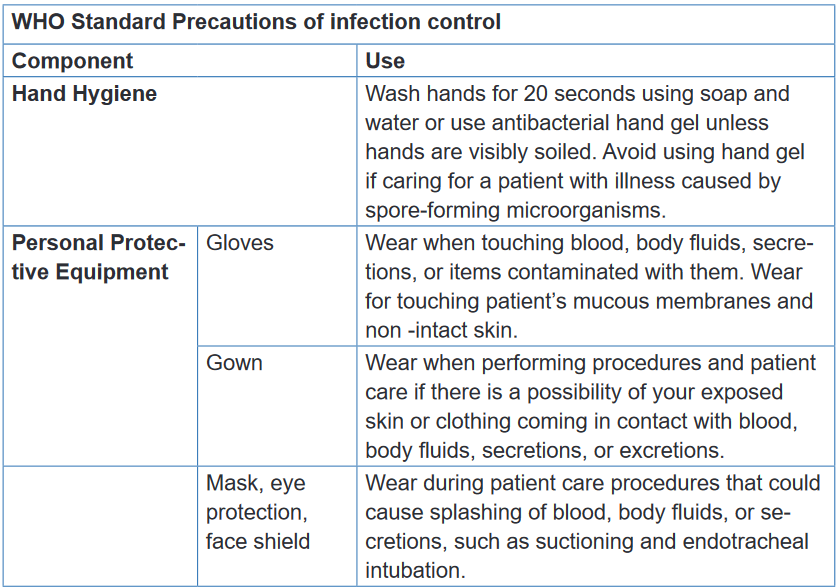
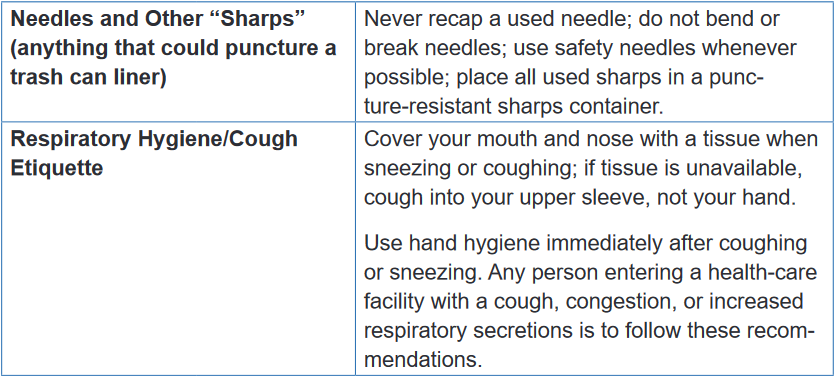
Self-assessment 4.3.
1) Which of the following are basic standard precautions for infection
control?(choose one answer)
a) Hand hygiene
b) Personal protective equipment and clothing
c) Safe handling of sharps
d) All of these are basic standard precautions2) What is the purpose of wearing gloves and gowns? (Check all that
apply).
c) Protect the healthcare worker
d) Prevent transmission of pathogens
e) Reduces hand washing requirements
f) Looks professional and identifies healthcare staff
3) What is importance of standards precautions of nosocomial infection?4.4. Overview of hand hygiene
Learning activity 4.4.
Observe the pictures and answer the questions below:

1) What are similarities and differences between picture A and B?
2) In your point of view, what is importance of the actions in pictures A and B?Hand hygiene is a general term referring to any action of hand cleansing. The term
hand rubbing is used when using an alcohol-based hand rub or hand washing with
soap and water aimed at reducing or inhibiting the growth of micro-organisms on
hands.4.4.1. When to perform hand hygiene
Hand hygiene are indicated before and after touching the patient; before handling
an invasive device for patient care regardless of whether or not gloves are used;
after contact with body fluids or excretions, mucous membranes, non-intact skin,
or wound dressings; if moving from a contaminated body site to another body site
during care of the same patient; after contact with inanimate surfaces and objects
(including medical equipment) in the immediate vicinity of the patient; after removing
sterile or non-sterile gloves; before handling medication or preparing food.4.4.2. Benefits of hand hygiene
Germs from unwashed hands can be transferred to other objects, like handrails,
table tops, or toys, and then transferred to another person’s hands. Hand hygiene
is the most important measure to avoid the transmission of harmful germs between
people and prevent health care-associated infections.Note: As much as it is necessary, perform hand hygiene. Hand rubbing never
replaces hand washing. Whenever possible, do hand washing. Soap andalcohol-based hand rub should not be used at the same time.
4.4.3. Hand rubbing and hand washing
Hand hygiene is the single most important procedure for preventing the transmission
of diseases and infections. It can be done through hand rubbing and/ or hand
washing. (For more, refer to the UNIT 2: Subtopic 2.1. )a) Hand rubbing
Hand rubbing is a hand hygiene technique with alcohol-based formulation (antiseptic
hand rubbing). It last between 20-30 seconds. The equipment to be used in hand
rubbing is the following: antiseptic hand rub: Alcohol-based, waterless, antiseptic-
containing emollientHand rubbing involves the following steps: (1) Apply an ample amount of product
to palm of one hand; (2) Rub hands together, covering all surfaces of hands and
fingers with antiseptic; (3) Rub hands together for several seconds until alcohol is
dry; (4) Allow hands to dry before applying gloves. (Refer to the UNIT 2:, Subtopic
2.1. )b) Hand washing
Action of performing hand hygiene using soap and water for the purpose of
physically or mechanically removing dirt, organic material, and/or microorganisms.
The duration of the entire procedure is 40-60 seconds.Equipment of hand washing include easy-to-reach sink with warm running water,
antimicrobial or non-antimicrobial soap, Paper towels or air dryer, Disposable nail
cleaner (optional).Self-assessment 4.4.
1) What are benefits associated with hand washing?
2) As a future associate nurse, when to perform hand washing?
3) What is the difference between hand rubbing and hand washing?4.5. Personal protective equipment (PPE)
Learning activity 4.5.
See the image below and answer the related questions:

1) What are you seeing on the image above?
2) On your view, what is importance of each item on this image?Personal protective equipment is clothing and equipment that is worn or used in
order to provide protection against hazardous substances or environments. This
can include items such as safety helmets; ear protection; high visibility clothing;
safety footwear and safety harnesses; thermal, weather and waterproof clothing;
respiratory protective equipment.4.5.1. Gloves
The use of gloves does not replace the need for hand hygiene by either hand
rubbing or hand washing. The gloves should be worn when it can be reasonably
anticipated that contact with blood or other potentially infectious materials, mucous
membranes or non-intact skin will occur. After caring for a patient all the gloves
should be removed and always the gloves are single use.It is important to wear gloves when working with hazardous chemicals and other
materials because they protect our hands from infection and contamination.
Protective gloves should be selected on the basis of the hazards involved. Rubber
gloves protect against mild corrosive material.4.5.2. Gown
Nurses wear sterile gowns when assisting at the sterile field in the operating room,
delivery room, and special treatment areas. Surgical gowns serve to protectpatients from microorganisms carried by the surgical team or patients themselves
and protecting healthcare providers from contact with infectious microorganisms
harbored by the patient.It allows the nurse to handle sterile objects and also be comfortable with less
risk of contamination. The sterile gown acts as a barrier to decrease shedding
of microorganisms from skin surfaces into the air and thus prevents wound
contamination. A fluid-resistant gown or protective apron is worn to keep the nurse’s
clothing clean when potential exists for body substances to splash.The main difference between a gown and an apron is that a gown covers the entire
torso and goes all the way down to the healthcare worker wrists.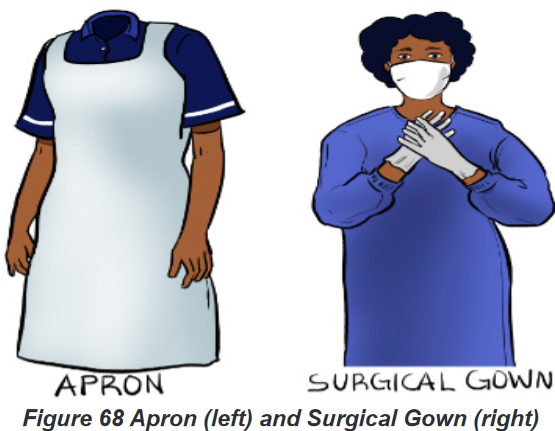
4.5.3. Mask
Masks help protect clients and healthcare personnel from respiratory infections and
certain communicable diseases.
Considerations in mask use include (1) put on the mask before the gloves;(2) do
not touch the mask until it is to be removed; (3) the mask must be changed when
moist or soiled; (4) wash hands and remove gloves before removing the mask; (5);
handle masks by the strings or elastic only; (6) dispose of a used mask immediately;
do not leave a mask dangling around the neck.4.5.4. Eye protection (goggles) and face shield
Safety goggles are important because they protect health care providers from
accidental entry of blood and other microorganisms in the eyes. They also allow
the wearer to handle potentially harmful chemicals and biological without fear ofdamaging their eyes. Safety goggles can also help to protect an individual from
harm to the eye from physical trauma.Wear goggles with side and forehead shields if any danger exists that a client’s
body fluids may splash or spray. Goggles are also available that fit over glasses.
In some types of isolation, disposable goggles are worn. In situations when extra
protection is needed, such as in the operating room, emergency department, or
morgue, full face shields are used. These protect the eyes, as well as the mouth.
The situation dictates the type of eye and mucous membrane protection to be used.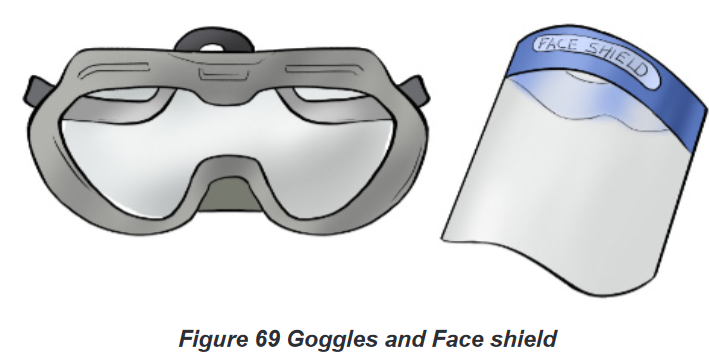
4.5.5. Boots
A pair of safety shoes also known as safety boots is personal protective equipment
(PPE) for foot protection at workplaces. Protective footwear worn in the workplace is
designed to protect the foot from physical hazards such as falling objects, stepping
on sharp objects, heat and cold, wet and slippery surfaces, or exposure to corrosive
chemicals.4.5.6. Donning (wearing) of Personal Protective Equipment
Donning involves putting on the required apparel before patient contact and must
be performed in the following order; (1) hand hygiene; (2) put on shoe covers (if
applicable);(3) wear gown; (4) wear mask;(5) put eye or face protection ;(6) and
gloves.4.5.7. Doffing (removing) of Personal Protective Equipment
Personal protective equipment must be removed in the following specified
sequence, to minimize the potential for disease transmission: (1) wash hands, (2)remove gloves, (3) remove mask by touching only the string tied behind the head,(4)
remove eye protection without touching the face, (5) wash hands, (6) remove gown
or apron touching only the inside, turn it inside out, to contain contamination, (9)
properly dispose of all PPE, (10) wash hands.Self-assessment 4.5.
1) The nurse wears a gown when:
a) The patient’s hygiene is poor
b) The nurse is assisting with medication administration.
c) The patient has acquired immunodeficiency syndrome
(AIDS) or hepatitis.
d) Blood or body fluids may get on the nurse’s clothing from
a task that he or she plans to perform.2) Match in the correct order of donning(wearing) Personal Protective
Equipment (PPE)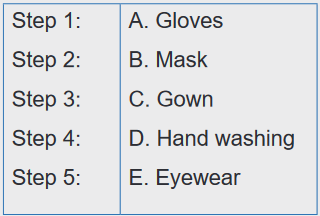
3) Match in the correct order of doffing(wearing) Personal Protective
Equipment (PPE)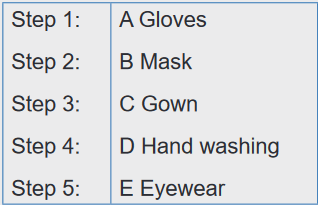
4.6. Respiratory hygiene and cough etiquette
Learning activity 4.6.
Observe the picture below and answer following questions
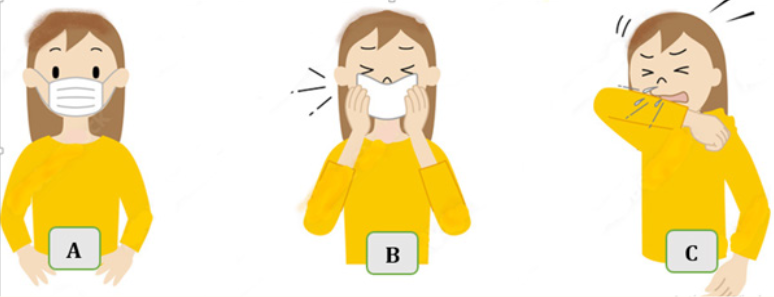
1) What are you seeing on the picture A, B and C?
2) On your view, what are similarities and differences of persons on picture
A, B and C?Respiratory hygiene and cough etiquette are terms used to describe infection
prevention measures to decrease the transmission of respiratory illness (e.g.,
influenza and cold viruses). A respiratory infection is spread when a person who is
infected with a virus coughs or sneezes.
Cough etiquette is a series of actions that should be taken when coughing or
sneezing which are designed to reduce the spread of respiratory illness to others.4.6.1. The actions to respect in respiratory hygiene
In respiratory hygiene everyone should (1) cover the mouth and nose with the tissue,
wear mask or put on elbow when coughing or sneezing; (2)Use tissues and discard
the tissue immediately into a bin; (3)wash hands or use a hand sanitizer every time
touching the mouth or nose; (4) post visual alerts (in appropriate languages) at the
entrance to outpatient facilities instructing patients and persons who accompany
them (e.g., family, friends) to inform healthcare personnel of symptoms of a
respiratory infection when they first register for care and to practice respiratory
Hygiene/cough Etiquette.4.6.2. Importance of respiratory hygiene
Respiratory hygiene and cough etiquette are very important components to protect
self and others from the transmission of respiratory illness. Like hand hygiene,
respiratory hygiene is part of the standard precautions that should be taken to
prevent the spread of disease.Self-assessment 4.6.
1) Respiratory hygiene/cough etiquette includes:
a) Posting visual alerts about signs and symptoms of infection
b) Re-using tissues to help keep costs down
c) Frequent hand hygiene, especially after contact with respiratory
secretions
d) A and C are correct answers2) What is the importance of respiratory hygiene /cough etiquette?
4.7. Sharps Safety/ Safe Injection Practices
Learning activity 4.7.
Observe the pictures and answer questions below:

1) What do you see on the picture A and B?
2) On your view, what are consequences associated with the picture B?Safe injection is injection practice which does not harm the recipient (patient), does
not expose the provider to any avoidable risks and does not result in waste that is
dangerous for the community.Safe injection practice is achieved by administering the injection using a sterile
device (syringe, needle etc.), adopting sterile technique by a qualified and well
trained person and discarding the used devices in a puncture-proof container
specially designed for appropriate disposal. Any breach in the process makes the
injection unsafe.4.7.1. Consequences of unsafe injection
Unsafe injection practices which can transmit Hepatitis B, Hepatitis C, Human
immunodeficiency virus (HIV) and other blood borne pathogens result in substantial
burden of preventable blood borne viral diseases.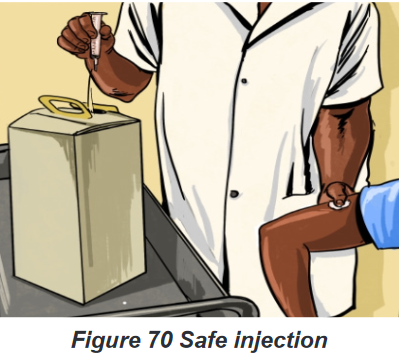
4.7.2. Management of Accidental Needle sticks or Other
ContaminationUnfortunately, the nurse may sustain an accidental stick with a contaminated
needle. If this occurs, follow these procedures:
Wash the area gently with soap and running tap water as soon as possible;
Report the incident to the direct leader and / infection prevention and; control
focal person,
Fill out an incident report,
Blood tests of the client and nurse will usually be performed.The nurse may be required to take medication as post exposure prophylaxis if the
patient has blood transmissible disease or has disappearing without being tested.
If material is splashed into the eyes or mouth, wash with copious amounts of water
and report as above.Self-assessment 4.7.
1) Which of the following is included in the steps for needle stick injuries?
a) Wash needle stick injury with soap and water
b) Report needle stick injury to your supervisor
c) Wash needle stick injury with soap and water and use alcohol
d) A and B are correct answers2) The first step after a needle stick or sharps injury is to
a) Express or suck the wound.
b) Apply caustic agents (e.g., bleach) to the wound.
c) Inject antiseptics or disinfectants into the wound.
d) Gently wash the exposed area with soap and water without
scrubbing.4.8. Sterilization and Disinfection of Patient-Care Items
and DevicesLearning activity 4.8.
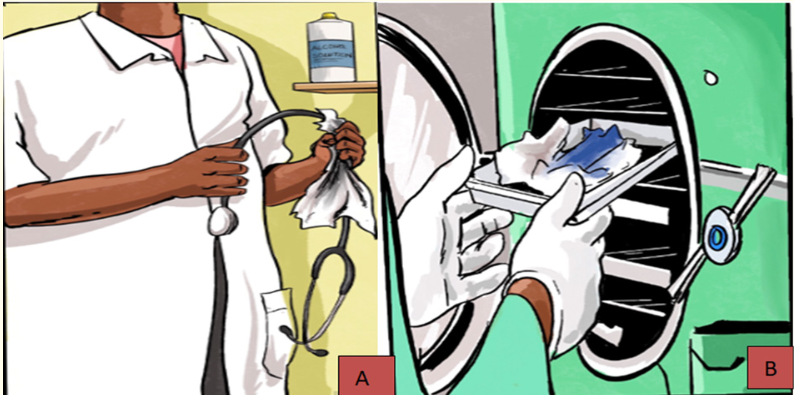
See the picture and answer the questions
1) What is the action done on picture A and picture B?
2) What is the importance of each action?Sterilization and disinfection are the basic components of hospital infection control
activities.The medical device or the surgical instrument that comes in contact with the sterile
tissue or the mucus membrane of the patient during the various processes is
associated with increased risk of introduction of pathogens into the patient’s body.4.8.1. Importance of disinfection
Frequent cleaning and disinfection helps to prevent the spread of germs that
may cause illness. The importance of respecting the proper disinfection is that it
will reduce infections associated with contaminated patient-care items.
The cleaning and disinfection of medical equipment depends on their physical
nature, character of the material it is made up of, lumen size, etc.4.8.2. Importance of sterilization
Sterilization aims to eliminate or kills all microorganisms on medical items. Sterilizing
each piece of equipment is critical to keeping each patient as safe and healthy
as possible.The level of disinfection and sterilization is dependent on the intended use of the
object: Critical items (such as surgical instruments (example forceps), which contact
sterile tissue), semi critical items (such as endoscopes, which contact mucous
membranes), and noncritical items (such as stethoscopes, which contact only
intact skin) require sterilization, high-level disinfection, and low-level disinfection,
respectively. Cleaning must always precede disinfection and sterilization.Self-assessment 4.8.
1) Remove and killing all microorganisms on materials is known as:
a) Disinfection
b) Cleaning
c) Sterilization
d) Destruction
2) What is the importance of disinfection and sterilization4.9. Cleaning and disinfection of environmental surfaces
Learning activity 4.9.
See the picture below and answer the following questions:
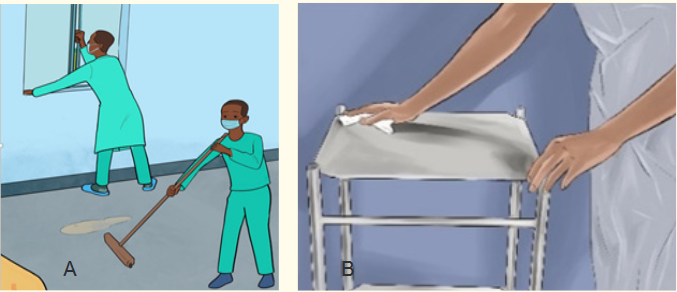
What are you seeing on picture A and B
1) What is importance of activity done on picture A and B?
2) What are the similarities and differences among the picture A and B?Environmental surfaces in health-care settings include furniture and other fixed
items inside and outside of patient rooms and bathrooms, such as tables, chairs,
walls, light switches and computer peripherals, electronic equipment, sinks, toilets
as well as the surfaces of non-critical medical equipment, such as blood pressure
cuffs, stethoscopes, wheelchairs and incubators.4.9.1. Cleaning and disinfection of environmental surfaces
Environmental surfaces are more likely to be contaminated in health-care settings
where certain medical procedures are performed. Therefore, these surfaces, are
being cared for, must be properly cleaned and disinfected to prevent infection
transmission.4.9.2. Principles used in cleaning and disinfection
Cleaning helps to remove pathogens or significantly reduce their load on
contaminated surfaces and is an essential first step in any disinfection process.
Cleaning with water, soap (or a neutral detergent) and some form of mechanical
action (brushing or scrubbing) removes and reduces dirt, debris and other organic
matter such as blood, secretions and excretions, but does not kill microorganisms.Organic matter such as stool, vomits etc. can inhibit direct contact of a disinfectant
to a surface and inactivate the germicidal properties or mode of action of several
disinfectants that is why the cleaning should be done first. Moreover, the disinfectant
concentration and contact time are also critical for effective surface disinfection.
Therefore, a chemical disinfectant, such as chlorine or alcohol, should be appliedafter cleaning to kill any remaining microorganisms.
Disinfectant solutions must be prepared and used according to the manufacturer’s
recommendations for volume and contact time. Concentrations with inadequate
dilution during preparation (too high or too low) may reduce their effectiveness.
High concentrations increase chemical exposure to users and may also damage
surfaces. Enough disinfectant solution should be applied to allow surfaces to
remain wet and untouched long enough for the disinfectant to inactivate pathogens,
as recommended by the manufacturer.Self-assessment 4.9.
1) Why cleaning and disinfection of environmental surfaces?
2) Give four examples of environmental surfaces in health-care settings4.10. Safe handling of linens
Learning activity 4.10.
Observe the pictures below and answer the following questions
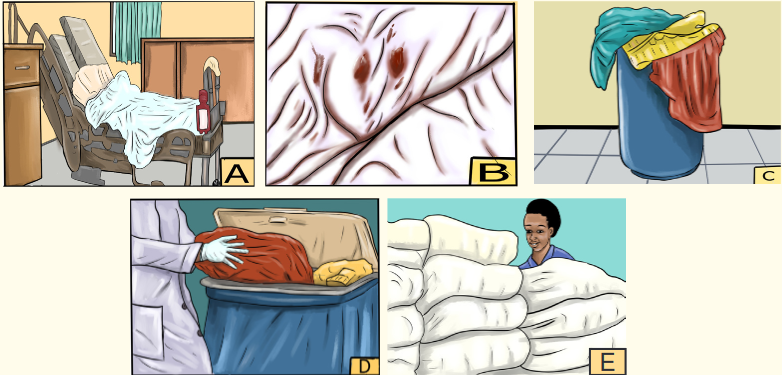
1) What are you seeing on the picture A, B, C, D and E?
2) What is the similarities and differences and on picture C and D?Linen is a kind of cloth that is made from a plant called flax. It is used for making
clothes and things such as tablecloths and sheets4.10.1. Handling linens in health settings
Clean linens should be stored in a clean, designated area, preferably an enclosed
cupboard. If clean linen is not stored in a cupboard then the trolley used for storage
must be designated for this purpose and completely covered with an impervious
covering that is able to withstand decontamination.All soiled linen should be placed into a clearly labeled, leak-proof container (e.g.,
bag, bucket) in the patient care area. Never transport soiled linen by hand outside
the specific patient care area from where it was removed. Never carry soiled linen
against the body; carefully roll up soiled linen to prevent contamination of the air,
surfaces, and cleaning staff and do not shake linen.All used linen should be handled with care to avoid dispersal of microorganisms into
the environment and to avoid contact with staff clothing.General principals of handling the linen consist of hand hygiene protocol respected by
all personnel when handling linen; standard precautions followed when handling
soiled linen, clean linen and soiled linen should be handled, stored, and transported
separately . Furthermore, linen should be maintained in good repair.Self-assessment 4.10.
1) How the soiled linen should be handled in health setting?
4.11. Hazardous wastes management
Learning activity 4.11.
Observe the picture below and answer following questions
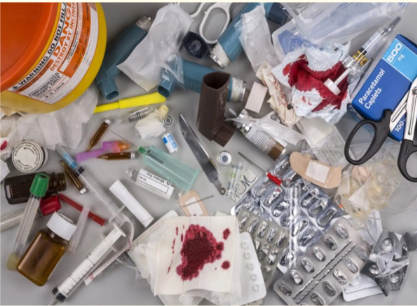
1) What do you see on this picture?
2) What are risks associated with the above hazardous wastes ?A hazardous waste is a waste with properties that make it dangerous or capable
of having a harmful effect on human health or the environment. Hazardous waste
when improperly handled can cause substantial harm to human health.4.11.1. Types of hazards waste
The hazardous nature of health-care waste is due to one or more of the following
characteristics:
Presence of infectious agents
A genotoxic or cytotoxic chemical composition
Presence of toxic or hazardous chemicals or biologically aggressive
pharmaceuticals
Presence of radioactivity
Presence of used sharpsHazardous-waste management consists of the collection, transport, disposal and
treatment of waste material safety. They may cause damage during inadequate
storage, transportation, treatment, or disposal operations.a) Collection of hazardous wastes:
Hazardous waste must be accumulated and stored at the point of generation until removed
by and must be: Collected in a container that is compatible with its contents under all
conditions that it might be subjected to during accumulation, storage, and shipment.
b) Disposing of Biohazardous Wastes
After cleaning up a spill, the nurse is responsible for properly disposing of the
materials. In addition to spilled body fluids, other biohazardous wastes include
soiled dressings, used blood tubes, syringes, catheters, or IVs. Many bio hazardous
items are placed in red “biohazard” bags for disposal. (It is important not to place
inappropriate materials in these bags, because there is an additional charge for
their disposal.) Remember to put sharps, such as needles, lancets, razor blades
or disposable razors, suture removal scissors, or scalpel blades, in the designated
sharps container. Any broken glass must be carefully disposed of as well. Be sure
to ask if you have any questions regarding disposals. The nurse in a community-
based setting or in home care is responsible for disposal of biohazardous wastes
and for teaching clients and families how to dispose of them as well.c) Hazardous waste transport
Hazardous waste generated at a particular site often requires transport to an
approved treatment, storage, or disposal facility. Because of potential threats
to public safety and the environment, transport is given special attention by
governmental agencies. It is highly prohibited to intentionally spilled or abandoned
at random hazardous waste in any locations no designed for that.d) Treatment of hazardous wastes:
Hazardous waste can be treated by chemical, thermal, biological, and physical
methods.Chemical methods include ion exchange, precipitation, oxidation and reduction,
and neutralization.Thermal methods are high-temperature incineration, which not only can detoxify
certain organic wastes but also can destroy them. Special types of thermal
equipment are used for burning waste in either solid, liquid, or sludge form. Theseinclude the fluidized-bed incinerator, multiple-hearth furnace, rotary kiln, and liquid-
injection incinerator. One problem posed by hazardous-waste incineration is the
potential for air pollution.Biological treatment of certain organic wastes, such as those from the petroleum
industry, is also an option. One method used to treat hazardous waste biologically
is called land farming. In this technique the waste is carefully mixed with surface soil
on a suitable tract of land. Microbes that can metabolize the waste may be added,
along with nutrients. In some cases a genetically engineered species of bacteria
is used. Food or forage crops are not grown on the same site. Microbes can also
be used for stabilizing hazardous wastes on previously contaminated sites; in that
case the process is called bioremediation.The chemical, thermal, and biological treatment methods outlined above change
the molecular form of the waste material.Physical treatment, on the other hand, concentrates, solidifies, or reduces the
volume of the waste. Physical processes include evaporation, sedimentation,
flotation, and filtration.So far another process is solidification, which is achieved by encapsulating the
waste in concrete, asphalt, or plastic. Encapsulation produces a solid mass of
material that is resistant to leaching. Waste can also be mixed with lime, fly ash,
and water to form a solid, cementike product.4.11.2. Health risks of hazardous waste
Health-care waste contains potentially harmful microorganisms that can infect
hospital patients, health workers and the general public. Other potential hazards
may include drug-resistant microorganisms which spread from health facilities into
the environment.Adverse health outcomes associated with health care waste and by-products also
include:
Sharps-inflicted injuries;
Toxic exposure to pharmaceutical products,
Chemical burns arising in the context of disinfection, sterilization or waste
treatment activities;
Air pollution arising as a result of the release of particulate matter during
medical waste incineration;
Thermal injuries occurring in conjunction with open burning and the opera-
tion of medical waste incinerators; and
Radiation burns.Self-assessment 4.11.
1) What is the problem associated with hazardous-waste incineration?
2) What is hazardous waste?End unit assessment 4
1) Which of the following is not the effective way to break the
chain of infection?
a) Wearing gloves
b) Hand hygiene
c) Placing patients in isolation
d) providing private rooms for patients2) Which of the following are basic standard precautions for infection
control?
a) Hand hygiene
b) Personal protective equipment and clothing
c) Safe handling of sharps
d) All of these are basic standard precautions3) The nurse wears a gown when:
a) The patient’s hygiene is poor
b) The nurse is assisting with medication administration.
c) The patient has acquired immunodeficiency syndrome (AIDS) or
hepatitis.
d) Blood or body fluids may get on the nurse’s clothing from a task
that he or she plans to perform.4) Respiratory hygiene/cough etiquette includes:
a) Posting visual alerts about signs and symptoms of infection
b) Re-using tissues to help keep costs down
c) Frequent hand hygiene, especially after contact with respiratory
secretions
d) A and C are corrects5) Remove and killing all microorganisms on materials is known as:
a) Disinfection
b) Cleaning
c) Sterilization
d) Destruction6) Which of the following is included in the steps for needle stick injuries?
a) Wash needle stick injury with soap and water
b) Report needle stick injury to your supervisor
c) Wash needle stick injury with soap and water and use alcohol
d) A and B are correct answers7) Match in the correct order of donning(wearing) Personal Protective
Equipment (PPE) :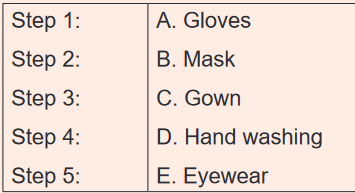
8) Arrange in the correct order of doffing (removing) Personal Protective
Equipment: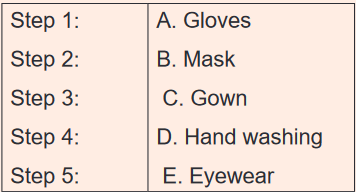
9) Define nosocomial infections
10) Explain the causes of transmission of nosocomial infections
11) Discuss the mode of transmission of nosocomial infections
12) Differentiate asepsis and antisepsis
13) What is importance of standards precautions of nosocomial infection?
14) What are benefits associated with hand washing?
15) What is the importance of respiratory hygiene /cough etiquette?UNIT 5: DRUG ADMINISTRATION
Key Unit Competence:
Administer correctly drugs through enteral, topical and selected parenteral routesIntroductory activity 5.
Case study on drug administration
Shema a 16-year-old boy went for consultation to NKUNGU health center, they
prescribed anti malaria 4 tablets to be taken by mouth two times a day for
three days. On the 2nd day, he forgot the morning tablets, during the evening
he decided to take together the forgotten tablets and current ones. At 10 P.M,
he started developing vomiting, weakness and abdominal pain. His parents
took him immediately back to the health center, the nurse transferred Shema
to MIBIRIZI District hospital for further management. At the admission, the Dr
started medication in form of injections for 3 days, including anti malaria and
anti-vomiting. A nurse calculates the prescribed dose as required then she
gives to Shema, after 2 days, Shema recovered and discharged.1) After being treated at his health facility, SHEMA received different
medications. Did his health care provider give him instructions to follow
about medication before going back home?
2) In this case, discuss the instruction nurse provided to Shema before
going home to continue medication.
3) What do you think about Shema’s attitude in regards his prescribed
tablets? Give your suggestion.
4) What do you think about different ways of taking prescribed medication?
5) Do you think the action of the Dr, to change the tablet to injection
medication for Shema, was is it the right time? Explain5.1. Rights of drug administration
Learning activity 5.1.
Read the text below and answer related questions:
Nurse Brune is going to offer insulin to a patient in room 213, internal medicine
at King Faisal Hospital. She reads careful the patient file to confirm the patient’s
name, age and disease, the amount, name of the drug, expiration date and the
intervals to follow to provide everyday dose. Arriving in the patient room, she
introduces to the patient and explain the indication, purpose and the route of
medication administration. The patient agrees to receive the drug, the nurse
started by controlling blood sugar and then injected the prescribed amount of
insulin. After providing this medication, she documented the whole process in
patient file.
1) As an associate nurse, do you believe on Brune’s process of drug
administration?
2) What are the rights of drug administration observed in the above case
study?
3) Do you think that there are other drug administration right not mentioned
in this case study? If yes list them.When people become ill, they are used to go to the health centers to seek for
treatment. Some treatment mode involves prescription of medications with curative
or preventive role. To achieve intended outcomes, health professionals should
follow different rights of drug administration in order to ensure patient safety.Drug administration is the process of giving out medication to the patient in order
treat or prevent disease or complication.A medication/drug is a substance administered for the diagnosis, treatment, relief
of a symptom and prevention of disease. Nurses help the patients to develop a
proactive understanding of medications, clarifying the confusing information and
responsibly share decision making with other healthcare professionals.Right for drug administration is a guidance to health practitioners on the
appropriate way to follow while ensuring the safety of drug administration.
This is a nursing responsibility. To abide to the rights of drugs administration
help nurses to maintain patient safety, meet the quality of care and prevent
medication errors.In today’s health care delivery, nurses are accountable for their practices.
This is the reason why; we have to be aware from the beginning the rights of
drug administration to ensure both patient and healthcare professionals are
protected.5.1.1. Right patient
The first right in drug administration is to identify the correct patient to be given
medications. A nurse must carefully verify the person’s identification each time
before administration of a medication. Use the names as recorded in the patient
file, ask the patient if he or she is conscious and read patient identification band.5.1.2. Right medication
The ordered medication is appropriate for the patient. Nurses should not rely on
memory from previous interaction with the patient because beds can be changed
at any way or patent discharged and replaced.5.1.3. Right dose
The dose ordered is appropriate for the patient. A nurse should be able to calculate
the correct dose in accordance to the prescription and not expect to always exact
doses of medication from pharmacy. E.g: a dose may be a half of a tablet, two
tablets, the tenth of a bottle depending on the desired doses.5.1.4. Right time
Give the medication at the right frequency and at the time as ordered. Medications
given within 30 minutes before or after the scheduled time are considered to meet
the right time standard.5.1.5. Right route
Give the medication by the ordered way of administration. Make sure that the route
is safe and appropriate for the person.5.1.6. Right education
Explain information about the medication to the person e.g. why receiving, what to
expect, any precautions.5.1.7. Right documentation
Document medication administration after giving it, not before. Write the name and
the dose of given medication, route of administration and injection site in case of
parenteral medication, date and time lastly the name or initials of the administeringnurse. Please, note any issue encountered during this process such as lack of the
medication, vomiting after oral medication intake, any abnormal reaction5.1.8. Right to refuse
Adults have the right to refuse any medication. The nurse’s role is to ensure that the
person is fully informed of the potential consequences of refusal and to communicate
the person’s refusal to the health care provider.5.1.9. Right assessment
Some medications require specific assessment prior to administration. E.g: Check
blood pressure before giving diuretics, verify glycemia values before giving insuline.
Medication orders and manufacturer instructions may indicate specific parameters.
E.g: do not give if pulse is less than 60 beats per minute or do not give if systolic
blood pressure less than 100 mmHg”.5.1.10. Right evaluation
The nurse has to make a proper follow-up after certain time of drug administration.
That follow up will answer questions such as: Was the desired effect achieved?
Did the person experience any side effects or adverse reactions? If, yes what was
those side effects or adverse reactions?Self-assessment 5.1.
1) What do you understand by drug administration?
2) Explain different rights of drug administration.
3) An associate nurse student is asked to administer Cloxacillin 350mg
per mouth but the prescription was not very clear to read. He decided to
offer 500mg because it was difficult to read the prescription. Which right
of drug administration has been not respected in this case?5.2. Enteral routes of drug administration
Learning activity 5.2.
Nurses use various ways of drug administration as illustrated in the pictures
below.
Observe these pictures.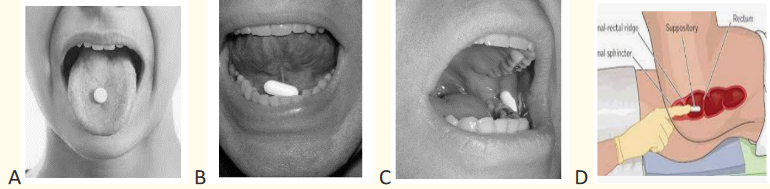
1) Observe the above picture A, B, C, D, do you think all tablets are
reserved to be swallowed?
2) What are the similarities and difference between the message from the
above pictures?
3) Give the indications of drug administration routes presented above
4) What are the advantages of the above routes of drug administration?When people become ill, they are used to go to the health centers or hospital for
treatment. Some treatment modalities involve medication provision. Usually, every
medication has a way to be administered in order to reach the site of action. The route
of drug administration is the path by which a drug, fluid or other substance is brought into
contact with the body to obtain maximum benefit. The route of administration should
be indicated when the drug is ordered. When administering a drug, the nurse should
ensure that the pharmaceutical preparation is appropriate for the route specified. The
enteral route of drug administration is the one of three categories.Enteral administration is about exposing drug to the gastrointestinal (GI) tract.
The medications are introduced in the mouth or in the rectum. The enteral route of
drug administration includes oral, buccal, sublingual and rectal route.Substances prepared for enteral administration may be available in a variety of
pills, including tablets, capsules, and syrup. Tablets are commonly round, and are
sometimes coated so that they do not easily dissolve in the mouth. Capsules have
rectangle forms and may contain granules of the active compound that release as
the outer coating is dissolved in the stomach. Children may have immature muscle
and nerve development which interfere with swallowing reflexes others may just
dislike their taste.5.2.1. Oral route
Oral route (Figure 68) is the most common, least expensive and most convenient
route for most people.In oral administration, the medication is given by mouth and then swallowed. It is
used for patients who can ingest and tolerate an oral form of medication however it
cannot be used in unconscious patients, patients with vomiting, in patient with nil
per mouth order and during emergency.Oral route of drug administration is most convenient, usually least expensive,
safe, does not break skin barrier and administration usually does not cause stress.
This route has some disadvantages as some medication have unpleasant taste,
can cause irritation of the gastric mucosa (Aspirine), poorly absorbed from the
gastrointestinal tract and may harm to the person’s teeth. For example, the liquid
preparation of ferrous sulfate (iron) can stain the teeth.For oral drug administration technic, nurse need different equipment like
prescription chart, medication pack, disposable medicines container; straw, water
or juice, kidney dish to be used in case of vomiting, examination gloves and plate.
This equipment will be needed in the below procedure:Procedural steps
1. Preparation
Review the patient’s notes and prescription.
Wash hands
Gather all necessary equipment and arrange them on the plate
Check that the details on the prescription are complete, including the pa-
tient’s name, hospital number, date of birth and allergy status
Self-introduction by name and function to the patient and obtain verbal
consent. This is an ideal opportunity to answer any questions the patient
has about their treatment and check their understanding of the medicine
regimen.
Check that the prescription is unambiguous/legible and includes the medi-
cine name, form, route of administration, strength and dose of the medicine
to be administered.
Check the date and time when it should be administered, that the prescrip-
tion is signed and includes a start and finish date, if appropriate
Caution: A medicine should not be administered if there are any concerns
about the prescription; any such concerns should be discussed immediately
with the prescriber. Ensure you know why the medicine is being administered and you are
aware of potential complications associated with administration
Check if the medicine has not been given to the patient and signed for by
another staff member.
Take the medicine and prescription to the patient and check the identity of
the patient against the prescription using their name, hospital number and
date of birth. Check their wristband according to local policy. It is important
to ask the patient to state, rather than confirm, their name and date of birth.
Complete the necessary assessment before administering the medication.
Check whether the patient has any allergies or previous adverse drug reac-
tions.1. Implementation
Wash your hands.
Position the patient comfortably so they can swallow the medicine, (The
patient should be placed in a sitting position to prevent accidental aspiration
of the medication).
Decontaminate your hands.
Select the medicine and check the expiry date
Put the required dose into a medicine pot, avoiding touching the medicine.
Position the patient in sitting or upright position
Administer the medicine (put the tab or capsule on the tongue).
Offer a drink of water or other permitted fluid with pills, capsules, tablets
to help the patient swallow the medicine if this is allowed, and ensure they
have swallowed it.
When administering a liquid suspension, shaken the bottle before the appro-
priate dose is poured. When administering sprays, the container also needs
to be shaken2. Finishing
Thank the patient, arrange patient items, and provide appropriate health
education
Disposal of the medicine pot according to local policy.
Decontaminate your hands.
Immediately record that the medicine has been administered
If the patient refuses or is unable to take their medicine, this should be docu-
mented along with the reason for omission and inform the prescriber.
Check the client within 30min to verify response to medication
Caution: If the capsule or tablet fall down, it must be discarded and a new one
should be administered. Oral medications need to be given before sublingual or
buccal medications.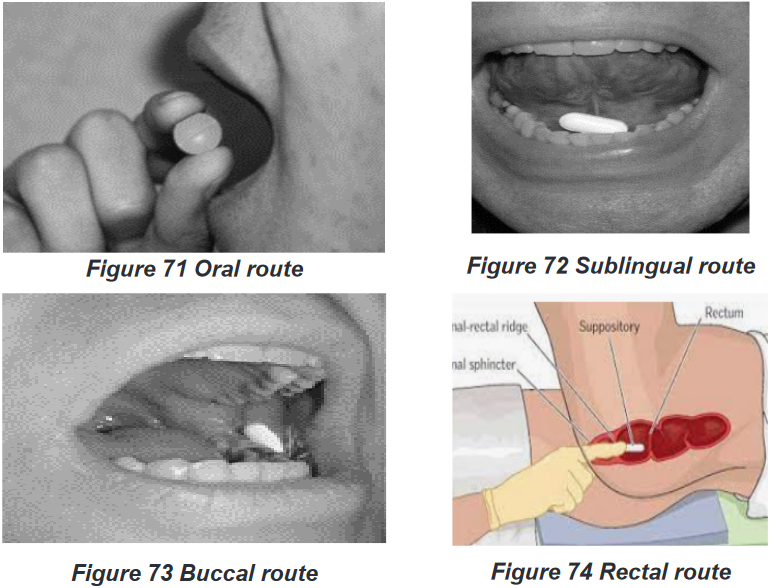
5.2.2. Sublingual route
Sublingual (Figure 72 Sublingual route) is another enteral route of drug
administration where a drug is placed under the tongue and then it dissolves there
in short time, the drug is largely absorbed into the blood vessels on the underside
of the tongue. E.g.: Nitroglycerine.Sublingual route is indicated in any of the following circumstances such as
When the drug needs to get into body system quickly, When patient has trouble
of swallowing medication, When the medication doesn’t absorb very well in the
stomach and When the effects of the drug would be decreased by digestionSublingual route is contraindicated for patients who cannot tolerate oral drugs,
such as those who have altered mental status or have nausea or vomiting.The sublingual route’s advantages are that it is more potent than oral route
because drug directly enters the blood and bypasses the liver, drug is rapidly
absorbed into the bloodstream, no need to swallow the drug, easier to take for
people who have problems of swallowing pills.However, this route has some disadvantages such as inactivation of drug by gastric
juice if swallowed, drug must remain under tongue until dissolved and absorbed,may cause irritation of the mucous membranes, not used in large amount of
medication, inconvenient to maintain the exact site. It induces nausea and vomiting
if it has unpleasant taste. Eating, drinking, or smoking, can affect how the drug is
absorbed and how well it works. Any open sores in the mouth can also become
irritated by the medication.In addition to the oral route technique basis, sublingual administration requires the
patient to open his or her mouth and raise the tongue. The tablet should then be
placed under the tongue. The nurse should examine the mucous membranes of the
patient’s mouth for irritation or sores. If there are sores in the mouth, the physician
should be contacted before any sublingual drugs administration. Alternating sites
should be used when giving regular doses of sublingual or buccal medications.
Explained to the patient that nothing should be eaten, drank, swallowed, chewed,
or smoked until the tablet has dissolved.5.2.3. Buccal route
Buccal route (Figure 73 Buccal route) of drug administration is another form of
enteral route which means that the drug is placed between cheek and gum.In buccal administration, a medication (e.g. a tablet) is held in the mouth against the
mucous membranes of the cheek until the drug dissolves. The drug may act locally
on the mucous membranes of the mouth or systemically.In buccal route drug directly enters the blood and bypasses the liver, drug is rapidly
absorbed into the bloodstream. It is contraindicated for patients who cannot tolerate
oral drugs, such as those who have altered mental status or have nausea or vomiting.Buccal route of drug administration has disadvantages like inactivation of drug
if swallowed, drug must remain between cheeks and gum until dissolved and
absorbed. Drug in buccal administration may cause stinging or irritation of the mucous
membranes. This is not used in large amount of medication, inconvenient to maintain
the exact site. It induces nausea and vomiting if drug has unpleasant taste.In addition to the oral route technic, in buccal drug administration the patient should
open his or her mouth, then tablet should be placed between the gum and the wall
of the cheek. With the mouth closed, the tablet should be held in this position for
five to 10 minutes until it has dissolve. Mouth should be examined for the presence
of sore before drug administration through this route. Alternating sites should be
used when giving regular doses of buccal medications.5.2.4. Rectal route
Rectal route is also anther enteral form of drug administration which consist of
administration of medication into rectum for absorption.It can be used as a drug delivery route for both local and systemic effects. Rectal
medication may be in suppository or in liquid form in order to facilitate administration
and absorption.It is indicated when drug has unpleasant taste or odor, drug released at slow,
steady rate provides a local therapeutic effect. To evacuate the bowel before
surgical intervention, help to relieve constipation as well as when they want to treat
hemorrhoids or anal pruritis. The most common medication in rectal routes serve as
antipyretic, analgesia and laxatives as long as the patient accept the rectal route.This route is contraindicated when patient refuse to consent, recent rectal or anal
surgery, abnormalities or trauma involving the perineal area, suspected paralytic
ileus or colonic obstruction, diarrhea and in case of active anal bleeding.The rectal route has advantages such as the absorption rate of the drug not influenced
by food or gastric emptying. The metabolism of both enteric and first-pass hepatic
elimination is avoided. It is a preferred route when drugs are administered to relieve
constipation or hemorrhoids. Drugs administered in rectal have a faster action
than via the oral route and has a higher bio-availability. Rectal administration also
reduces side-effects of some drugs, such as gastric irritation, nausea and vomiting.
Applicable in cases of nausea, vomiting, and inability to swallow (unconscious
patients), as well as in the presence of diseases of the upper gastrointestinal tract
that affect oral drug absorption. It is a tolerable route in children. In cases of toxicity
or overdose, this effect can be rapidly terminated.The disadvantages of rectal route include the interruption of the absorption process
by defecation which leads to irregular or incomplete absorption. Low volume of
rectal fluids can lead to incomplete dissolution of the drug. Certain drugs may be
altered by microorganisms in the rectum and patient adherence may be a problem.Rectal application technique
Rectal suppositories are used mainly to local effects as laxatives and stool softener
and systemic effect such as reducing nausea, vomiting and fever. The rectal
suppositories are thinner and bullet shaped than vaginal ones. They are kept in
refrigerator until their administration, remember to always wear gloves before
insertion of rectal medication to protect your hands from fecal contamination.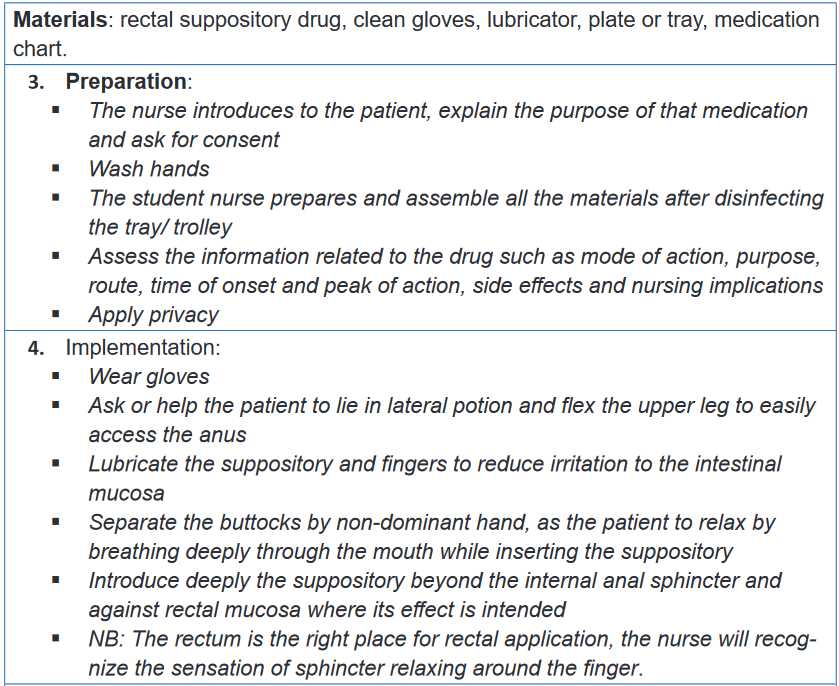
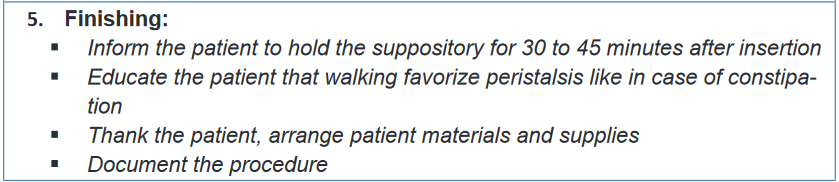
Self-assessment 5.2.
1) Illustrates the disadvantages of buccal route of drug administration?
2) What happen when a drug designated to sublingual administration is
accidentally swallowed?
3) What are the precautional measures a nurse will teach a patient who is
taking medication in sublingual?
a) Precise the location of a drug in buccal route of medication
administration
4) Where do we exactly dispose a suppository drug using rectal route5) Administration way which is least expensive, using little equipment,
and minimal training is the
a) Oral route
b) Skin application
c) Vaginal application
d) Intradermal route
6) Why will you choose to administer medication in oral route?
7) List the disadvantages of oral route of drug administration
8) Patient KANEZA is hospitalized for 3 days under treatments including
suppository, while an associate nurse going to administer the medication
found the patient has a diarrhoea. What can you do to help this patient
taking his medication as an associate nurse? Tell us the best route to
be used to treat this patient among the routes we already covered?5.3. Parenteral route- Intramuscular (IM)
Learning Activity 5.3.
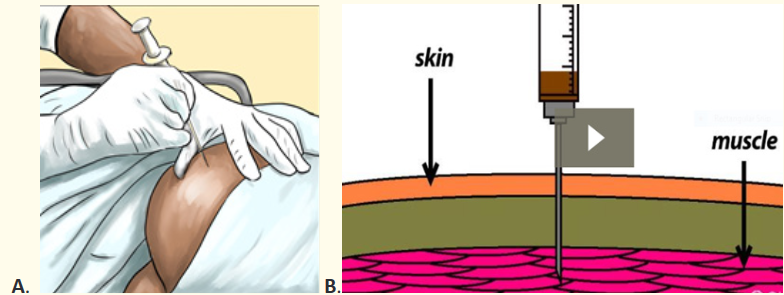
Observe the images above (A and B) and answer the following questions:
1) Talk about what a person with gloved hands is doing?
2) What is the relationship and differences between image A and B?
3) Which materials are being used on image ADepending the form of medication or patient’s conditions, different routes of drug
administration can be applied including parenteral route. Parenteral route of
drug administration is a way to administer medication in form of solution into the
body using injection to attain rapid systemic effect. It can also be injected in a
localized organ or tissue in order to achieve high concentration in the site of action
or minimize systemic effect. When selecting an injection site, avoid the area with
skin abnormalities (e.g: scar tissue, birth marks, tumor) or at bony prominences.
The intramuscular route is one of parenteral routes which is a method of installing
medications via injection into the depth of the bulk of specifically selected muscles.
The common sites for IM injection are ventrogluteal, dorsogluteal, vastus lateralis
and deltoid muscle. The basis of this process is that the large muscles have good
vascularity, and therefore the injected drug quickly reaches the systemic circulation
and thereafter into the specific region of action, bypassing the first-pass metabolism.Always remember to select safe site away from large nerves, bones and blood
vessels. Failure to do so may be the origin of different complications such as
abscess, necrosis, nerve injuries, lingering pain and periostitis. The amount of 4 ml
is considered the maximum dose in a single site for adults in the developed muscle.
IM is commonly indicated for patients who are noncompliant, uncooperative,
reluctant, and unable to receive drugs through other commonly utilized routes.It is contraindicated to use IM in case of active infection such as cellulitis or
dermatitis at the site of administration. Acute myocardial infarction- the release
of muscle enzymes may provide a confounding bias in making the diagnosis. In
case of thrombocytopenia, coagulation defects, hypovolemic shock which cause
reduced absorption of the drug due to poor perfusion of that muscle. Myopathies
and associated muscular atrophy delay drug absorption as well as adds up the risk
of neurovascular injuries.The advantages of IM route are based on its rapid and uniform absorption of the
drug, especially those of the aqueous solutions. It has a rapid onset of the action
compared to that of the oral and the subcutaneous routes. IM injection avoids the
first-pass metabolism as well as gastric factors governing the drug absorption. Has
efficacy and potency comparable to that of the intravenous drug delivery system,
highly effective in emergency scenarios such as acute psychosis and status
epilepticus. A large volume of the drug can be administered compared to that of the
subcutaneous route.The disadvantages of IM route is that the administration of medications require
a trained personnel. The absorption of the drug is determined by the bulk of the
muscle and its vascularity. It is not a best option during emergency. IM injection
at the appropriate landmarks may be difficult in a child as well as in patients
requiring physical restrain. Inadvertent injection in the subcutaneous plane of the
fascia can lead to delayed action of the drug. It is painful, can lead to anxiety inthe patient, especially in children. Self-administration of the drug can be difficult.
The precipitation of the drug following faster absorption of the solvent may lead to
delayed and prolonged action of the drug. Unintended prolonged sequelae following
delayed drug release from the muscular compartment.Common complications IM injection can be summarized as muscle fibrosis and
contracture, abscess at the injection site, gangrene, nerve injury -the sciatic nerve in
gluteal injection, the femoral nerve in vastus lateralis injection, the superior gluteal
nerve in dorso gluteal injection and radial nerve in deltoid injection, periostitis,
transmission of HIV, hepatitis virus when sharing the needle and persistent pain at
the site of injection.5.3.1. Anatomical landmarks in IM injection
There are specific landmarks to be taken into consideration while giving IM injections
so as to avoid any neurovascular injuries. The specific landmarks for the most
commonly used sites are discussed below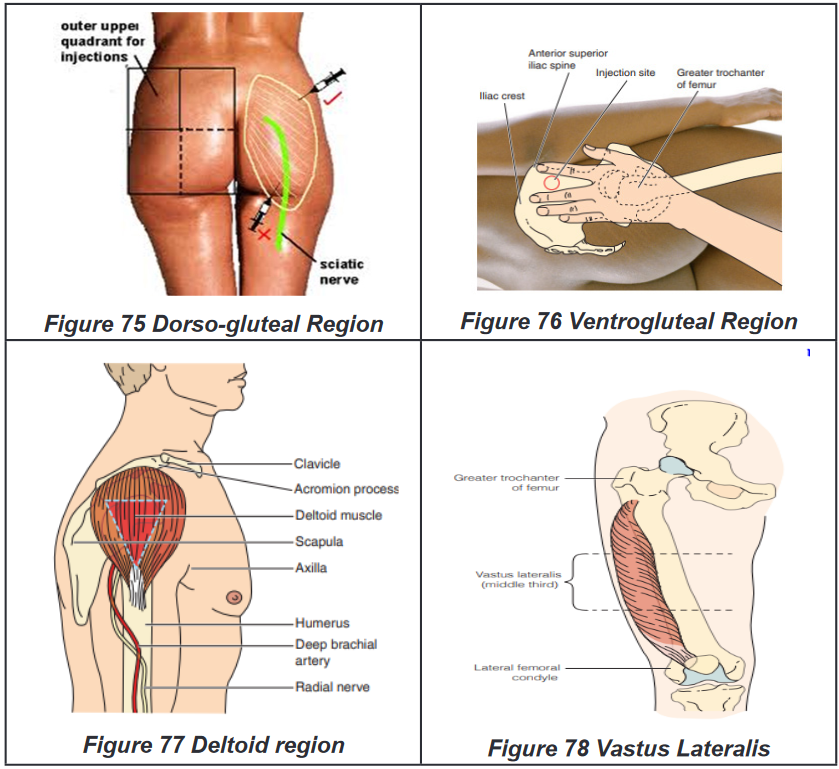
BOX 5.3.1.
• The dorso-gluteal site is upper outer quadrant of each buttock
• The deltoid site is 2.5 to 5 cm below the acromion process
• During the ventrogluteal site location, the heel of the opposing hand is
placed in the greater trochanter, the index finger in the anterior superior
iliac spine, and the middle finger below the iliac crest. The drug is injected
into the triangle formed by the index, middle finger, and the iliac crest
• The vastus lateralis site is the middle third of the line joining the greater
trochanter of the femur and the lateral femoral condyle of the knee.5.3.2. Intramuscular (IM) injection technique
Materials: sterile syringes and needles, alcohol-based antiseptic solution, drug,
medication chart, dry cotton swab, safety box, disposable gloves, dustbin, trolley,
plate.1. Preparation:
Introduce yourself to the patient including your name and role
Confirm the patient’s name and date of birth
Briefly explain the procedure, indication of the drug using patient-friendly
language
Gain consent to proceed with intramuscular injection
Check for any contraindications to performing an intramuscular injection
Check if the patient has any allergies
Ask if the patient has a preferred injection site. If the patient is receiving regular
intramuscular injections, ensure that the injection sites are rotated
Position the patient so that they are sitting or lying comfortably according to
selected site
Wash your hands
Gather equipment
Do final checks/ rights of drug administration:
Right patient: ask the patient to confirm their details and then compare this to
the patient’s wrist band (if present) and the prescription
Right drug: check the labelled drug against the prescription and ensure the
medication hasn’t expired
Right dose: check the drug dose against the prescription to ensure it is correct
Right time: confirm the appropriate time to be administering the medication and
check when the patient had previous doses if relevant
Right route: check that the planned route is appropriate for the medication you
are administering
Right to refuse: ensure that valid consent has been gained prior to medication
administration
Right assessment: ensure all the precautions are examined before administer
any medication2. Implementation:
Wash and dry your hands or use hand rub
Wear gloves and an apron
Draw-up the appropriate medication into the syringe using a drawing-up needle
Remove the air bubbles from the syringe
Remove the drawing-up needle and immediately dispose of it into a sharps bin,
then attach the needle to be used for performing the injection
Choose an appropriate site for the injection
Position the patient to provide optimal access to your chosen site
Clean the site
Gently place traction on the skin with your non-dominant hand away from the in-
jection site, continuing the traction until the needle has been removed from the
skin. If the patient is elderly with reduced muscle mass or the patient is emaciat-
ed, do not apply traction, instead, bunch the muscle up to ensure adequate bulk
before injecting.
Warn the patient of a sharp scratch
Holding the syringe like a projectile in your dominant hand, pierce the skin at a
90° angle.
Insert the needle quickly and firmly, leaving approximately one-third of the shaft
exposed (however this varies between sites and patients).
Aspirate to check if the needle is not in a blood vessel
If aspiration does not reveal blood (evidence of intravascular needle placement)
inject the contents of the syringe whilst holding the barrel firmly.
If the aspiration reveal blood into syringe (this is a sign of intravascular injec-
tion), do not inject medication, remove syringe and needle immediately, discard
it with contained medication and start over with anew medication.
Inject the medication slowly at a rate of approximately 1ml every 10 seconds.
Remove the needle and immediately dispose of it into a safety box
Release the traction you were applying to the skin
Apply gentle pressure over the injection site with a cotton swab or gauze. Do
not rub the site.
Discard the gauze3. Finishing:
Offer a comfortable position and arrange patient’s environment
Explain to the patient that the procedure is now complete
Thank the patient for their time
Remove of your gloves and equipment into an appropriate clinical dustbin
Arrange used materials
Wash your hands
Document the details of the procedure and the medication administered
Evaluate the client response to the medication within time flame.Self-assessment 5.3.
1) What are the advantages and disadvantages of intramuscular injection?
2) List the commonly used sites for intramuscular injection
3) List the commonly used sites for intramuscular injection
4) KALISA a 39-year-old man is admitted in surgical ward following road
traffic accident. He is still complaining about pain even though he received
diclofenac 100mg suppository every 12 hours 1gr Paracetamol tablets
every 8 hours. As an associate nurse, which route would you propose
to bring a quick control on patient’s pain? Explain why of the proposed
route.5.4. Parenteral route-Subcutaneous (SC)
Learning activity 5.4.
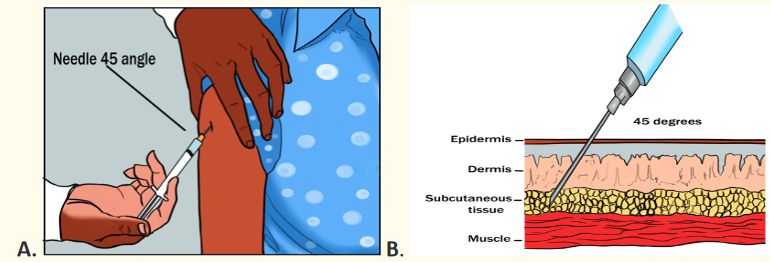
Observe the image above (A and B) and answer the following questions:
1) Describe the action which is being done on the image A
2) What is the meaning of 450C degrees on both image A and B
3) What are the advantages and disadvantages of the action on the image ASubcutaneous route of drug administration is another parenteral way of drug
administration. It consists of deposits the medication into the subcutaneous layer
below the skin and above the muscle layer. The drug to be used must be isotonic
and must be the same pH as the tissue in order to prevent irritation and tissue
damage. There are different sites of subcutaneous injection as illustrated on the
picture below: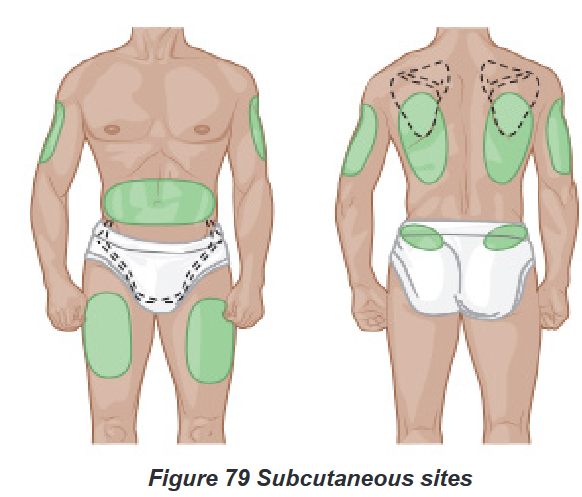
The sites for subcutaneous injection are the following: The back of the upper arms,
the abdomen (but stay a minimum of 5cm away from the umbilicus), the anterior
thighs, the area of the back just below the scapulae and the upper buttocks.SC is indicated when slow and continuous absorption is required and long duration
of action. E.g. Insulin, heparin. It is contraindicated in case of edema or inflammation
at the planned site of injection, shock and peripheral hypoperfusion (because it can
impair absorption), and when patients refusing consent to the procedure. It serves
to provide complete drug absorption. It is less invasive than intramuscular as it
ends up in the subcutaneous tissues. It is also possible to train the patient for self-
administration especially if he or she is taking lifelong medication. E.g: insulin.SC route has some disadvantages as it is expensive than oral route as it involves
some degree of education and materials. On the other hand, it is slower than
intramuscular injection. The procedure of SC injection breaks the skin barrier, causes
pain, can irritate tissues and may be a source of anxiety. SC drug administration
is applicable for limited quantities of medications not exceeding 1.5 to 2 ml, the
greater amount will cause pain.
Procedural stepsMaterials
To perform SC injection, there is a need of different equipment such as needles
and syringe, drug for administration, medicines administration prescription, tray to
carry the drug, sharps container, alcohol swab or cotton and disinfectant1. Preparation:
Introduce yourself to the patient including your name and role
Confirm the patient’s name and date of birth
Briefly explain the procedure, indication of the drug using patient-friendly
language
Gain consent to proceed with intramuscular injection
Check for any contraindications to performing an intramuscular injection
Apply folded screen around the bed patient to ensure privacy during the
procedure.
Check whether the patient has any allergies.
Check if the prescription is correct and follow the rights of medicines admin-
istration
Wash and dry hands to reduce the risk of infection.
Assemble the syringe and needle and then draw the required amount of
drug from the ampoule. Some drugs are available in pre-filled syringes and
manufacturer’s instructions should be followed, example enoxaparin.
Remove any air bubbles from the syringe.
Change the needle to ensure that the one you are about to use for injecting
the drug is sharp, thereby reducing pain.
Dispose of the needle used to draw the drug in a sharps container according
to local policy and apply a new one.
Place the injection in a tray and take it to the patient, along with a sharps bin
so the used needle can be disposed of immediately after the procedure.
Position the patient comfortably with the selected injection site exposed.
Check the site for signs of oedema, infection or skin lesions. If any of these
are present, select a different site.
Wash and dry hands or rub the hands
Put gloves on4. Implementation:
Disinfect the skin with alcohol swab.
Inform the patient that you are going to carry out the injection. Use distrac-
tion and relaxation techniques to reduce anxiety if needed.
Hold the syringe and needle in your dominant hand and pinch the skin
together using the non-dominant hand to lift the tissue away from underlying
muscle
Insert the needle at the required angle 450 degree or 900 degrees for the
obese patients to ensure that you inject medication in subcutaneous tissue.
Aspiration to check whether the needle is not in a blood vessel, if so, re-
move the needle and discard both the needle and syringe then prepare a
new medication.
If no blood appears, inject the drug slowly over 10-30 seconds
Massage the area gently with a swab but don’t massage after insulin and
heparin SC injections (massage heparin injection after SC foster bruising
whereas it speeds up the absorption of insulin)
Release the lifted skinfold5. Finishing:
Dispose of sharps directly into the sharps bin and dispose of the syringe
according to local policy.
Ensure the patient is comfortable and wash hands.
Record administration on the prescription chart. Also record administration
site so that the same site is not repeatedly used. This is to avoid lipohyper-
trophy.
Monitor the patient for any effects of the prescribed medicine and any prob-
lems with the injection site.
Patients receiving injection in a health center or outpatient department may
need to wait for a period of time to monitor for any reaction to the drug. Lo-
cal policies should be followed.Self-assessment 5.4.
1) Dr. MUTESI writes a prescription for 5mg of morphine in SC every 12
hours. The medication is available in a concentration of 10 mg per 2ml
a) Describe the commonly used sites for subcutaneous injections?
b) What is the rational to inject at 45 degrees in subcutaneous
injection?
2) MUKASINE a 78-year-old woman needs a SC injection of anti-tetanic
vaccine. You realize that she is having generalized edema. What will do
in this situation?5.5. Parenteral route- Intradermal (ID)
Learning activity 5.5.
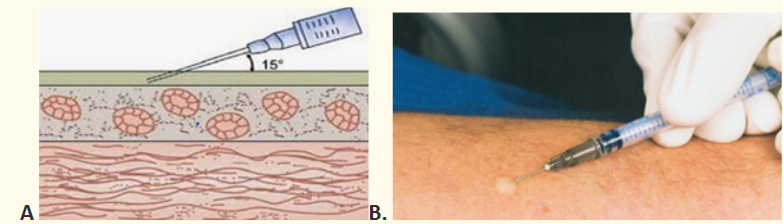
Look carefully the image posted here and respond related questions.
1) What do you see on the site of injection in picture B?
2) What is the relationship between image A and B.
3) Why is the angle of 150 appliedAnother parenteral route of drug administration is the intradermal (ID) route. ID is
the administration of a drug into the dermal layer of the skin just under the epidermis.
ID is indicated frequently for allergy testing before administering larger amounts
of drug by other routes or in case of tuberculosis vaccination and screening. The
advantage of these tests is that the body reaction is easy to visualize, and the
degree of reaction can be assessed. Before using this route choose an injection
site that is free from lesions, rashes, moles, or scars, which may alter the visual
inspection of the test results. Once the ID injection is completed, a bleb (small
blister) should appear under the skin. Its disadvantages are based on the longest
absorption time of all parenteral routes. The procedure is usually painful, so make
sure that the needle is inserted into the epidermis at an angle of 10 to 15 degrees
and not into enter the subcutaneous to reduce patient discomfort. To make the
intradermal injection, we need materials such as sterile syringes and needles
specific for ID, alcohol-based antiseptic solution, drug, medication chart, dry cotton
swab, safety box, disposable gloves, dustbin, trolley, plate.Intradermal procedure
Gather all the equipment needed and check the physician order
Explain the procedure to the patient, the purpose, site for injection, and how he/
she has to cooperate.
Wash hands and wear disposable gloves
Prepare medication from ampule or vial.
Position the patient and select the inner aspect of the forearm, upper chest, or
upper back beneath scapulae that is not very hyperpigmented or covered with
hair.
Cleanse the site with an alcohol swab in a circular motion moving outward.
Allow skin to dry. Keep cotton in the clean tray for reuse when taking out the
needle.
Remove the needle cap with the non-dominant hand by pulling it straight off.
Use the non -dominant hand to spread skin taut over the injection site.
Place the needle almost flat against the patient’s skin. Insert 0.4cm bevel up so
that needle can be seen through the skin.
Slowly inject the drug (0.01ml-0.1ml do not exceed 0.5ml) watching for a bleb
to develop (appearance of the bleb indicates that the needle is in intradermal
tissue). If not, remove the needle and restart.
Withdraw the needle quickly at the same angle as it was inserted
Do not massage the area.
Do not recap the needle. Discard syringe and needle into the appropriate recep-
tacle
Thank the patient and arrange his or her environment
Offer appropriate health education
Remove glove and wash hands.
Record the medication administration-the medication administered, amount,
dose, site, and patients’ response
Draw a circle using blue/black pen around the injection site. Write the date and
time of administration of medication.
Check the reaction within a specified interval of time; usually, it depends on the
hospital protocols.
Inform the physician of a medication reaction.Self-assessment 5.5.
1) Intradermal injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 900
2) What will indicate you that you successful injected a drug in intradermal
route?
3) Associate nurse M. is going to administer a small dose of penicillin to a
patient to test for hypersensitivity or allergy on that drug. Which route will
M. use? What is the maximum dose not to be exceeded is?5.6. Topical skin application
Learning activity 5.6.

) What this image shows to you
2) When is skin medication indicated?
3) Discuss on the side effect which may originate from skin medication
application?Sometimes the location of a disease may dictate the route of drug administration.
The outermost body parts are treated by using topical route of drug administration.
The topical route of drug administration involves applying a drug to the skin
or mucous membranes for example in the eye, external ear canal, nose andvagina. They are typically used for their action at one specific site. They usually act
locally, but they may have systemic effects. The frequency of delivery of the drug
is controlled and depends up the type of the prescribed drug and instructions from
the manufacturer.Topical dermatological preparations are in different forms such as ointment,
lotions, creams, powders, pastes, sprays and patches. The lotions, ointment and
creams are used to manage skin diseases localized on the specific area of the
skin. Lotion such as skin moisturizers prevent the complication linked to excessive
dry skin. This is the application of the drug to the desired area of the skin which
will serve as route of absorption. The ointment such zinc oxide when applied on
the skin, it protects against abrasion or moisture associated with bowel or bladder
incontinence. Patches as a form of transdermal medication which are designed to
be applied on the skin and then penetrate it to generate systematic effect. Patches
may last between 24 to 72 hours. Nitroglycerine and nicotine are the commonly
used patches. This route has fewer risks to gastro intestinal system, fewer risks
of abuse and easy to administer. In some case the drug can be sufficient enough
to enter systemic circulation and produce unwanted side effects. During the use
of topical medication there is a risk to potential production of irritant and allergic
contact dermatitis, potential rapid appearance of bacterial resistance and potential
alteration of cutaneous flora. Before application of skin preparation, we need to wash
it with water and soap then dry it throughout. The skin scurf and previous applied
medication can hinder the effective drug application and absorption. Remember to
wear gloves before application of medication on the skin and respect asepsis when
handling open skin area.To apply the medication on the skin we need the drug dedicated for skin, gloves,
some gauze, plate or trolly. In case of powder application make sure the skin
surface is dry. Spread apart any skin folds and apply the powder until the area
is covered with a fine thin layer. Cover the site with a dressing if ordered. For
suspension-based lotion, shake the container before use to distribute evenly
suspended particles. Put a little lotion on a small gauze dressing or pad and apply
the lotion to the skin by stroking it evenly in the direction of the hair growth. Rub the
lotion on the skin until it is no longer visible. For creams, ointments, pastes and
oil-based lotions: Warm and soften the preparation in gloved hands to make it
easier to apply. Spread over the affected skin evenly using long strokes that follow
the direction of the hair growth. Explain that the skin may feel somewhat greasy
after application. Apply a sterile dressing if ordered by the doctor.To apply transdermal patches, select a clean, dry area that is free of hair and
matches the manufacturer’s recommendations. Remove the patch from its
protective covering, holding it without touching the adhesive edges, and apply it by
pressing firmly with the palm of the hand for about 10 seconds. Advise the person
to avoid using a heating pad over the area to prevent an increase in circulation
and the rate of absorption same as when the patient has fever greater than 400c.
Remove the patch at the appropriate time, folding the medicated side to the inside
so it is covered. Remember to rotate the sites. Write date, time and your initials on
the patch guide your colleagues to take appropriate follow up care.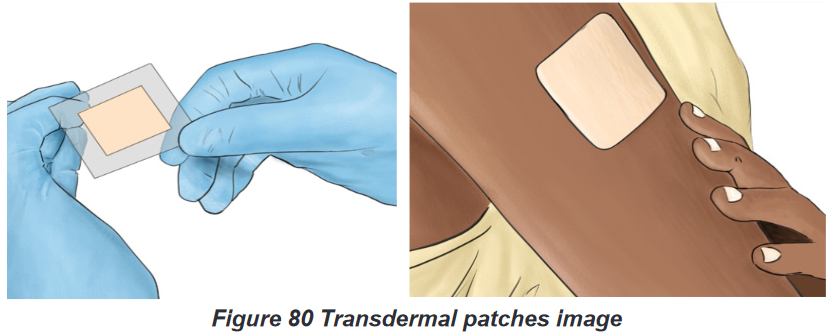
Self-assessment 5.6.
1) Before applying a powder medication, what are nursing consideration to
be respected?
2) Give different forms of skin application medication
3) Patient Y. consult for skin disorder and Dr prescribes a skin application
medication in form of cream to be applied twice a day. As an associate
nurse, give to Yvan the precautions to guide him to remove the patch.5.7. Eye medication administration
Learning activity 5.7.
Observe the image on the left and reply to these questions:
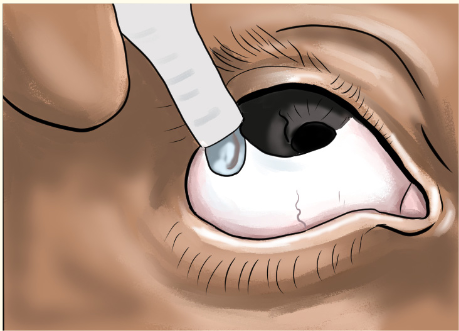
1) What this image indicates to you
2) Why is this action done?
3) Which safe measures will apply to make this activity?Medications become effective when they reach their site of action. Therefore, different
route of drug administration are used to reach the exact site of action. Ocular route
of drug administration is designed to treat eye diseases. Drugs administered to
the eye are in the form of drops or ointments and usually introduced into the lower
conjunctival sac. Eye medications may be ordered to lubricate the eye, to prevent
or treat conditions such as infection, inflammation or glaucoma or for diagnostic
purposes. E.g: of eye medications include gentamicin for bacterial infection such as
conjunctivitis, prednisolone for inflammation and timolol for glaucoma.The advantages of ocular route are that it offers direct application to the site of
action in higher concentration than when taken by other routes. It involves quicker
drug absorption and less systemic effect. It is also suitable to all type of patient as
well as easier for self-administration. The disadvantages quick elimination of drug
through tear and blink. Application of eye ointment may cause blurring vision. Few
drugs are in ocular form, they are also expensive than oral medication.BOX 5.7.
• Always remember to wash hands and if necessary, wear glove before
administer eye medications and follow other prescribers’ instructions.
• In some situations, the drug that is administered for a local effect may
be absorbed into the bloodstream and cause unwanted systemic effects.
To prevent this, after administration of the eyedrops, press your gloved
fingertip gently against the lacrimal ducts on either side of the nose for a
few secondsEye drugs are primarily in form of ointment and drops. Their administration methods
are different to ensure that they reach the maximum surface.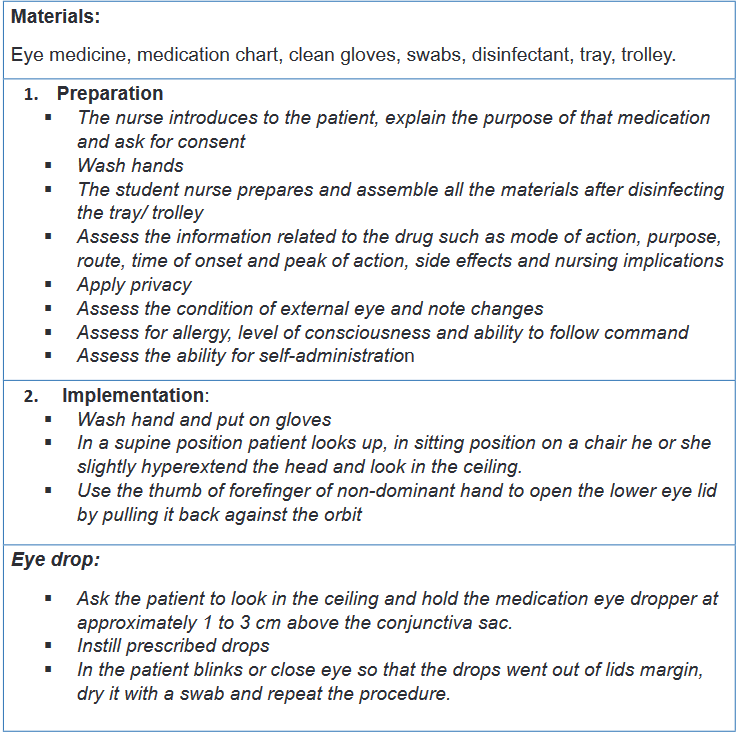
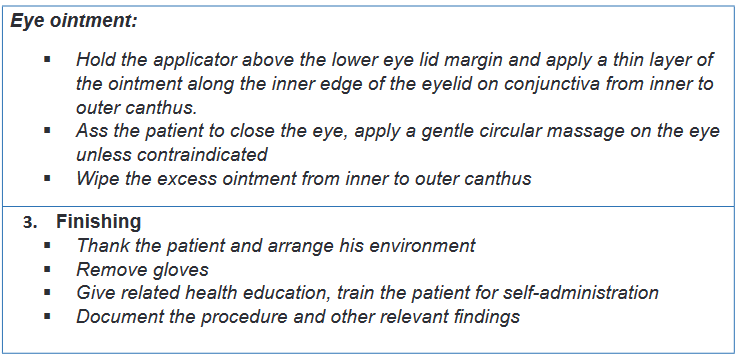
Self-assessment 5.7.
1) Explain the advantages and disadvantages eye medication administration
2) When is eye medication instillation indicated?
3) Patient K. consult for redness of the eyes and Dr prescribe an eye
ointment to be applied twice a day. As an associate nurse, give to K. the
precautions to be followed before and during medication application.5.8. Ear medications administration
Learning activity 5.8.
Look at the picture here attached and answer the given questions

1) What is this person doing
2) What do you think should the best way to instill ear drop?
3) Educate a patient whose ear drop prescription is to be taken at homeDrugs administered in the ear are in the form of drops. These drugs may be used
to soften cerumen, relieve pain, treat infection or inflammation, or facilitate removal
of a foreign body, such as an insect or a small object. It is important to control
local problems found in the ear. Its disadvantages are based difficulties for self-
administration as well as time consuming because the patient remain in a position
for a while.To instill eardrops, position the patient lying on his or her side with the affected ear
up. For adults and children older than 3 years of age, gently pull the pinna up and
back. For children younger than 3 years of age, pull the pinna down and back. This
helps straighten the ear canal, which allows the drops to penetrate to the middle
ear. Orients the dropper so that the medication drops rolls down the wall of the
canal and does not drop directly onto the tympanic membrane, which would cause
pain.Ask the patient to remain with his or her head positioned with the affected ear
up for at least 2 minutes. A cotton ball can be placed loosely in the ear to absorb
excess medication. It is advisable to avoid touching the dropper to the surface of
the ear to prevent the introduction of pathogens into the bottle of ear medication.
Before eardrops administration, make sure that tympanic membrane is intact. If in
doubt, ensure that the tympanic membrane has been examined with an otoscope
by a healthcare professional prior to administering the medication. Here is a list of
materials to be used to apply ear drug: ear medicine, ear dropper, medication chart,
clean gloves, swabs, disinfectant, trolley or plate.
Self-assessment 5.8.
1) Proper administration of an ear medication to a 2-year-old person
includes which of the following?
a) Pull the ear straight back
b) Pull the ear down and back
c) Pull the ear up and back
d) Pull the ear straight upwards
2) Describe the indications of ear medication instillation.
3) What are the disadvantages of ear drop?
4) Patient B. age 10 years old, consult the health center for right ear pain,
as an associate nurse what do you think the doctor can pay attention to,
before prescribing an ear drops?5.9. Nasal route of drug administration
Learning activity 5.9.
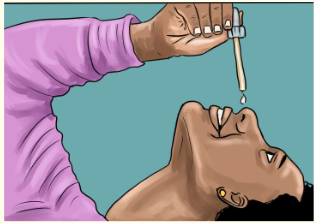
Look carefully the image posted here and respond related questions.
1) Where does this medication instilled?
2) Think on the importance of this route of drug administrationNasal route consists of drugs administration via the nasal mucosa. Some
medications are administered for local effects on the nasal mucosa other are given
for systemic effects and are simply absorbed through the nasal mucosa. Nasal
medications are administered to reduce inflammation, facilitate drainage, or treat
infections in the nasal cavity. Nasal route is contraindicated for patients with recent
radiation to the head and neck, high risk for serious bleeding due to tumour, history
of coagulopathy disorder.The advantages of easily administered and generally well tolerated, rapid onset
because medications are directly absorbed through the nasal mucosa into systemic
circulation. There is higher bioavailability than oral medications as first pass hepatic
metabolism is bypassed, may escape the blood-brain barrier through olfactory
region of the central nervous system. Provides alternate route for rapid medication
delivery when IV access is unavailable like in case of seizure or if there is a high risk
of needle-stick injury. Nasal drug administration is limited to very small volumes due
to relatively small area available for absorption. It only applicable to potent drugs
with high water solubility. It is not suitable for drugs that are irritating or injurious
to the nasal mucosa in addition to disease conditions of the nose may result in
impaired absorption. Instilling a drug into a blocked nose or a nose with watery
rhinorrhea may expel the medication from the nose. Chronic applications may lead
to more serious toxicity issues and may ultimately damage the cilia and compromise
body’s defenses. If long-term use continues, the arteries in the nasal passage will
shrink and scar, causing lesions and nosebleeds.Procedure of ear route drug administration
To perform the ear medication, we need materials such as medication in its
container, clean dropper, facial tissue, small pillow, wash cloth.
Self-assessment 5.9.
1) Explain the advantages and disadvantages nasal medication
administration.
2) When is nasal medication instillation indicated?
3) When is nasal medication instillation indicated?5.10. Vaginal route of drug administration
Learning activity 5.10.
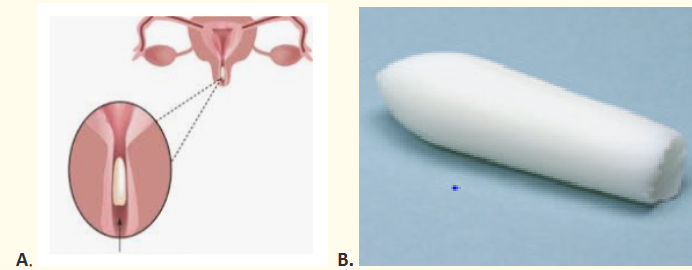
Observe the images above the work on the following questions:
1) What do you see introduced in the female genitalia?
2) Why is it important to introduce drug in female genitalia?
3) Which kind of medicines used in female genitalia?Healthy vaginal has many non-pathogenic organisms than pathogenic ones. This
ratio protects the vaginal from invasion by pathogenic organisms in addition to the
acidic vaginal secretion also protect the vagina from microbial invasion. There may
be an imbalance in the above protective mechanism which originate results into
diseases to be managed vaginal drugs.Vaginal drug administration indicates the administration of medications within the
vaginal cavity to produce local or less frequently, systemic pharmacological effects.
Medications administered via the vaginal route come in the form of suppositories,
creams, aerosol foams, or tablets that are inserted into the vagina and dissolve
there to treat infection or to relieve discomfort. Vaginal administration is indicated
to treat local infections such as yeast infections, vaginitis, endometrial atrophy,
labor induction and contraception with spermicidal agents.This route offers a number of benefits over other routes of drug delivery including
avoidance of hepatic first-pass effect because absorbed drugs penetrate directly
to the systemic circulation via the inferior vena cava thus prevent hepatic toxicity
induced by some drugs. It is an easier route of administration and possible
self-insertion and removal of the dosage form. This route limits the side effects
associated with oral route such unpleasant taste, nausea and so on as well as
parental routes associated inconvenience due to pain, tissue damage, and possible
risk of infection.However vaginal route has some disadvantages like gender specificity, patient
incompliance, some drugs can cause vaginal irritation. Only a few drugs are
administered by this route. Drug absorption may be affected by menstrual cycle,
menopause, pregnancy and sexual intercourse. It affects personal hygiene due to
some medication leakage and some drugs can be inactive due to vaginal pH. Some
preparations come with a disposable tubular applicator for insertion others are just
inserted by index and thumb fingers. Medical aseptic technique is usually used
during this procedure. Suppositories are designed to melt at body temperature, so
they are generally stored in the refrigerator to keep them firm for insertion.Procedure of vaginal administration
The following materials are needed to perform vaginal drug administration; vaginal
suppository, cream or tablets, applicator (if needed), clean gloves, tower, perineal
pad, lubricant, bedpan, medication chart.
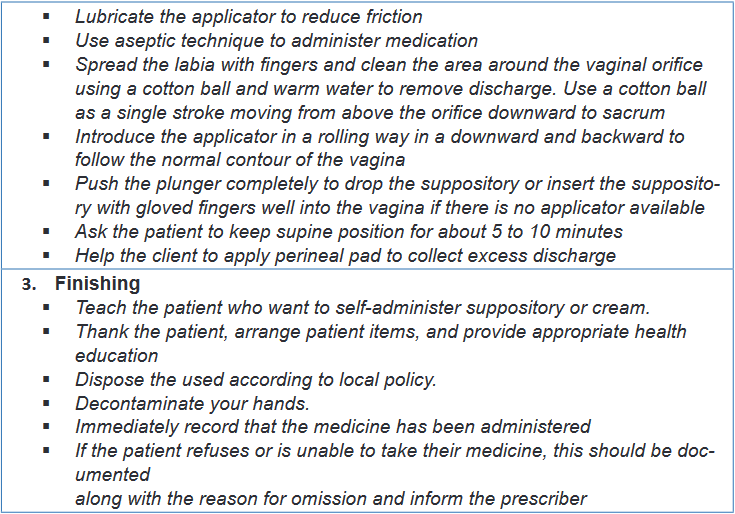
Self-assessment 5.10.
1) Explain the advantages and disadvantages vaginal administration.
2) When is vaginal medication indicated?
3) Patient C. has vaginal affection which require self-insertion of vaginal
suppository as treatment, as an associated explain her the procedure
she will follow.5.11. Drug dose calculation
Learning activity 5.11.
4) Dr. R. orders amoxicillin syrup 500 mg per feeding tube every 6 hours.
The available bottle of amoxicillin is labeled 250 mg per 5 ml.
How many milliliters needed to provide the prescribed dose of 500mg?
Calculate a daily dose for this patient.5) The prescription indicates 1000 milligrams (gm) of Erythromycin while
the available tablets are of 500gm per a tablet. How many tablets are
needed to meet the prescribed dose of 1000gm of Erythromycine?Nurses must be able to calculate the dose of medications so that the right dose is
appropriately provided to the patient. The dose of medication available to you may
be different from what the prescriber ordered. If the available medication is in a
different dose than what is ordered, you must calculate how much of the available
medication to administer to your patient. For tablets it is a matter of adding or
dividing tablets to meet the desired dose whereas for the capsule we add to get the
exact dose. For liquid medication, we calculate the amount of the drug dissolved in
liquid, expressed as milligrams per milliliter (mg/mL). You will then be required to
calculate how many milliliters of liquid to administer to give the desired milligrams
of medication. In this unit, we are going to study how to calculate the dose of
medications of different forms such as tablets, capsules, liquid forms including
injectable ones.To be able to calculate the drug dose, we have to know the abbreviations used
in drug prescription in addition to units converting process. We are going to see
the commonly used abbreviations in combination with conversion measures. It is
advisable from students to make sure what she or he is reading is correct or ask
clarification in case of confusing abbreviations to mitigate medication errors.BOX 5.11.
• To convert larger units to the smaller ones, requires to multiply.
Kiligrams (Kg)to Grams (g)=Kg×1000
Kilograms (kg) to grams(g)= Kg×1000
Grams to milligrams (mg) =g × 1000
Milligrams to micrograms (mcg) = mg ×1000
Liters(L) to milliliters(ml)= L ×1000
• To convert the smaller units to the larger ones, we divide.
Grams to kilograms = g/ 1000
Milligrams to grams = mg/1000
Microgram to milligrams = mcg/1000
Milliliters to liters = ml/100
Many ways of dose calculation are acceptable as their result into exact responses.
The calculations use simple mathematic formula which nurse need to be aware off
to ensure correct dose is ready for administration. It is necessary for students and
novice nurses to get guidance while performing dose calculation avoid confusion
and error which may arise leading medication error. To be able to find the dose to
administer (), we need the dose we have on hand () or the dose available, the dose
that is ordered by the prescriber () and () stands for the vehicle, which is either a
tablet or liquid.The first fraction is: H/V=D/x
The next step is to cross multiply: HX = VD
Now x equals to: X= DV/H = (Dose prescribed*vehicle)/(Dose in hand )
Example 1: The ophthalmologic officer MUGISHA orders 200 mg of Ibuprofen,
and 50 mg tablets are available, how many tablets should be given to the patient?
We know that 50 mg = 1 tablet,
We need 200 mg in an unknown number of tablets.
Step one: Set up a fraction operation: 50mg/(1 tab)=200mg/(x )
Step two: Do cross multiplication 50 mg * X= 1 tab *20 mg
Step three for ‘’x’’: X tab= (1tab * 200mg)/(50 mg )= 4 tabThe nurse needs four tablets to administer 200mg of ibuprofen using 50mg tablets.
Using simple explanation of this equation, the dose to administer equals the dose
we want times what is in over the dose we have.Here is a typical example:
Prescription states 200mg (milligrams)
You have an ampoule of 500mg (milligrams) in 4ml (millilitres).
What volume contains the dose you need?
H/V=D/x gives us; 500/(4 )=200/x; 500X=200*4; 500x= 800; x=800/500; x= 1.6It means that we need 1.6ml to be able to administer 200mg of the prescribed drug.
Self-assessment 5.11
1) Mrs. B have been prescribed the following medication: Cloxacillin 500mg
to be given 3 times a day for 7 days and Ibuprofen 400mg to be given
2 times a day for 3 days. The available cloxacillin in health center’s
pharmacy has 500mg per capsule while ibuprofen is 200mg per tablet
a) Calculate the daily and total dose of cloxacillin for Benitha
b) Calculate the daily dose and total dose of Ibuprofen for Benitha2) Dr. I. writes a prescription for 25 mg of morphine in SC every 12 hours.
The medication is available in a concentration of 100 mg per ml. How
many ml will the nurse administer to meet the prescribed dose?End unit assessment 5.
1) Select the right of medication administration among the following
concepts:
a. Patient file
b. Concentration
c. Route
d. Thermometer2) Proper administration of an ear medication to a 2-year old person
includes which of the following?
a. Pull the ear straight back.
b. Pull the ear down and back.
c. Pull the ear up and back.
d. Pull the ear straight upwards.3) The administration route for a drug injected just beneath the top layer
of the skin is called:
a) Intradermal
b) Subcutaneous
c) Vaginal application
d) Transdermal application4) The drug administration route where the needle is inserted at 45 degrees is:
a) Intradermal
b) Subcutaneous
c) Intramuscular
d) Sublingual5) If blood appears in the syringe when the plunger is pulled back during
subcutaneous and intramuscular injections the nurse should
a) Inject drug
b) Inject drug followed by a small amount of bubble air
c) Insert needle one cm further
d) Start over with new syringe
e) Ignore it because the presence of blood has no significance6) Drug administration way which is least expensive, using little equipment,
and minimal training is the:
a) Enteral route
b) Skin application
c) Vaginal application
d) Intradermal route7) Intramuscular injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 9008) Hand Hygiene is a part of standard precautions before any nursing
procedure
a) True
b) False9) Intradermal injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 90010) How much medication can the nurse safely administer into the deltoid
muscle?
a) 4 ml
b) 1-2 mL
c) 10 ml
d) 2-3 mL11) When giving injections in the buttocks the nurse must properly identify
appropriate land marks to prevent damage to the ___
a) Sciatic nerve
b) Spinal cord
c) Coccyx
d) Atlas12) Nurse Carine has completed giving Ms. Smith her injection. Which
method is the BEST method for Nurse Carine to use to dispose of the
needle after giving the injection?
a. Nurse Carine should sit the needle on the bedside table and make
sure she disposes of the needle before she leaves the room.
b. Nurse Carine should immediately discard used needle in the nearest
sharps container.
c. Nurse Carine should discard needle when she completes the
injection.
d. Nurse Carine should recap needle and place into the nearest sharps
container.13) What is most important reason to press firmly but not to massage an
applied medicated patch?
a. Massaging a medicated patch can result in the untimely release of
medication.
b. Massaging a medicated patch can cause the medicated patch to
become dislodged.
c. Massaging a medicated patch can result in skin irritation.14) You go to place a transdermal patch on Mrs. LOWERY and note that the
patch from yesterday is still applied to her chest.
a. As an associate nurse, what do you expect to find on the applied
patch?
b. How long a transdermal patch should last?15) Nurse AKALIZA is going to administer amoxicillin to Mr. KALISA through
enteral route,
a. Discuss different ways of enteral route should be used to administer
a medication.
b. Outline the advantages and disadvantages of each enteral route16) The Dr. prescribe to Mr. JO an injectable cyanocobalamin 10mg to be
administered in intramuscular, the available vial has a concentration of 2
mg/1 ml.
a. Calculate the correct volume of cyanocobalamin to be administered
to Mr. JO.
b. Discuss the advantages and disadvantages of IM injection?
c. What are the indications and contra indications of IM route of drug
administration?d. Give 3 nursing considerations before administer a prescribed
medication to MR JO.
e. What are the complications may be associated to associated to IM
injection17) Describe the process used to perform each of the topical drug
administration.18) Name the materials used in IM technique of medication administration
19) When assessing a person’s response to medication therapy, how
does the nurse best recognize that the medication is therapeutic or
subtherapeutic?20) How do Three Checks facilitate a culture of safety in medication
administration?21) Mrs. LOWERY prefers to insert her own nose drops. As you observe her
doing so, what key aspects of the administration procedure should she
be doing to ensure correct technique?22) Subcutaneous route of drug administration consists of deposits the
medication into the subcutaneous layer below the skin, give out the 3
commonly used site in this route.23) Outline the 3 indications of rectal drug administration route
24) ISARO and KEZA, 3 and 7 years old girls admitted in general word of
pediatric unit. ISARO has persistent fever of 38.70C whereas KEZA
is having vomiting and diarrhea. The physician prescribed for ISARO,
paracetamol 250mg to be inserted in anus three times a day. KEZA
received Metronidazole 500mg by mouth to be taken 2 times a day. The
word nurse is coming for a new shift, is assigned to care for the above
patients. She read their files and discover that it is time to give medication
to ISARO. She went in the patients’ room and starts identifying these
children by asking the mothers and compare the names on the files.
She takes body temperature of Isaro and finds that it is now 38.30C. She
approaches the ISARO’S mother to explain that her child is still having
fever and a need to administer the paracetamol 250mg to control fever.
The mother accepts the request of the nurse. She then takes the drug
from patient’s box and prepare it and introduce in the anus of ISARO as
it was written in the file. She thanks the patient and write this activity in
the patient file. After 30 minutes she returned to ISARO and take again
her body temperature which is now 37.20C. Finally reassure the mother
on the effectiveness of the medication.a) What are the key actions done by the nurse while caring for
ISARO?
b) Which route of drug administration used in this case?
c) Compare and contrast the intramuscular to intradermal routes of
drug administration.UNIT 6: DATA COLLECTION
Key unit competence:
Carry out a comprehensive data collection of clientsIntroductory activity 6
Look at the figures (A, B, C, D, E and F) and reflect on the activity below:
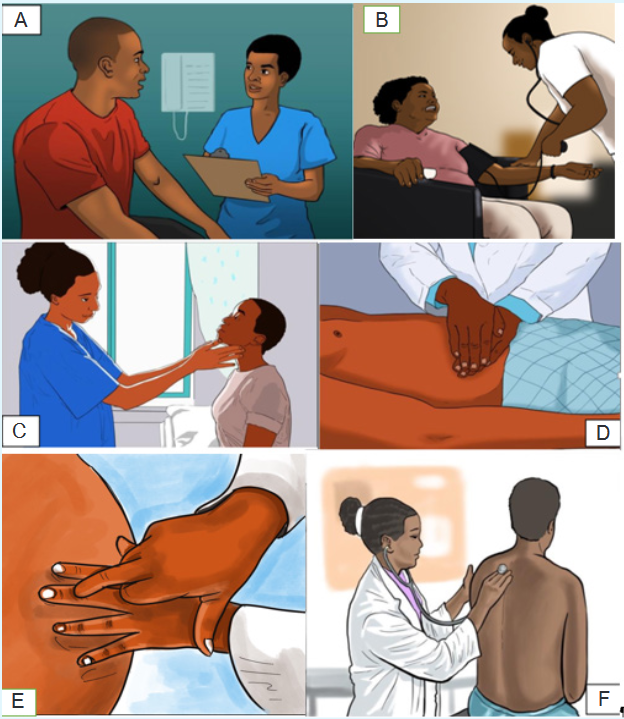
1) Referring to the figure A, what do you think is the Nurse doing?
2) What do you think is the Nurse doing in figure B, C, D, E and F?
3) According to you, what is the purpose of doing all the above actions
(Figures A, B, C, D,E and F) by the Nurse to the client?6.1. Introduction to data collection
Learning activity 6.1.
Use the provided books of Fundamentals of Nursing, read about data collection
or assessment and make a short note on the following
1) Definition of data collection?
2) Purpose of data collection or assessment
3) Sources of data
4) Types of data
5) Types of assessment
6) Methods of data collection
After, you will present your work in class6.1.1. Definition and purpose of data collection
Data collection or assessment means the gathering of information (data) about a
patient in order to facilitate effective nursing care and medical management. The
purpose of assessment is to establish a database concerning a client’s physical,
psychosocial, and emotional health in order to identify health-promoting behaviors
as well as actual and potential health problems.6.1.2. Types of assessment
The assessment can be comprehensive or focused (ongoing).
A comprehensive assessment is usually the initial assessment. It is usually
performed upon admission to a health care agency and includes a complete
health history and physical examination to determine current needs of the client. A
comprehensive assessment examines the patient’s overall health status. A focused
or ongoing assessment is frequently performed on an ongoing basis to monitor
and evaluate the patient’s progress, interventions, and response to treatments. A
focused assessment is problem oriented and may be the initial assessment or an
ongoing assessment. Focused assessments are not as detailed as comprehensive
assessments. The nurse and physician both perform a patient history and a physical
examination, but they use different formats and analyze the data based on their
discipline’s focus.6.1.3. Types of data
In all assessments, only two types of data are obtained: Subjective and Objective
data.Subjective data, also known as symptoms, are collected by interviewing the patient
and/or caregiver during the nursing history. This type of data includes information
that can be described or verified only by the patient or caregiver. It is what the
person tells you either spontaneously or in response to direct questioning. Objective
data, also known as signs, are data that can be observe or measured. You obtain
this type of data using inspection, palpation percussion, and auscultation during
the physical examination. Objective data are also acquired by diagnostic testing.
Usually subjective data are obtained by interview, and objective data are obtained
by physical examination.6.1.4. Sources of data
Data are collected from a variety of sources where the client is considered the
primary source of data (the major provider of information about self). Sources of
data other than the client are considered secondary sources and include family
members, other health care providers, and medical records. Examples of sources
of data are: Client, Family and significant other, Other health care professionals,
Medical records, Interdisciplinary conferences, rounds, and consultations, Results
of diagnostic tests, Relevant literature.6.1.5. Methods of data collection
Assessment requires sharp observation skills and the ability to distinguish relevant
from irrelevant and important from unimportant data. Data collection can occur
through interviews, observation, and physical assessmentSelf-assessment 6.1.
1) What is data collection?
2) With examples, differentiate primary and secondary sources of data
3) With examples, differentiate the subjective and objective data
4) What are the main components of a comprehensive client assessment?
5) How does comprehensive assessment differ from focused assessment?
6) List the methods of data collection6.2. Interview and Health History: Subjective Data
CollectionLearning activity 6.2.
For Overview:
Use the provided books of Fundamentals of Nursing, read topics about
interview and Health History and make a summary note on the following:
1) Definition of interview
2) Phases of the interview
3) Interviewing techniques
4) Definition of health history
5) Purpose of health history
6) Description of components of health historyAfter, you will present your work to your classmates
For the technique of taking the health history:
Through role play, two paired learners will follow the interview phases and use
effective interviewing skills/techniques to take the health history of his/her partner6.2.1. Interview
Interviewing is the method by which health care providers take health histories and
gather subjective data. Interview is a therapeutic interaction that has a specific
purpose. A primary focus of the data collection interview is the health history. The
nurse interviews for a variety of reasons throughout the nurse-client relationship,
including data collection, teaching, exploration of the client’s feelings or concerns,
and provision of support. Effective interviewing depends on the nurse’s knowledge
and ability to skillfully elicit information from the client using appropriate techniques
of communication. Observation of nonverbal behavior during the interview is also
essential to effective data collection.a) Phases of the interview
The interview is divided into three phases: the introductory phase, the working
phase, and the termination phase. Each phase has a specific purpose and different
communication patterns.i) Introductory phase
The introductory phase is the time to introduce yourself to your patient, put him or
her at ease, and explain the purpose of the interview and the time frame needed to
complete it. The nurse also asks the patient his or her preferred name. The nurse
shakes hands if that seems comfortable with the patient and is appropriate for culture
and setting. The beginning phase may continue with discussion of neutral topics
(eg, the weather) if the patient seems anxious. Questions should be nonprobing
and patient centered. Explain to the patient that you will be taking notes, but keep
your writing to a minimum. Reassure your patient that the information collected is
confidential.ii) The Working Phase
The working phase is often where data collection occurs. It is usually very
structured; it is also the longest phase. Make sure you allow enough time for the
working phase. Although you will need to take notes, stay focused on your patient.
Listen to what the patient is saying both verbally and nonverbally. With experience,
you will become skilled at taking minimal notes and then documenting your data
after the interview rather than during it. During the working phase the nurse asks
specific questions, two types of which are closed ended and open ended. Each has
a purpose, which the nurse chooses to elicit appropriate responses. Closed-ended
(direct) questions yield “yes” or “no” answers. An example is “Do you have a family
history of heart disease?”. Closed -ended questions are important in emergencies
or when a nurse needs to establish basic facts. Open-ended questions require
patients to elaborate. They are broad and provide responses in the patient’s own
words. They are key to understanding symptoms, health practices, and areas
requiring intervention.iii) The Termination Phase
The end of the interview is the termination or closing phase. During this phase, you
need to summarize and restate your findings. This provides an opportunity to clarify
the data and share your findings with the patient. The nurse also ends the interview
by stating what the two to three most important patterns or problems might be, as
well as asking patients if they would like to mention or need anything else. Based
on this information, both the nurse and the patient can discuss follow-up plans.
The nurse also thanks patients and family members for taking the time to provide
information.d) Interviewing techniques
Begin the interview by establishing trust and conveying a caring attitude. Make
sure that the environment is comfortable and that privacy is ensured with minimal
distractions. Effective interviewing skills evolve through practice and repetition and
include the following:Active listening: is the ability to focus on patients and their perspectives. It requires
the nurse to constantly decode messages, including thoughts, words, opinions, and
emotions.Restatement: relates to the content of communication. The nurse makes a simple
statement, usually using the same words of patients. The purpose is to ask patients
to elaborate.Reflection: is similar to restatement; however, instead of simply echoing the
patient’s comments, the nurse summarizes the main themes. Patients, thus, gain
a better understanding of underlying issues, which helps to identify their feelings.Encouraging elaboration (facilitation): assists patients to more completely
describe problems. Responses encourage patients to say more, continue the
conversation, and show patients that the nurse is interested.Purposeful silence: allows patients time to gather their thoughts and provide
accurate answers. Silence can be therapeutic, communicating nonverbal concern.
It gives patients a chance to decide how much information to disclose.Focusing: helps when patients stray from topic and need redirection. It allows the
nurse to address areas of concern related to current problems.Clarification: is important when the patient’s word choice or ideas are unclear.
Summarizing: happens at the end of the interview, when the nurse reviews and
condenses important information into two or three of the most important findings.
Doing so also helps to reassure the patient that he or she has been heard accurately.6.2.2. Health History
The health history is a review of the client’s functional health patterns prior to the
current contact with a health care agency. In other words, the health history is a
record of information about a person’s health. Health history provides the subjective
database for your assessment. The health history is subjective, it consists of what the
patient tells you, what the patient perceives, and what the patient thinks is important.
It provides a holistic, qualitative picture of your patient. All history information isconsidered subjective data. Clues that you obtain from the health history will direct
your physical assessment and are essential in developing a successful plan of
care for your patient. While the medical history concentrates on symptoms and the
progression of disease, the nursing health history focuses on the client’s functional
health patterns, responses to changes in health status, and alterations in lifestyle.a) Purpose of Health history
The purpose of the health history is to:
Provide the subjective databased
Identify patient strengths
Identify patient health problems, both actual and potential
Identify supports.
Identify teaching needs.
Identify discharge needs.
Identify referral needsb) Components of Health History
Components of the Nursing Health History are:i) Biographical Information
Biographical information is factual demographic data that include a patient’s age,
gender, address, insurance information, occupation, working status, marital status,
and referral source. The staff who works in the admitting office usually collects this
information.ii) Chief Concern or Reason for Seeking Health Care
The chief concern is a brief statement about why a patient (in his or her own
words) is seeking health care. This information offers a focus to explore a patient’s
concerns and issues. Once you learn a patient’s chief concerns, you will compare
those findings with what you learn during your assessment. Often you will learn
much more.Ask a patient why he or she is seeking health care (e.g., “Tell me, Ms. Richard,
what brought you to the clinic today?”). Once you learn a chief concern, you then
gather more comprehensive data and probe for a full description of the patient’s
health status. You record a patient’s response in quotations to indicate a subjective
statement. As you explore a patient’s reason for seeking health care, you will learn
the chronological and sequential history of his or her health problems.iii) Patient Expectations
It is important to assess a patient’s expectations of health care providers (e.g.,
being diagnosed correctly, obtaining pain relief, or being treated for a disease).Patient satisfaction, a standard measure of quality for all hospitals throughout the
country, can be perceived by patients as poor if their expectations are unmet.Patients typically expect to receive information about their treatments, prognosis,
and a plan of care for their return home (whether they are inpatients or outpatients).In addition, they expect relief of pain and other symptoms and to have caring
expressed by health care providers.During the initial interview have a patient express expectation when entering the
health care setting. Later, as the patient interacts with health care providers, assess
whether these expectations changed or were met.iv) History of the Present Illness or Health Concerns
The nurse begins with open-ended questions and asks patients to explain
symptoms. A complete description of the present illness is essential. Questions
about symptoms (subjective sensations or feelings of patients) in six to eight
categories assist patients to be more specific and complete: location, duration,
intensity, description, aggravating factors, alleviating factors, pain goal, and
functional impairment.Common mnemonics used to remember the key elements of the presenting
symptom(s) are OLDCARTS (Onset, Location, Duration, Character, Associated/
Aggravating factors, Relieving factors, Timing, Severity) and PQRSTU (Provocative/
Palliative, Quality, Region, Severity, Timing, Understanding patient perception).P—Provokes (precipitating and relieving factors): How did it come about? What
might be the causes for the symptom? What makes it better or worse? Are there
activities ( e.g., exercise, sleep) that affect it?Q—Quality: What does the symptom feel like? (Have the patient explain in his or
her own words.) If the patient has difficulty in describing symptoms, offer probes
(e.g., “Is the pain sharp? Dull?” or “Do you feel light-headed, dizzy, off balance?”).
What does the illness or symptom mean to the patient?R—Radiate: Where is the symptom located? Is it in one place? Does it go anywhere
else? Have the patient be as precise as possible.S—Severity: Ask a patient to rate the severity of a symptom on a scale of 0 to 10
(with no symptom at 0 and the worst intensity at 10). This gives you a baseline with
which to compare in follow-up assessments.T—Time: Assess the onset and duration of symptoms. When did a symptom start?
Does it come and go? If so, how often and for how long? What time of day or on
what day of the week does it occur?Also assess whether the patient is experiencing other symptoms along with the
primary symptom. For example, does nausea accompany pain? Does the patient
have pain along with shortness of breath?v) Past Health History
A health history provides a holistic view of a patient’s health care experiences
and current health habits. Assess whether a patient has ever been hospitalized or
injured or has had surgery. Has any illness or injury limited the patient’s ability to
function? Include a complete medication history (including past, current, and recent
medications). Review the use of any prescription medications, herbal supplements,
etc. Also essential are descriptions of allergies, including allergic reactions to food,
latex, drugs, or contact agents (e.g., soap).Asking patients whether they have had problems with medications or food clarifies
the type and amount of agent, the specific reaction, and whether a patient has
required treatment.If the patient has an allergy, note the specific reaction and treatment on the
assessment form and the special armband provided. When considering allergies,
also ask if the patient has ever had a blood product transfusion and whether any
reactions occurred.The history also includes a description of a patient’s habits, emotional status, and
lifestyle patterns. Assessing for the use of alcohol, tobacco, caffeine, or recreational
drugs (e.g., methamphetamine or cocaine) determines a patient’s risk for diseases
involving the liver, lungs, heart, or nervous system.vi) Family History
The family history includes data about immediate and blood relatives. Your objective
is to determine whether a patient is at risk for illnesses of a genetic or familial nature
and to identify areas of health promotion and illness prevention.For example, a patient with a strong family history of breast cancer will be
recommended to pursue mammography more often, and female children may be
recommended for genetic counselling.vii) Psychosocial profile
The psychosocial profile focuses on health promotion, protective patterns, and roles
and relationships. It includes questions about healthcare practices and beliefs, a
description of a typical day, a nutritional assessment, activity and exercise patterns,
recreational activities, sleep/rest patterns, personal habits, occupational risks,
environmental risks, family roles and relationships. Details on the psychosocial
profile is described in the next lesson of bio-psycho-social model.viii) Spiritual Health
Life experiences and events shape a person’s spirituality. Review with patients their
beliefs about life, their source for guidance in acting on beliefs, and the relationship
they have with family in exercising their faith.Also assess rituals and religious practices that patients use to express their
spirituality.Patients may request availability of these practices while in a health care setting.
ix) Review of Systems
The review of systems (ROS) is a systematic approach for collecting subjective
information from patients about the presence or absence of health-related issues
in each body system.The ROS is used to obtain the current and past health status of each system and
to identify health problems that your patient may have failed to mention previously.
Remember, if your patient has an acute problem in one area, every other body
system will be affected, so look for correlations as you proceed with the ROS.During the ROS ask the patient about the normal functioning of each body system
and any noted changes.Use a series of questions to assess each system as needed. For example, the
review of the skin, hair, and nails includes assessment of whether a patient has
noticed any rash or skin lesions or has itching or abnormal nail or hair growth.Self-assessment 6.2.
1) You are obtaining a health history on a newly admitted patient with the
diagnosis of congestive heart failure. He tells you, “I’m having trouble
breathing since yesterday.” Once the chief complaint is identified, which
part of the history should be completed next?
a) Symptom analysis
b) Past health history
c) Review of systems
d) Family history2) Which section of the health history identifies environmental health risk
factors?
a) Review of systems
b) Psychosocial profile
c) Past health history
d) Family history3) What is the purpose of the review of systems in the health history?
a) Identify actual problems
b) Determine cause of current problem
c) Identify current/past health of systems
d) Validate current symptoms4) Mr. Brunner, 35 years old, is complaining of abdominal pain. You perform
a symptom analysis of the abdominal pain. Which question would best
assess the severity of the pain?
a) Is the pain really bad?
b) On a scale of 0 to 10, rate the pain
c) Does the pain feel knifelike?
d) Does the pain go anywhere else?5) Mr. Brunner, 35 years old, is complaining of abdominal pain. You perform
a symptom analysis of the abdominal pain. Which question would best
assess the quality of the pain?
a) What does it feel like?
b) Is the pain sharp?
c) When did the pain start?
d) Does the pain go anywhere else?6.3. Bio-Psycho-Social model to collect holistic client
dataLearning activity 6.3.
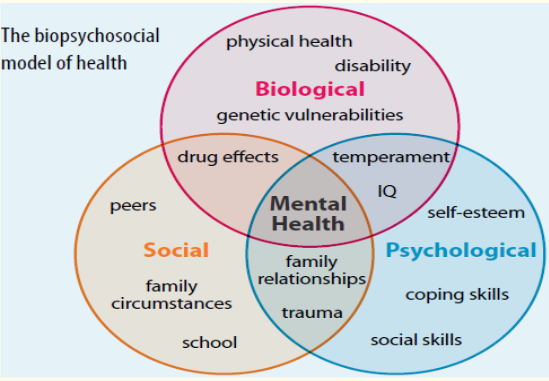
Look at this Biopsychosocial model of health conceptualized by George Engel
in 1977, read the Fundamentals of Nursing book (topic on psychosocial profile
under the Health History) for additional information about the model and answer
the following questions:
1) Define the Biopsychosocial model
2) Describe the domains of the Biopsychosocial model
3) Explain how the Biopsychosocial model can be integrated while
assessing the clientAfter you will present your work in class
6.3.1. Introduction
The biopsychosocial model is an inter-disciplinary model that looks at the
interconnection between biology, psychology, and socio-environmental factors.
The biopsychosocial model was first conceptualized by George Engel in 1977,
suggesting that to understand a person’s medical condition it is not simply the
biological factors to consider, but also the psychological and social factors. The late
George Engel also believed that to understand and respond adequately to patients’
suffering, the healthcare provider must attend simultaneously to the biological,
psychological, and social dimensions of illness. This model is attributed to improvepatient care, compliance, and satisfaction. This model is important to remember
the World Health Organization defines health as complete well-being, not just the
absence of disease.6.3.2. Domains of the Biopsychosocial model of health
Three domains of the Biopsychosocial model are: biology, psychology, and
sociology.Biology: Bio (physiological pathology). Biological factors involve genetics,
physiology, chemistry, and neurology. Psychology: Psychological factors involve
a person’s personality, thoughts, and ensuing emotions and behaviour such as
psychological distress, fear/avoidance beliefs, current coping methods and
attribution. Social: Social factors involve socio-economical, socio-environmental,
and cultural factors that affects a person’s thoughts, feelings, and behaviour such
as work issues, family circumstances and benefits/economics.According to Gurung, 2014, some of the factors that fall under Biological are:
Gender, Physical Illness, Disability, Genetic Vulnerability, Immune Function,
Neurochemistry, Stress Reactivity and Medication Effects. Some of the factors that
fall under Psychological are: Learning & Memory, Attitudes & Beliefs, Personality,
Cognitions, Behaviors, Emotions, Coping Skills and Past Trauma. Some of the
factors that fall under Social are: Social Support, Family Background, Cultural
Traditions, Socioeconomic Status, Education, Society, and community6.3.3. Biopsychosocial assessment
The psychosocial assessment focuses on health promotion, protective patterns,
and roles and relationships. It includes questions about healthcare practices and
beliefs, a description of a typical day, a nutritional assessment, activity and exercise
patterns, recreational activities, sleep/rest patterns, personal habits, occupational
risks, environmental risks, family roles and relationships, and stress and coping
mechanisms. The psychosocial assessment enables you to identify how your
patient incorporates health practices into every aspects of her or his life. This will
therefore help you in teaching and reinforcing health promotion activities that your
patient can incorporate into her or his everyday life.During the biopsychosocial assessment, interview questions are related to its three
domains, namely biology, psychology, and sociocultural influences.For biology domain, questions will address biological aspects that may include
diet, sleep habits, and family history. Some examples of biology questions are as
follows:
Do you currently take any prescription medication or supplements? If yes,
what are they?
Do you have any current medical problems that you believe significantly
impact your life?
Is there a family history of significant medical problems or disease? If yes,
what are they?For the psychology domain, questions will address current cognitive functioning,
coping skills, and mood. Examples of psychology questions are: (1) How would
you describe your mood? Do you have a history of suicidal thoughts or acts of self-
harm? (2) Do you have a family history of psychiatric illness? (3) Name three of
your strengths and three of your weaknesses.For social domain, questions may address the quality of family relationships,
financial stability, and educational background. Examples of social questions are
the following: (1) Do you have close relationships with family members? Do you
find them a source of emotional support? (2) Do you currently have a job? Does it
provide you personal satisfaction and financial stability? (3) What is happening in
your life right now that increases your stress level? What about in the past?6.3.4. Benefits of the biopsychosocial model
The biopsychosocial approach can be applied to understand a variety of health
behaviors. For example, the biopsychosocial approach can be used to understand
the health behavior of excessive drinking. A person may excessively drink because
they have a genetic disposition for an addiction to alcohol (Biological). A person
may be struggling with negative emotions and use alcohol as a coping mechanism
(Psychological). A person may also be prone to drink excessively when they are
with friends that also drink excessively (Social).The Biopsychosocial approach can also be used in understanding what determines
health behaviors. It is a beneficial approach because it looks at all the possible
biological, psychological, and social influences affecting overall health and health
behaviors.Self-assessment 6.3.
) Explain the three domains of the biopsychosocial model of health?
2) During history taking a nurse asks this question to the client “Do you find
your family members a source of emotional support?” In which domain of
the biopsychosocial model this question belongs?
a) Biology domain
b) Psychology domain
c) Social domain
d). Psychosocial domain
3) What does the biopsychosocial model serve for during client assessment?6.4. Introduction to physical examination
Learning activity 6.4.
Use the provided textbooks of Fundamentals of Nursing and read topics about
Physical Examination and make a summary note of the following:
1) Definition of physical assessment.
2) Description of purposes of physical assessment.
3) Physical and psychological preparation of the patient for physical
assessment
4) Explanation of different vital signs and parameters6.4.1. Definition of Physical Examination
A physical examination is an investigation of the body to determine its state of
health. The examination involves use of the techniques of inspection, palpation,
percussion, auscultation, and smell. In other words; Physical assessment is the
process you use to collect physical data that are relevant to the patient’ s health.To collect physical data about the patient’s current condition, you will perform a
physical examination of the patient, using four of your senses: sight, smell, hearing,
and touch.Nurses perform systematic physical assessments on a regular basis in nearly every
health care setting. In acute care settings you will perform more comprehensive
assessments when patients are admitted to agencies and brief physical assessments
at the beginning of each shift to identify changes in a patient’s status for comparison
with the previous assessmentA routine physical assessment takes 10 to 15 minutes and reveals information that
supplements a patient’s database.Nurses are often the first to detect changes in patients’ conditions. For this reason,
the ability to think critically and interpret patient behaviours and physiologic changes
are essential.The skills of physical assessment are powerful tools for detecting both subtle and
obvious changes in a patient’s health.Although you may use additional tools to assist you in assessment, the most
important tools you will need are your eyes, ears, hands, nose, and critical thinking
ability.When use of the four senses produces evidence of illness or injury, the findings are
objective and measurable, and are classified as signs.When evidence of illness or injury is verbalized by the patient, the findings are
subjective, not directly measurable, and classified as symptoms.In other words, signs of disease are those that can be detected by the nurse, while
symptoms of disease are apparent only to the patient, so they must be verbally
communicated by the patient to the nurse.A complete examination includes a patient’s height, weight, vital signs, and a head-
to-toe examination of all body systems.The data from a hands-on physical assessment allow you to collect valuable
objective information needed to form accurate diagnostic conclusions.Always conduct an examination competently with a caring and culturally sensitive
approach.6.4.2. Purposes of the Physical Examination
A physical examination is conducted as an initial evaluation in triage for emergency
care; for routine screening to promote wellness behaviours and preventive health
care measures; to determine eligibility for health insurance, military service, or a
new job; or to admit a patient to a hospital or long-term care facility.After considering the patient’s current condition, a nurse selects a focused physical
examination on a specific system or area. For example, when a patient is having a
severe asthma episode, the nurse first focuses on the pulmonary and cardiovascular
systems so treatments can begin immediately.When the patient is no longer at risk for a bad outcome or injury, the nurse performs
a more comprehensive examination of other body systems.For patients who are hospitalized, a nurse integrates the collection of physical
assessment data during routine patient care, validating findings with what is known
about the patient’s health history. For example, on entering a patient’s room a
nurse may notice behavioral patient cues that indicate comfort, anxiety, or sadness;
assess the skin during the bed bath; or assess physical movements and swallowing
abilities while administering medications.Purpose of physical assessment
Physical assessments are performed for several purposes:
To establish the patient’s current condition, a baseline against which future
changes may be measured
To identify problems the patient may have or have the potential to develop
To evaluate the effectiveness of nursing interventions or the outcomes of care
To monitor for changes in body function
To detect specific body systems that need further assessment or testing6.4.3. Preparation of the patient for physical assessment
a) Physical Preparation of the Patient
Gather the necessary equipment to perform the assessment, including;
a stethoscope, sphygmomanometer, thermometer, pulse oximeter, and
penlight.
Upon entering the patient’s room, ask any visitors to step out into the hallway
or waiting room.
Close the door, provide privacy, and explain what you are about to do.
To show respect for a patient, ensure that physical comfort needs are met.
Before starting, ask if the patient needs to use the restroom.
Give the patient time to empty the bowel or bladder if needed. An empty bladder
and bowel facilitate examination of the abdomen, genitalia, and rectum.
If you require urine or stool specimens, now is a good time to collect them.
Be careful to protect the patient’s modesty by keeping the patient covered
with a sheet, except for the body part that is being assessed.
Make certain the room temperature is comfortable for the patient.
Maintain a professional demeanor at all times.
Speak in a relaxed tone of voice and exhibit a relaxed facial expression.These preparatory steps serve to gain the patient’s cooperation and decrease his
or her anxiety.Physical preparation involves making certain that patient privacy is maintained with
proper dress and draping. The patient in the hospital likely is wearing only a simple
gown. In the clinic or health care provider’s office the patient needs to undress and
usually is provided with a disposable paper cover or paper gown.If the examination is limited to certain body systems, it is not always necessary for
the patient to undress completely. Provide the patient privacy and plenty of time to
undress to avoid embarrassment. After changing into the recommended gown or
cover, the patient sits or lies down on the examination table with a light drape over
the lap or lower trunk.Make sure that he or she stays warm by eliminating drafts, controlling room
temperature, and providing warm blankets. Routinely ask if he or she is comfortable.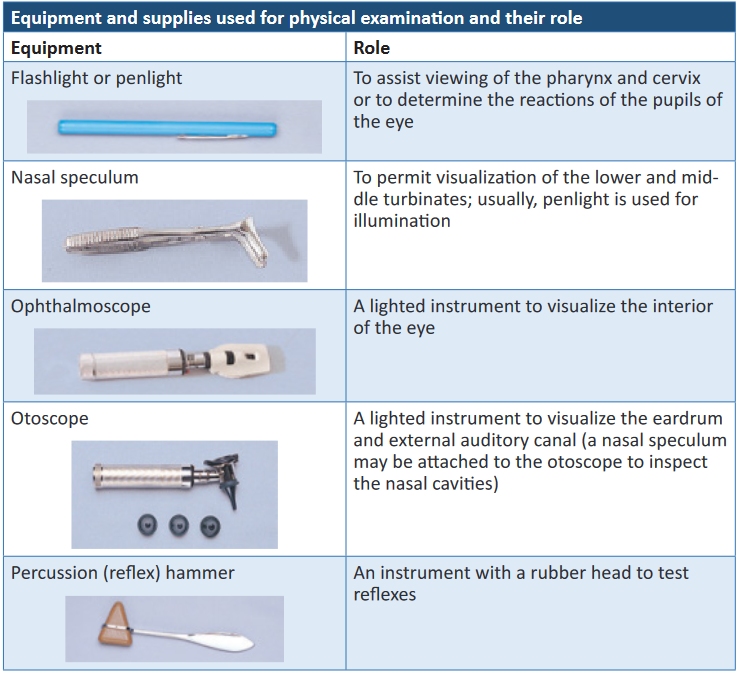
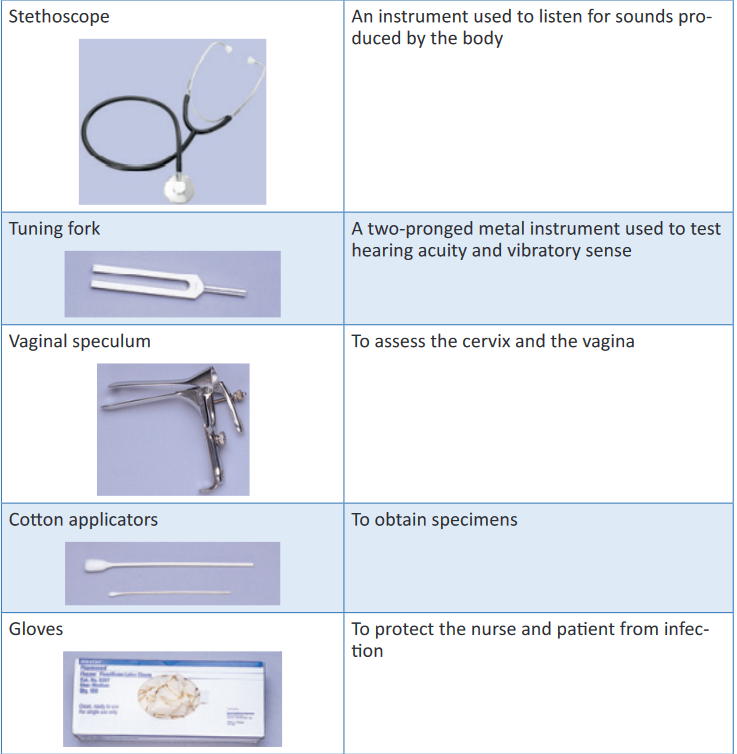
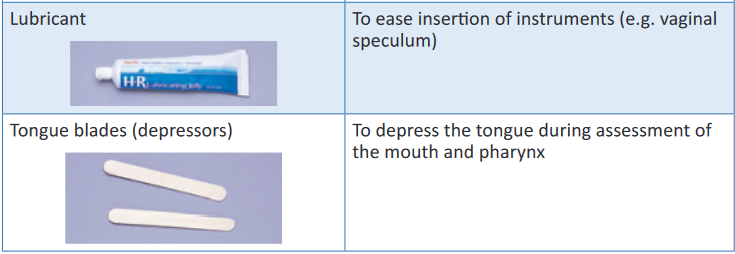
Other equipment and supplies that may be needed are: Disposable pad/paper
towels, Drapes/cover, Forms (e.g., physical, laboratory), Gown for patient, Pulse
oximeter, Scale with height measurement rod, Specimen container, slides, wooden
or plastic spatula, and cytological fixative if needed, Tape measure and Watch with
second hand or digital display.b) Psychological preparation of the patient
Many patients find an examination stressful or tiring, or they experience anxiety
about possible findings. A thorough explanation of the purpose and steps of each
assessment lets a patient know what to expect and how to cooperate.Adapt explanations to the patient’s level of understanding and encourage him or
her to ask questions and comment on any discomfort.Convey an open, professional approach while remaining relaxed.
A quiet, formal demeanor inhibits the patient’s ability to communicate, but a style
that is too casual may cause him or her to doubt an examiner’s competence.During the examination, watch the patient’s emotional responses by observing
whether his or her facial expressions show fear or concern or if body movements
indicate anxiety.When you remain calm, the patient is more likely to relax. Especially if the patient is
weak or elderly, it is necessary to pace the examination, pausing at intervals to ask
how he or she is tolerating the assessment.If the patient feels alright, the examination can proceed. However, do not force
the patient to cooperate based on your schedule. Postponing the examination is
advantageous because the findings may be more accurate when the patient can
cooperate and relax.i. Assessment of Age-Groups
It is necessary to use different interview styles and approaches to physical
examination for patients of different age-groups. Your approach will vary with each
group.When assessing children, show sensitivity and anticipate the child’s perception of
the examination as a strange and unfamiliar experience.
When examining children, the following tips help in data collection: Gather all or part of the history on infants and children from parents or
guardians.
Perform the examination in a nonthreatening area; provide time for play to
become acquainted.
Because parents sometimes think the examiner is testing them, offer support
during the examination and do not pass judgment.
Call children by their first name and address the parents as “Mr., Mrs., or
Ms.” rather than by their first name unless instructed differently.
Use open-ended questions to allow parents to share more information and
describe more of the children’s problems. This also allows observation of
parent-child interactions. You can interview older children, who often provide
details about their health history and severity of symptoms.
Treat adolescents as adults and individuals because they tend to respond
best when treated as such.
Remember that adolescents have the right to confidentiality. After talking
with parents about historical information, speak alone with adolescentsii. Cultural Sensitivity
Respect the cultural differences among patients from a variety of backgrounds
when completing an examination.It is important to remember that cultural differences influence patient behaviors.
Consider the patient’s health beliefs, use of alternative therapies, nutrition habits,
relationships with family, and comfort with physical closeness during the examination
and history. These factors will affect your approach as well as the type of findings
you might expect.Be culturally aware and avoid stereotyping on the basis of gender or race. There is
a difference between cultural characteristics and physical characteristics.Learn to recognize common characteristics and disorders among members of
ethnic populations within the community.It is equally important to recognize variations in physical characteristics such as
in the skin and musculoskeletal system, which are related to racial variables. By
recognizing cultural diversity, you show respect for each patient’s uniqueness,
leading to higher-quality care and improved clinical outcomesc) Positioning.
During the examination ask the patient to assume proper positions so body parts are
accessible and he or she stays comfortable. Table 6-4 lists the preferred positions
for each part of the examination and contains figures illustrating the positions.Patients’ abilities to assume positions depend on their physical strength, mobility,
ease of breathing, age, and degree of wellness.After explaining the positions, help the patient to assume them.
Take care to maintain respect and show consideration by adjusting the drapes so
that only the area examined is accessible.During the examination a patient may need to assume more than one position.
N.B. To decrease the number of position changes, organize the examination so all
techniques requiring a sitting position are completed first, followed by those that
require a supine position next, and so forth.Use extra care when positioning older adults with disabilities and limitations.
The table below shows various patients’ positions for physical assessment
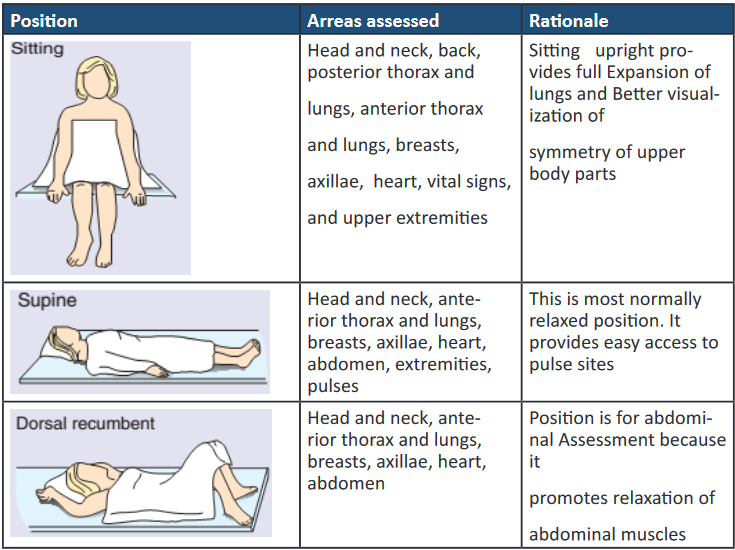
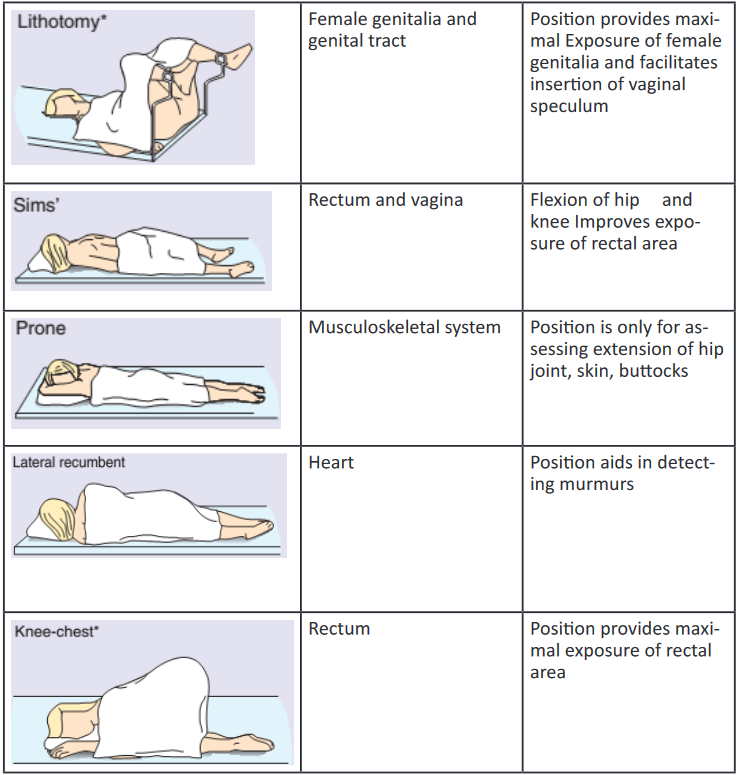
d) Explanation of Different Vital signs and Parameters
i. Vital Signs
After completing the general survey, measure the patient’s vital signs.
Measurement of vital signs is more accurate if completed before beginning positional
changes or movements. If there is a chance that the vital signs are skewed when
first measured, recheck them later during the rest of the examination.Pain, considered the fifth vital sign, should also be assessed.
Begin each head-to-toe shift assessment by assessing the patient’s six vital signs:
Blood pressure, Temperature, Pulse, Respirations, SpO2, and pain level.Because the vital signs serve as important indicators of numerous processes
occurring throughout the body, their assessment serves to establish a basic
foundation of the patient’s condition, possibly alerting you to problems or areas of
concern that you may want to assess in more depth.All six vital signs can also serve as possible indicators of infection, and all but the
SpO 2 and pain may relate to functioning of the immune system.1. Blood Pressure
Blood pressure provides data associated with the cardiovascular system. As we age,
atherosclerosis (hardening of the arteries) increases, contributing to the widening of
the pulse pressure, or the difference between the systolic and diastolic readings.Blood pressure also relates information regarding the kidneys, which excrete renin,
a major component in the control of blood pressure.Blood pressure also provides us with data relating to the level of hydration or fluid
volume within the cardiovascular system.A pulse pressure of 20 mm Hg or less may be indicative of severe dehydration.
In a patient who has fluid overload, blood pressure will be increased.2. Temperature
An elevated temperature can direct your attention to infection or injury to the
hypothalamus, the portion of the central nervous system that helps regulate
body temperature. If the immune system is working correctly, it raises the body
temperature whenever there are signs of microorganism invasion of the body.Hypothermia might indicate exposure to an environment that was too cold or a
disorder of the body’s temperature-regulating mechanisms.In a new-born, hypothermia may identify that the infant is not yet able to regulate
body temperature. It also can be a sign of sepsis or severe hypothyroidism, or it can
be a result of trauma.3. Pulse
Pulse assessment may reveal hypovolemia, due to either dehydration or blood loss.An elevated pulse rate can possibly indicate pain, anxiety, fear, stress, physical
exertion, low blood pressure, infection, effects of medication, and many other
conditions.4. Respirations
Assessment of respirations provides detail about the patient’s respiratory system
as well as the acid-base balance of the blood. The rate and depth of respirations
may provide insight into the patient’s pain intensity and level, anxiety or fear, or
recent exertion.5. Pulse Oxygen Saturation (SpO2)
The patient’s SpO2 level provides further insight as to the state of oxygenation.
6. Pain
Pain assessment includes the site of pain, characteristics of the pain, and strength
of the pain, which can affect assessment of the other vital signs. Include any body
language the patient may exhibit supporting the idea that he or she is in pain, such
as facial grimacing; rubbing, holding, or guarding any particular part of the body
such as the abdomen or head; or any additional verbal sounds such as moaning.
Pain also can direct you to problems in any of the body systems. The intensity and
characteristics of pain can relate the severity of illness or injury and also detail the
effectiveness of pain medication.Pain is normally assessed using a pain scale of 0 to 10 (or other facility-approved
scale) for adults and a scale using a series of facial expressions for children.Pain Scale
Use a pain scale, such as a scale of 0 to 10, with 0 being “no pain” and 10 being
“worst pain you can imagine,” when assessing the patient’s pain. Because pain is a
subjective matter for the patient, use of the numerical scale allows for introduction
of a certain amount of objectivity.For young children or patients with impaired cognition, you probably will use the
Wong-Baker FACES Pain Rating Scale, which consists of a picture of a series
of faces that show varying degrees of comfort, from smiling, to frowning, to crying.The child can point to the picture that matches his or her pain level
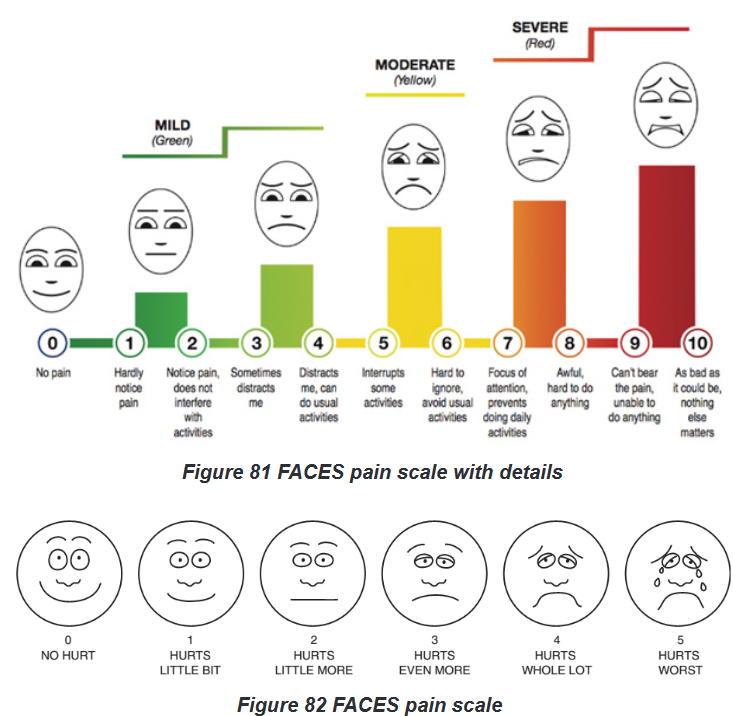
Explain to the person that each face is for a person who feels happy because he
has no pain (hurt) or sad because he has some or a lot of pain. Face 0 is very happy
because he doesn’t hurt at all. Face 1 hurts just a little bit. Face 2 hurts a little more.
Face 3 hurts even more. Face 4 hurts a whole lot. Face 5 hurts as much as you
can imagine, although you don’t have to be crying to feel this bad. Ask the person
to choose the face that best describes how he is feeling.Rating scale is recommended for persons age 3 years and older.
Brief word instructions: Point to each face using the words to describe the pain
intensity. Ask the child to choose the face that best describes own pain and record
the appropriate number Pain intensity or rating scales.
The single most important indicator of the existence and intensity of pain is the
person’s report of pain. In practice, however, D’Arcy (2011) found that nurses tend
to use less reliable measures for assessing pain. The top factors identified by nurses
were culturally influenced (e.g. facial expressions, verbalization, request for relief).
The use of pain intensity scales is an easy and reliable method of determining the
person’s pain intensity. Such scales provide consistency for nurses to communicate
with the person and other health care providers.To avoid confusion, scales should use a 0 to 10 range with 0 indicating ‘no pain’
and the highest number indicating the ‘worst pain possible’ for that individual.The inclusion of word modifiers on the scale can assist some people who find it
difficult to apply a number level to their pain. For example, after ruling out ‘0’ and
‘10’ (neither no pain nor the worst possible pain), a nurse can ask the person if : it
is mild (2), mild to moderate (4),moderate to severe (6), or severe (8).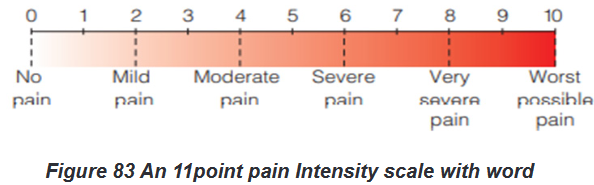
Another way to evaluate the intensity of pain for people who are unable to use the
numerical rating scales is to determine the extent of pain awareness and degree of
interference with functioning.
For example,
0 5 no pain,
2 5 awareness of pain only when paying attention to it,
4 5 can ignore pain and do things,
6 5 can’t ignore pain, interferes with functioning,
8 5 impairs ability to function or concentrate, and
10 5 intense incapacitating pain.
It is believed that the degree that pain interferes with functioning is a good marker
for the severity of pain, especially for those with chronic pain.After pain medication has been given, it is important to reassess the patient’s
pain using the same pain scale used before treatment of the pain so that you can
objectively determine whether or not the medication was effective.This is part of the evaluation phase of the nursing process.
7. Height and Weight
Height and weight reflect a person’s general health status. Assess every patient to
identify if he or she is at a healthy weight, overweight, or obese. Weight is routinely
measured during health screenings, visits to physicians’ offices or clinics, and on
admission to the hospital.Infants and children are measured for both height and weight at each health care
visit to assess for healthy growth and development. If older adults are underweight,
difficulty with feeding and other functional activities is a possibility.A patient’s weight normally varies daily because of fluid loss or retention. Ask the
patient to report current height and weight, along with a history of any substantial
weight gain or loss. A weight gain of 5 pounds (2.3 kg) in 1 day indicates fluid-
retention problems.A weight loss is considered significant if the patient has lost more than 5% of body
weight in a month or 10% in 6 months.When a patient is hospitalized, daily weight is measured at the same time of day,
on the same scale, with approximately the same clothes. This allows an objective
comparison of subsequent weights.Accuracy of weight measurement is important because health care providers base
medical and nursing decisions (e.g., drug dosage, medications) on changes.Several different scales are available for use. Patients capable of bearing their own
weight use a standing scale.The standard platform scale is calibrated by moving the large and small weights to
zero. Electronic scales automatically display the weight within seconds. They are
calibrated automatically each time they are usedSelf-assessment 6.4.
1) Define the following terms associated with physical assessment:
a) Physical assessment
b) Symptoms
c) Signs
2) Describe five purposes of physical assessment.
3) Name the various vital signs and parameters to be assessed during the
physical examination
4) Explain the action to be taken by a nurse during the physical examination
after considering the patient’s current condition and give an example.6.5. Techniques of physical assessment
Learning activity 6.5.
For Overview of Physical Assessment techniques
Use also the provided textbooks of Fundamentals of Nursing to read information
about Techniques of Physical Assessment and make a summary note of the
following:
1) Definition of each technique of Physical Assessment
2) Describe the techniques used with each physical assessment skill.
The summary will be presented to the class for discussion and clarificationFor Physical Assessment techniques
Images about conducting the techniques of Physical Assessment;
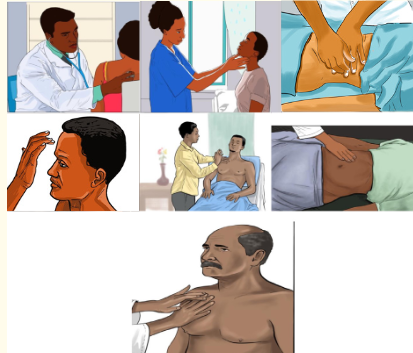
After observing the above images under section (b) for your guidance and after
carefully reading the guidelines provided to be followed under each technique
used in Physical Examination, each learner should demonstrate the techniques
used in physical assessment skill as follows:
1) Form pairs of 2 students and each one will conduct each technique used
during physical assessment namely: Inspection, Palpation, Percussion
and Auscultation.
2) Write down findings for your partner; Interpret results showing normal
and abnormal findings.The four techniques used in a physical examination are inspection, palpation,
percussion, and auscultation.5.6.1. Inspection
Inspection is the visual examination or assessment using the sense of sight.An initial visual assessment should be part of the procedure of greeting the person,
in which such aspects as the person’s overall demeanor and appearance, hygiene,
skin colour and skin appearance can be noted.Nurses frequently use visual inspection to assess: moisture, colour and texture of
body surfaces, as well as shape, position,size and symmetry of the body.Lighting must be sufficient for the nurse to see clearly and may be either natural or
artificial light.When using the auditory senses, it is important to have a quiet environment to
enable accurate hearing. Observation can be combined with the other assessment
techniques.To inspect, carefully look, listen, and smell to distinguish normal from abnormal
findings. To do so, you must be aware of any personal visual, hearing, or olfactory
deficits. It is important to deliberately practice this skill and learn to recognize all of
the possible pieces of data that can be gathered through inspection alone.Inspection occurs when interacting with a patient, watching for nonverbal
expressions of emotional and mental status. Physical movements and structural
components can also be identified in such an informal way. Most important, be
deliberate and pay attention to detail.Follow these guidelines to achieve the best results during inspection:
Make sure that adequate lighting is available, either direct or tangential.
Use a direct lighting source (e.g., a penlight or lamp) to inspect body cavities.
Inspect each area for size, shape, color, symmetry, position, and abnormality.
Position and expose body parts as needed so all surfaces can be viewed
but privacy can be maintained.
When possible, check for side-to-side symmetry by comparing each area
with its match on the opposite side of the body.
Validate findings with the patient. While assessing a patient, recognize
the nature and source of body odors. An unusual odor often indicates an
underlying pathology. Olfaction helps to detect abnormalities that cannot be
recognized by any other means. For example, when a patient’s breath has a
sweet, fruity odor, assess for signs of diabetes. Continue to inspect various
parts of the body during the physical examination.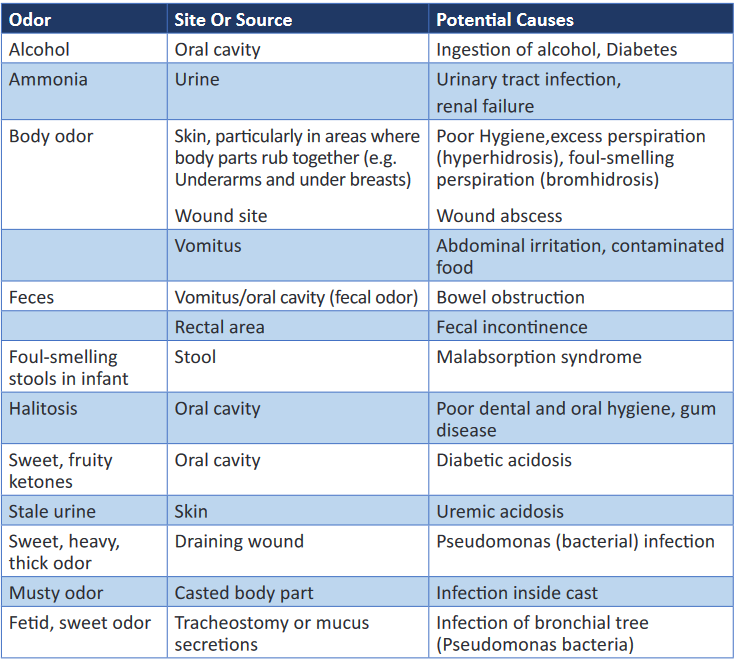
Palpation may be used concurrently with inspection, or it may follow in a more
deliberate fashion.6.5.2. Palpation
Palpation is the examination of the body using the sense of touch to gather
information.The pads of the fingers are used because their concentration of nerve endings
makes them highly sensitive to tactile discrimination.There are two types of palpation: light and deep.
Through touch you make judgments about expected and unexpected findings of
the skin or underlying tissue, muscle, and bones.Palpation is used to determine: texture (e.g. of the hair); temperature (e.g. of a skin
area); vibration (e.g. of a joint); position, size, consistency and mobility of organs
or masses; distention (e.g. of the urinary bladder); pulsation; and tenderness or
pain.General guidelines for palpation
General guidelines for palpation include the following:
The nurse’s hands should be clean and warm, and the fingernails short.
Areas of tenderness should be palpated last.
Deep palpation should be done after light palpation (see below).Light (superficial) palpation should always precede deep palpation because
heavy pressure on the fingertips can dull the sense of touch.
For light palpation, the nurse extends the dominant hand’s fingers parallel
to the skin surface and presses gently downward while moving the hand in
a circular motion.
With light palpation, the skin is slightly depressed.
If it is necessary to determine the details of a mass, the nurse presses lightly
several times rather than holding the pressure.Deep palpation is done with two hands (bimanually) or one hand.
In deep bimanual palpation, the dominant hand is extended (for light
palpation), then the finger pads of the non-dominant hand are placed on the
dorsal surface of the distal interphalangeal joint of the middle three fingers
of the dominant hand of deep bimanual palpation). The non-dominant hand applies pressure while the lower hand remains
relaxed to perceive the tactile sensations.
For deep palpation using one hand, the finger pads of the dominant hand
press over the area to be palpated. Often the other hand is used to support
a mass or organ from below
Deep palpation is usually not done during a routine examination and requires
significant practitioner skill. It is performed with extreme caution by doctors
because pressure can damage internal organs. It is usually not indicated in
people who have acute abdominal pain or enlarged abdominal organs and
where the source of pain is yet to be diagnosed.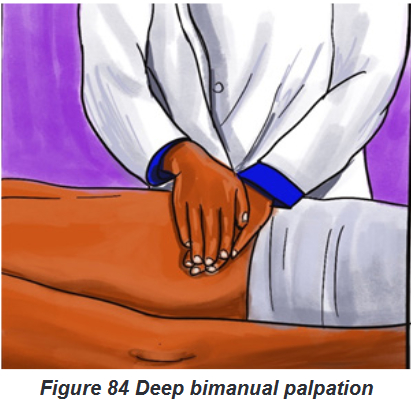
The palmar surface of the hand and finger pads is more sensitive than the fingertips
and should be used to determine position, texture, size, consistency, masses, fluid,
and crepitus.Assess body temperature by using the dorsal surface or back of the hand.
The palmar surface of the hand and fingers is more sensitive to vibration.
Measure position, consistency, and turgor by lightly grasping the body part with the
fingertips.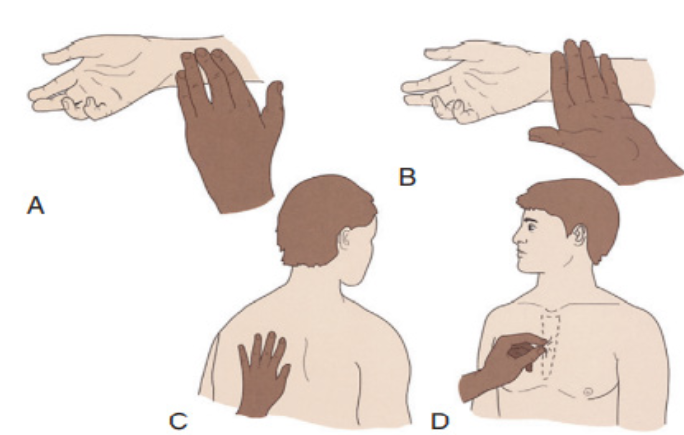
Figure 85 A, Radial pulse is detected with the pads of fingertips, the most
sensitive part of the hand. B, Dorsum of the hand detects temperature
variations in skin. C, The bony part of the palm at the base of the fingers
detects vibrations. D, Skin is grasped with the fingers to assess the turgor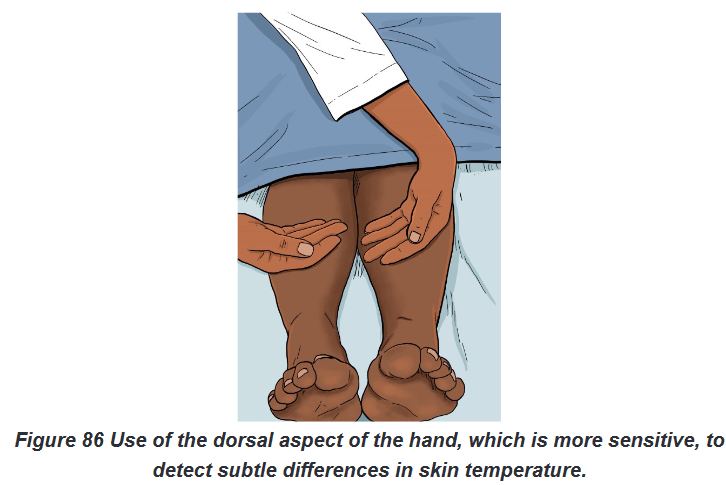
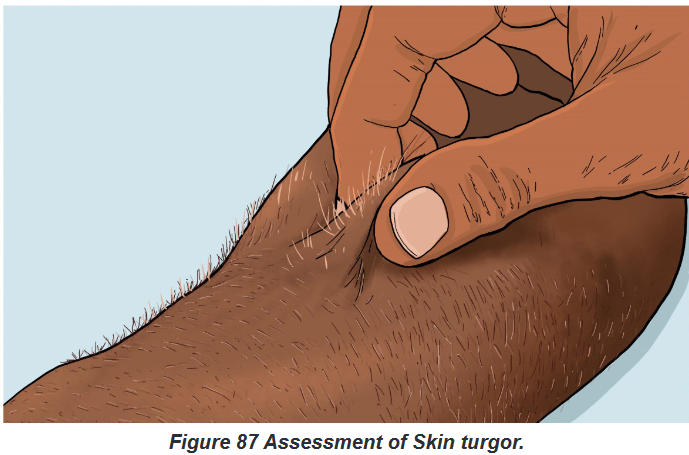
General considerations:
Touching the patient is a personal experience for both you and the patient.
Display respect and concern throughout the examination.
Before palpating consider the patient’s condition and ability to tolerate the
assessment techniques, paying close attention to areas that are painful or tender.In addition, always be conscious of the environment and any threats to the patient’s
safety.Prepare for palpation by warming hands, keeping fingernails short and using a
gentle approach.Palpation proceeds slowly, gently, and deliberately.
The patient needs to be guided to relax and feel comfortable since tensed muscles
make assessment more difficult. To promote relaxation, have him or her take slow,
deep breaths and place both arms along the sides of the body.Ask the patient to point to more sensitive areas, watching for nonverbal signs of
discomfort.Palpate tender areas last one hand (sensing hand) and place it lightly over the
patient’s skin. The other hand (active hand) helps apply pressure to the sensing
hand.The lower hand does not exert pressure directly and thus remains sensitive to
detect organ characteristics.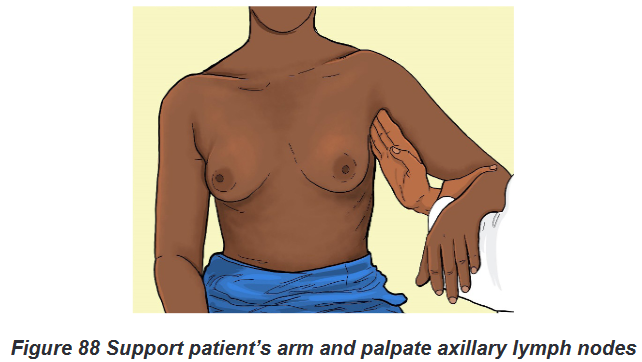
For safety deep palpation should be observed by your clinical instructor when you
first attempt the procedure.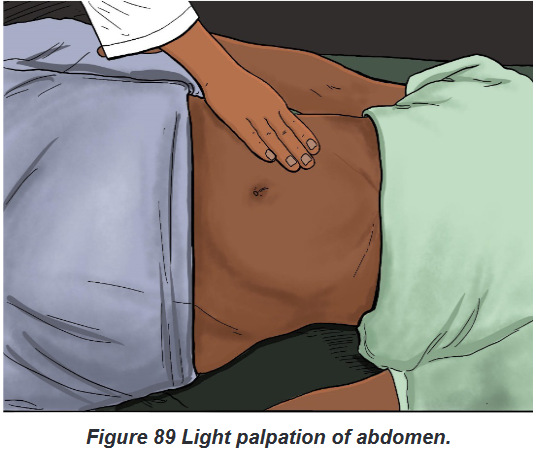
6.5.3. Percussion
Percussion is the act of striking the body surface to elicit sounds that can be heard
or vibrations that can be felt.Percussion involves tapping the skin with the fingertips to vibrate underlying tissues
and organs.The vibration travels through body tissues, and the character of the resulting sound
reflects the density of the underlying tissue.The denser the tissue, the quieter the sound. By knowing how various densities
influence sound, it is possible to locate organs or masses, map their edges, and
determine their size.An abnormal sound suggests a mass or substance such as air or fluid within an
organ or body cavity.The skill of percussion is used more often by advanced practice nurses than by
nurses in daily practice at the bedside.There are two types of percussion: direct and indirect.
a) Direct technique of percussion Procedural guideline
Direct percussion:
The nurse strikes the area to be percussed directly with the pads of two,
three or four fingers, or with the pad of the middle finger.
The strikes are rapid and the movement is from the wrist (see Figure 31.4).
This technique is not generally used to percuss the thorax but is useful in
percussing an adult’s sinuses.The most commonly used percussion technique is the indirect technique.
b) Indirect technique of percussion Procedural guidelines:
Indirect percussion is the striking of an object (e.g. a finger) held against the body
area to be examined.
You perform the indirect technique by placing the middle finger of your
nondominant hand referred to as the pleximeter, , firmly on the person’s
skin against the body surface.With palm and fingers remaining off the skin, the tip of the middle finger of the
dominant handcalled the plexor, strikes the base of the distal joint of the finger.Use a quick, sharp stroke, keeping the forearm stationary.
Relax the wrist to deliver the proper blow. Once the finger has struck, the
wrist snaps back.
The motion comes from the wrist; the forearm remains stationary.
The angle between the plexor and the pleximeter should be 90 degrees and
the blows must be firm, rapid and short to obtain a clear sound.If the blow is not sharp, if the hand is held loosely, or if the palm rests on the body
surface, the sound is softened; and you will not detect the presence of underlying
structures.A light, quick blow produces the clearest sounds.
Percussion elicits or produces five types of sound: flatness, dullness, resonance,
hyper resonance and tympany:
1. Flatness is an extremely dull sound produced by very dense tissue, such as
muscle or bone.
2. Dullness is a thud-like sound produced by dense tissue such as the liver, spleen
or heart.
3. Resonance is a hollow sound such as that produced by lungs filled with air
4. Hyperresonance is not produced in the normal body. It is described as booming
and can be heard over an emphysematous lung.
5. Tympany is a musical or drum-like sound produced from an air-filled stomach.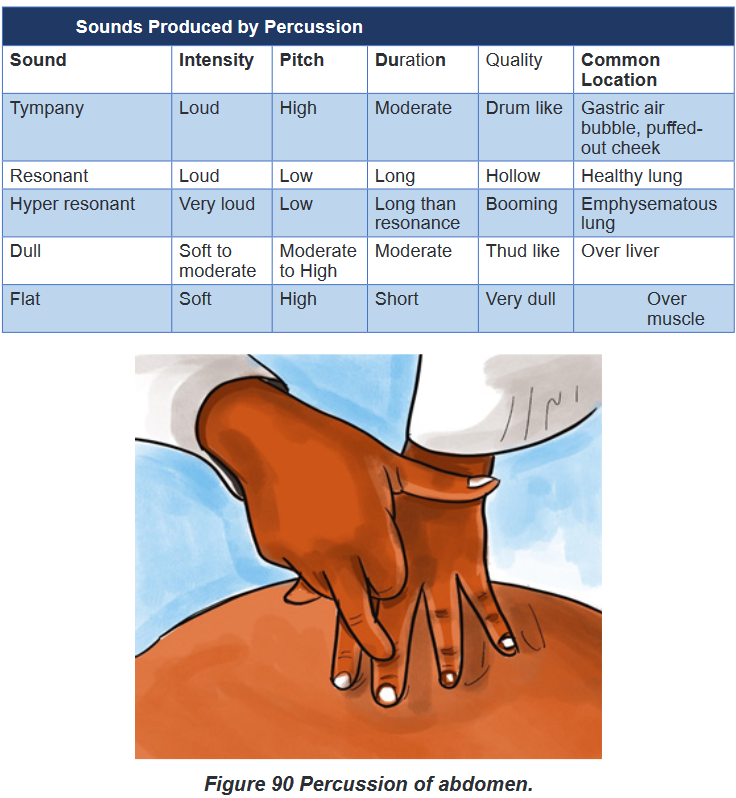
6.5.4. Auscultation
Auscultation is the process of listening to sounds produced within the body in
order to detect variations from normal.Auscultation may be direct or indirect: Direct auscultation is the use of the unaided
ear; for example, to listen to a respiratory wheeze or the grating of a moving joint
whereas Indirect auscultation is the use of a stethoscope, which transmits the
sounds to the assessor’s ears.A stethoscope is used primarily to listen to sounds from within the body, such as
bowel sounds or valve sounds of the heart and blood pressure. In other words, a
stethoscope is necessary to hear internal body sounds.Internal body sounds are created by blood, air, or gastric contents as they move
against the body structures. For example, normal heart sounds are created when
the heart valves close, moving blood to the next portion of the cardiovascular
system. Learn to recognize abnormal sounds after learning normal variations.Becoming more proficient in auscultation occurs by knowing the types of sounds
each body structure makes and the location in which the sounds are heard best.To auscultate internal sounds, you need to hear well, have a good stethoscope, and
know how to use it properly. Nurses with hearing disorders can obtain stethoscopes
with extra sound amplification.The bell is best for hearing low-pitched sounds such
as vascular and certain heart sounds, and the diaphragm is best for listening to
high-pitched sounds such as bowel and lung sounds.By practicing with the stethoscope, you become proficient at using it and realize
when sounds are clear and when there are extraneous sounds. Extraneous sounds
created by rubbing against the tubing or chest piece interfere with auscultation of
body organ sounds. By deliberately producing these sounds, you learn to recognize
and disregard them during the actual examination.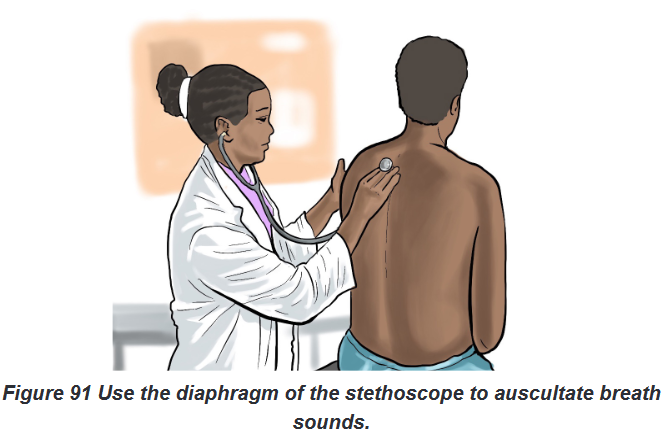
Auscultated sounds are described according to their pitch, intensity, duration and
quality:
The pitch which is the frequency of the vibrations; indicates the number of
sound wave cycles generated per second by a vibrating object. The higher
the frequency, the higher the pitch of a sound and vice versa. Low-pitched
sounds, such as some heart sounds, have fewer vibrations per second than
high-pitched sounds, such as bronchial sounds. Loudness (Intensity)refers to the amplitude of a sound wave. Auscultated
sounds range from soft to loud. Quality refers to sounds of similar frequency and loudness from different
sources. The quality of sound is a subjective description of a sound; for
example, whistling, blowing, gurgling or snapping. Duration means the length of time that sound vibrations last (long or short).
The duration of sound is short, medium, or long. Layers of soft tissue dampen the
duration of sounds from deep internal organs.Auscultation requires concentration and practice: while listening, know which
sounds are normally produced in certain parts of the body and what causes the
sounds.After understanding the cause and character of normal auscultated sounds, it
becomes easier to recognize abnormal sounds and their originsSelf-assessment 6.5.
For (a) section: Techniques of Physical Assessment Overview;
1) Define the four methods/ techniques used for physical assessment
2) List and explain the five types of sounds produced by Percussion
3) What are the conditions to be fulfilled in order to auscultate internal
sounds?
4) Why Light or Superficial palpation should always precede deep
palpation?
5) Provide the contra-indication of Deep Palpation.
6) Explain the four Characteristics according to which Auscultated Sounds
are described.
For (b) section: Procedure of conducting out the techniques of Physical
Assessment;
Learners will practice in skills lab under guidance of the facilitator.
Images /videos if possible and Guidelines will be provided.
After observing the above images under section (b) for your guidance and after
carefully reading the guidelines provided to be followed under each technique
used in Physical Examination; each learner should demonstrate the techniques
used in physical
assessment as follows:
1) Form pairs of 2 students and each one will conduct each technique used
during physical assessment namely: Inspection, Palpation, Percussion
and Auscultation.
2) Write down findings for your partner, interpret results showing normal
and abnormal findings.End unit assessment 6
1) The patient health history and physical examination provide the
nurse with information to primarily
a) Diagnose a medical problem.
b) Investigate a patient’s signs and symptoms.
c) Classify subjective and objective patient data.
d) Identify nursing diagnoses and collaborative problems2) The nurse is preparing to examine a patient’s abdomen. Identify the
proper order of the steps in the assessment of the abdomen, using the
numbers 1-4 with 1 =the first technique and 4 =the last technique:
(1) Inspection
(2) Palpation
(3) Percussion
(4) Auscultation3) The nurse is performing an admission assessment. Which of the following
are examples of objective data? Select all that apply.
a) 10 cc of emesis in basin
b) Cool, clammy skin
c) Client says, ‘‘My feet are swollen.’’
d) Complaint of nausea by client
e) Oral temperature 1030F
f) Rapid, thready pulse4) When performing an assessment, which of the following would the nurse
use as a primary source of data?
a) All health care personnel
b) Client
c) Client family and/or friends
d) Client medical records5) During interview, a nurse asks this question to the client “Do you
have a family history of psychiatric illness?” In which domain of the
biopsychosocial model this question belongs?
a) Biology domain
b) Psychology domain
c) Social domain
d) Psychosocial domain6) What is the purpose of health history?
7) Put “Words” under figures or numbers for each Pain scale as far as pain
assessment is concerned: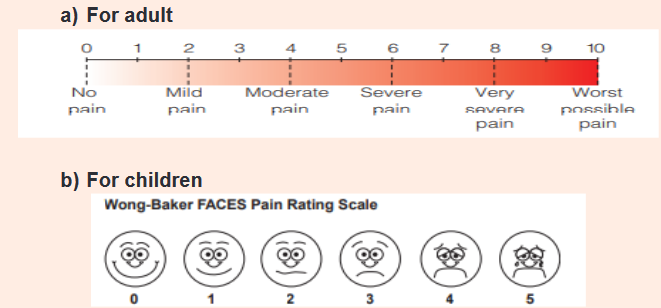
8) List the elements assessed frequently by Nurses using Visual Inspection.
9) What is the difference between Direct auscultation and Indirect
Auscultation?
10) Match the Characteristics odors in column (A) to Potential causes in
column (B)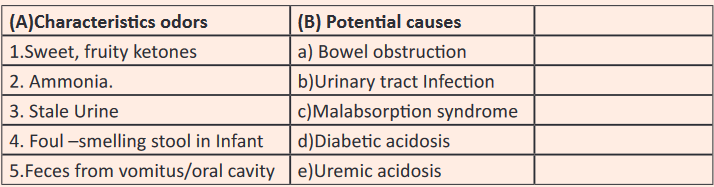
UNIT 7: NURSING ASSESSMENT OF RESPIRATORY SYSTEM
Key unit competence:
Take appropriate action based on findings of nursing assessment of respiratory
systemIntroductory activity 7
Observe the image below and respond to the asked questions
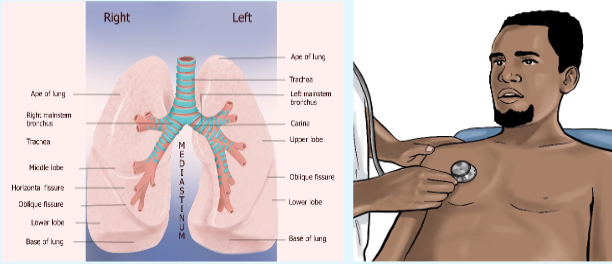
1) Identify the procedure that is being performed on picture B?
2) List the lung’s anatomy parts shown by allow on picture A on right and
left side?7.1. History taking on respiratory assessment
Learning activity 7.1.

1) Outline the types of information needed during history taking on
respiratory system?
2) State some of the 5 key questions asked by health care providers during
history taking on respiratory system?7.1.1. Respiratory history taking overview
Among the assessment techniques essential to valid diagnosis, performing a fact
finding history is key. To obtain adequate history, providers must be well organized
attentive to the patient’s verbal and nonverbal language and able to accurately
interpret the patent’s responses to questions. The history like the physical
examination is informed by the knowledge of a wide range of conditions, their
physiological basis and their associated signs and symptoms.A comprehensive nursing assessment includes an assessment of each system. In
this lesson, we are going to focus on the respiratory system. Regardless of the chief
complaint, a thorough symptom analysis is warranted.It is important to get an understanding of when the complaint started and how the
onset occurred, determine how it has evolved, starting with the initial episode or
awareness of the problem. Ask whether the problem is constant or intermittent.Determine whether a similar problem has been experienced in the past. It is
important to learn whether anything in particular, such as emotions, exposure to
outdoor allergens, or fatigue, tends to precipitate or accelerate the complaint. Also
determine whether the symptoms tend to be tied to any particular time of day, such
as night, early morning, or immediately following a meal.Another timing-related issue involves whether the complaint has continued
essentially unchanged, worsened, or improved since first noticed.The quality of the symptom is important
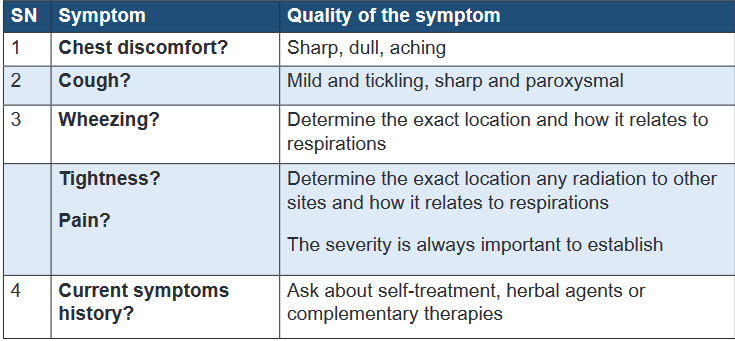
7.1.2. Pulmonary review of symptoms
a) Shortness of breath
If the patient experiences shortness of breath, record the amount of work or effort
that causes this symptom. Ask about nocturnal orthopnea or related difficulty
sleeping. Specifically, ask about the number of pillows the patient uses to sleep
and about the sleeping position. A patient may use no pillows and rest comfortably
only in a recliner.Determine whether the patient has had a cough and whether any cough has been
associated with the production of sputum or with hemoptysis.Also ask about wheezing, chest tightness, and sense of congestion. Ask whether
the patient has had a fever, chills, or night sweats. In addition to asking about
symptoms related to the lower respiratory tract, other systems should be explored
on the basis of the presenting symptom and symptom analysis.b) Dyspnea
The subjective sensation of difficulty in breathing is probably the most common
respiratory complaint and cannot be differentiated at first glance from dyspnea due
to cardiac disease, neuromuscular weakness, or simple obesity.Some questions can be asked to explore the origin of dyspnea;
Is the breathlessness recent or has it been present for sometimes?
Is it constant or does it comes and goes?
What can’t you do because of the breathlessness?
What makes the breathing worse?
Does anything make it better?
Duration?c) Cough
Cough is a normal defense mechanism of the respiratory tract, but when increased
in severity or frequency, cough can be a cause of disease as well as an indicator
of disease.The etiologies of cough can be:
Inflammatory: edema and hyperemia of airways and alveoli due to laryngitis,
tracheitis, bronchitis, bronchiolitis, pneumonitis, and lung abscess. Mechanical: inhalation of particulates (dust) or compression of airways
(pulmonary neoplasms, foreign bodies, granulomas, bronchospasm).
Chemical: inhalation of irritant fumes, including cigarette smoke Thermal:
inhalation of cold or very hot air.The assessment of a cough implies also the duration. The patient will be asked for
how long has he/she been coughing. When the cough has been there for days to
weeks; it is a sub acute cough. If the cough has been there for months to years; it
is a chronic cough.d) Sputum/ Expectoration
Sputum production reflects an image the presence of inflammatory, infectious or
neoplastic disease in the airways or pulmonary parenchyma. The amount and
character of sputum provide the health care provider with helpful clues to distinguish
among possible etiologies. The color can be mucoid, purulent, mucopurulent or
bloody. Also assess the duration and presence of fever or wheezing.e) Hemoptysis
Hemoptysis is the coughing up of blood from the lungs. Before using the term
“hemoptysis,” the source of bleeding should be confirmed by both history and
physical examination. Blood or blood-streaked material may originate from the
mouth, pharynx, or gastrointestinal tract and can easily mislabel. The color of the
blood is also implied; blood originating from the stomach is usually darker than blood
from the respiratory tract and may be mixed with food particles. When it is originating
from the gastric tract, it is called “hematemesis”. For patients reporting hemoptysis,
the volume of blood produced is also assessed. Hemoptysis is confirmed by the
presence of Cough, Sputum, Alcalin PH, and Alveolar macrophage.f) Wheezes
Wheezes are sounds that are heard continuously during inspiration or expiration,
or during both inspiration and expiration .They are most commonly heard at end
inspiration or early expiration. Wheezes are caused by air moving through airways
narrowed by constriction or swelling of airway or partial airway obstruction. Wheezes
can be classified as either high pitched or low pitched wheezes. It is often inferred
that high pitch wheezes are associated with disease of the small airways and low
pitch wheezes are associated with disease of larger airways.g) Chest pain
The source of chest pain can be due to parietal pleura, chest wall, diaphragm, or
mediastinal involvement, it can be pleuritic (sharp knife-like), it can also originate
from myocardium (angor pectoris, myocardial infarction), from pericardium
(pericaditis), from aorta (dissecting aortic, aneurism) or from trachea and large
bronchi (tracheitis, bronchitis). The following questions have to be asked while
assessing pain; where?, how long?, kind, radiation.h) Clubbing
Fingers extremities change in coloration due to their poor oxygenation. Clubbing
can be caused by lung abscess, chronic cavity due to mycobacterial or fungal
infection in lungs, clubbing may also be caused by cardiovascular diseases, or
metabolic diseases.Self-assessment 7.1.
1) In case the client consults the health care provider for respiratory
problems, the health care provider should determine whether a similar
problem has been experienced in the past and rule out the factors
influencing respiratory system disorders. The one among the following
factors has no influence on respiratory problems:
a) Emotions,
b) Fatigue,
c) The number of deliveries for a woman,
d) Exposure to outdoor allergens.2) If the patient experiences shortness of breath, record the amount of
work or effort that cause this symptom and ask about:
a) The sleeping position,
b) Nocturnal orthopnea or difficulty sleeping,
c) The number of pillows the patient uses to sleep,
d) All the above3) The coughing up of blood from the lungs is the symptom reported often
by patients. The source of bleeding should be confirmed by both history
and physical examination. This symptom is called:
a) Hematemesis
b) Hemoptysis
c) Expectorant
d) Soft vomiting4) The quality of the symptom is important if a patient complains about “pain”
during history taking of respiratory system conditions, the nurse should ask
whether the pain is:
a) Mild and tickling, sharp and paroxysmal
b) Sharp, dull, aching
c) In inspiration or expiration
d) Radiating to other sites and how it relates to respirations7.2. Physical examination of respiratory system: A/
General examinationLearning activity 7.2.
Analyze carefully the following images and respond to the questions below;
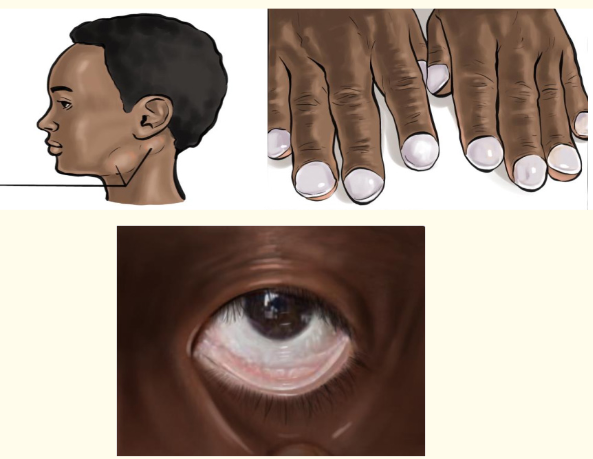
1) List the two (2) physical signs shown on above image which may indicate
poor oxygen in body?
2) Describe two signs of poor tissue oxygenation observed in nails?
3) Explain what does lymph nodes enlargement indicate in respiratory
assessment?
4) Which posture is to be observed to assess if the patient has respiratory
distress?Fundamental of Nursing | Associate Nursing Program | Senior 4 335
Initial survey is the first step to be performed by health care provider to evaluate the
level of consciousness if the patient is alert, cooperative, and normally oriented
because patients with hypoxemia may be irritable, somnolent, restless, confused,
or combative.The close assessment of the position for breathing is necessary whether the posture
is relaxed or upright because the patients in respiratory distress may lean forward
in “tripod position” a position whereby one sits or stands learning forward and
supporting the upper body with hands on knees or on another surface.
The other observation will focus on patient’s lips and nasal flaring including facial
expression as patient in respiratory distress may look anxious or show nasal flaring
and those with chronic obstructed pulmonary diseases show pursed lips; the
observation and documentation of skin color for cyanosis and pallor is also a key.
Skin color is appropriate tone for race. Cyanosis is a bluish color to the skin or
mucous membrane and is usually due to a lack of oxygen in the blood while pallor
is a condition in which a person’s skin and mucous membranes turn lighter in pale
color than they usually are secondary to respiratory distress it is often observed in
palms and nails.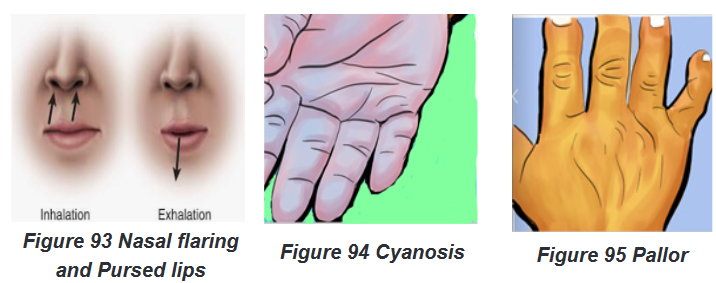
The nurse observes respiratory movements and note if the patient uses the upper
or lower chest to breathe because patients with disease that impedes outflow may
have forced expiration. Guarding may accompany respiratory pain. The observation
of respiratory movements may be accompanied by counting rate.Respiratory rate is 12 to 20 breaths per minute for adults with regular rhythm.
Tachypnea is greater than 24 breaths per minute; bradypnea is less than 10
breaths per minute. An infant’s breathing rate may reach 40 breaths per minute.
The respiratory pattern should be even, coordinated, and regular, with occasional
sighs (long, deep breaths).Assess muscles used for breathing. Diaphragm and external intercostals do most
of the work. Intercostals retractions are due to reduced air pressure inside the
chest; this can happen if the upper airway or small airways of the lungs become
partially blocked. Patients with respiratory distress may use accessory muscles.
Retractions accompany resistance to airflow (eg, in severe asthma)Observe fingers for clubbing, clubbing is a physical sign characterized by bulbous
enlargement of the ends of one or more fingers or toes due to proliferation and
edema of connective tissue result in loss of the normal angle between the skin and
nail plate and excessive sponginess of the nail base. Clubbing is noted with chronic
lung disease.The observation of lymph node enlargement is important as the most common
cause of lymph node swelling in the neck is an upper respiratory infection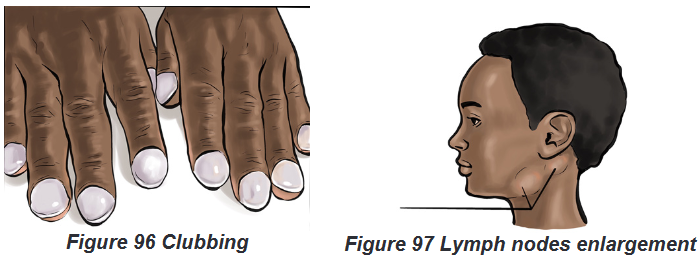
Self-assessment 7.2.
1) Recall the two observations to be noted by a health care provider related
to respiratory movements?
2) Explain intercostals retraction sign and give an example of respiratory
disease in which this sign may occur?
3) Express the importance to evaluating the level of consciousness in
respiratory assessment.
4) Recall two signs assessed on patient’s lips and nose to diagnose
respiratory problems?7.3. Physical examination of respiratory system: A/
Focused examinationLearning activity 7.3.
The images below illustrate the focused respiratory physical exam
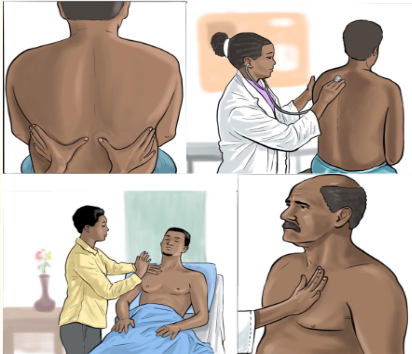
1) Describe the similarities and differences observed in images of
respiratory focused examination?The focused physical examination is helpful to examine the posterior thorax and
lungs while the patient is sitting, the anterior thorax and lungs while the patient is
supine. The process is performed in four ordered phases or techniques: inspection,
palpation, percussion and auscultation.7.3.1. Inspection
This phase/technique of inspection requires the use of the naked eye of health care
provider to observe the face for nasal flaring, pursed lips breathing, conjunctiva for
pallor and facial skin for central cyanosis. Observe neck and trachea for jugular
vein and neck veins pulsation in bronchial asthma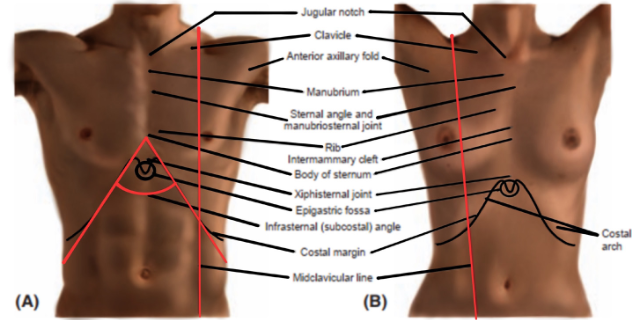
Note thoracic shape and configuration (horizontal ribs, barrel chest, kyphosis,
funnel chest), observe spontaneous chest expansion, scapulae are symmetric.
Chest wall is cone shaped, symmetric and oval. Accessory muscle use is to be
noted and hands inspection for Clubbing (base angle of nail obliterated, increased
sponginess of nail bed) and peripheral cyanosis: excessive O2 extraction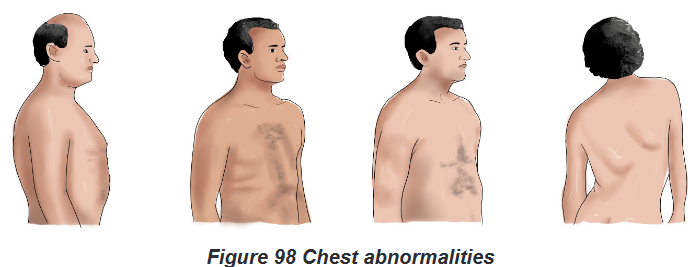
7.3.2. Palpation
Palpation technique consists of using fingertips above the scapula over the lung
apex. Move from one side to another; compare bilateral findings. End at lung base;
move laterally to midaxillary line.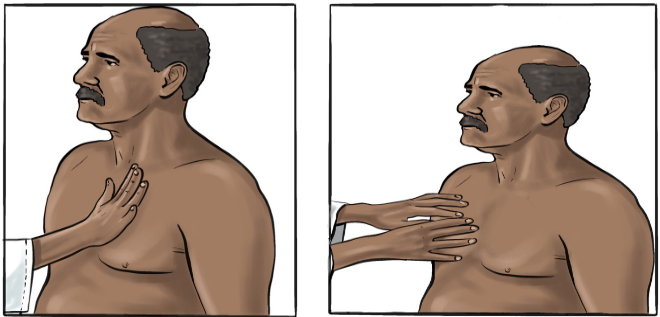
Place your palm (or palms) lightly over the thorax. Palpate for tenderness, alignment,
bulging, and retractions of the chest and intercostal spaces, lumps, masses. Assess
the patient for crepitus, especially around drainage sites. Repeat this procedure on
the patient’s back. Palpation helps to examine the thoracic wall defects like pain
press and swelling and vibration sounds (tactile fremitus).Use the pads of your
fingers to palpate the front and back of the thorax. Pass your fingers over the ribs
and any scars, lumps, lesions, or ulcerations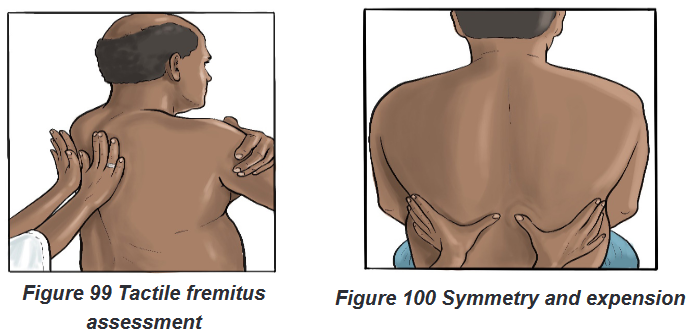
7.3.3. Percussion
Percussion is a method of tapping on a surface to determine the underlying
structure, and is used in clinical examinations to assess the condition of the thorax;
percussion is used when lung obstruction or consolidation is suspected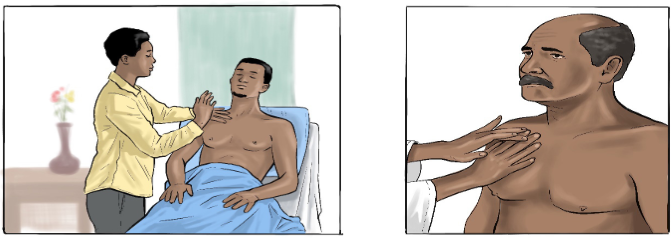
The examiner begins at the apex of the lungs. Percuss from one side to another.
Work toward the bases in the intercostal spaces. Move fingers approximately 5 cm
apart. When fingers are below the level of lung tissue, sound changes from resonant
to dull; from around T10 move laterally to percuss near the anterior axillary line and
7th and 8th Intercostals. Avoid the area over the ribs and scapulae, because normal
bone is flat.Healthy lung tissue sounds resonant.
Place your non dominant hand over the chest wall, pressing firmly with your
middle finger.
Position your dominant hand over your other hand.
Flex the wrist (not the elbow or upper arm) of your dominant hand; tap
the middle finger of your non-dominant hand with the middle finger of your
dominant hand.
Follow the standard percussion sequence over the front and back chest
walls.7.3.4. Auscultation
Auscultation is performed for the purposes of examining the respiratory system for
breath sounds. Listen from top to down alternating left and right. Ensure that the
stethoscope is in direct contact with the skin.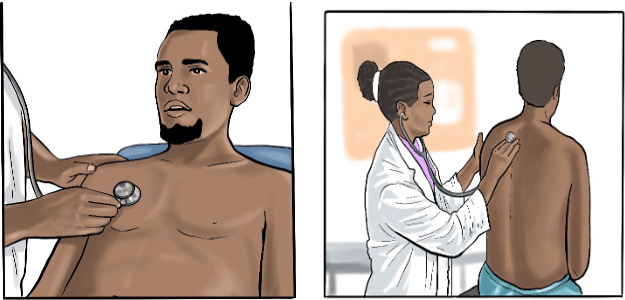
Listen for extra, abnormal sounds of breathing. Ask the patient to breathe through
the mouth. Place the flat side of the diaphragm on the chest wall firmly to block
extraneous noise. Listen to one full breath in each location. Move from one side to
another. Stand behind and beside the patient. Listen from lung apices to bases and
then laterally in the same sequence as percussion. If sounds are too soft, ask the
patient to breathe deeper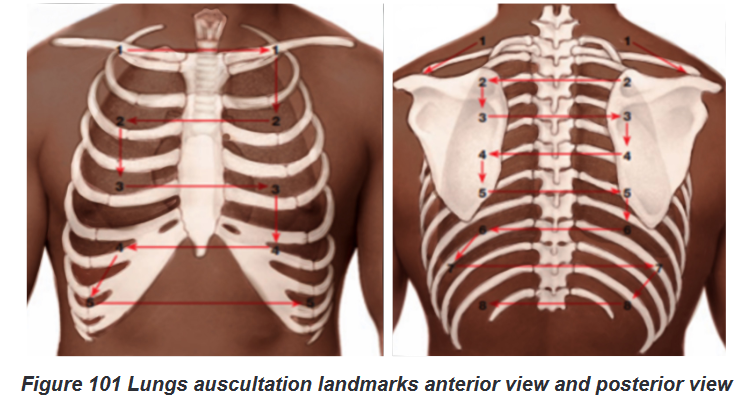
Identify vesicular, broncho vesicular, and bronchial breath sounds. Listen for
intensity of sounds, quality, pitch, and duration of inspiration versus expiration.
Normal breath sounds are vesicular. Expiration is longer than inspiration, similar
to normal breathing. Note the absence of adventitious sounds when documentingSelf-assessment 7.3.
1) List the four phases/techniques of respiratory physical examination?
2) Outline the elements of inspection in respiratory physical examination?
3) Describe the difference between percussion and palpation techniques
for thorax examination?7.4. Interpretation of specific findings and client’s
problems identificationLearning activity 7.4.
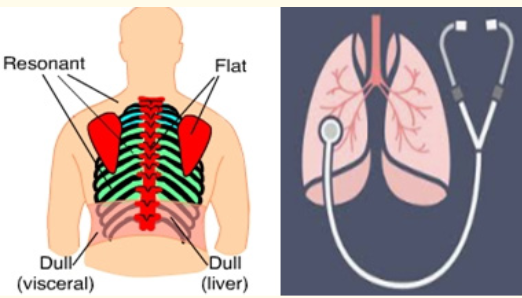
The image above shows areas of percussion and the stethoscope for lung
auscultation. Questions:
1) List the normal findings and abnormal findings of lungs percussion?
2) What are abnormal findings t of auscultation7.4.1. The normal findings and abnormal findings from
respiratory physical examination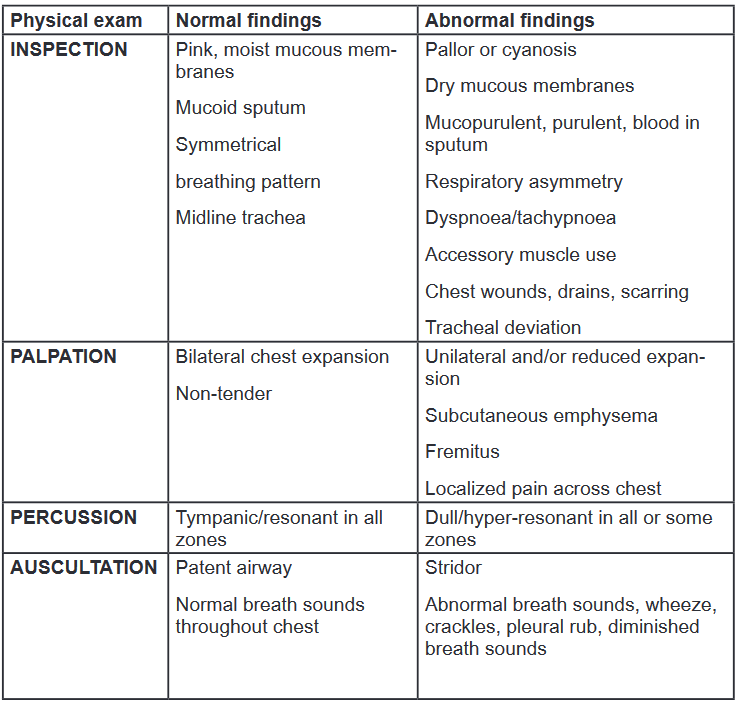
7.4.2. Normal breath sounds
Tracheal: The sound is heard over the trachea and above supraclavicular as very
loud, harsh, and high-pitched. Inspiration = expiration.Bronchial: The sound is heard just above clavicles on each side of sternum, over
the manubrium as loud, harsh, and high-pitched. Inspiration < expiration.Bronco-vesicular: The sound is heard below the clavicles, between the scapulae
as medium-pitched. Inspiration duration = expiration duration.Vesicular: Sound heard over areas of lung tissue as soft and low-pitched. Inspection
> expiration.7.4.3. Abnormal breath sounds
Wheezes: wheezes are whistling or rattling sound in the chest heard during
breathing, as a result of obstruction in the air passages. Wheezes indicate airway
restriction and are typically heard on expiration. Wheeze sound during inspiration
indicates severe airway narrowing. They are high-pitched when produced in small
bronchioles, and low-pitched when produced in larger bronchi. Monophonic (i.e.
single pitch) when heard in an isolated area, and polyphonic (i.e. multi-pitched)
when heard throughout the lung area. Causes include broncho constriction, airway
inflammation, secretions, and obstruction.Crackles: Crackles are adventitious lung sounds heard on auscultation of the chest,
produced by air passing over retained airway secretions or the sudden opening of
collapsed airways. Crackles indicate instability of airways collapsing on expiration.
Fine crackles can be heard in small airways, and coarse crackles can be heard in
larger airways. Causes include pulmonary oedema, secretions, atelectasis, and
fibrosis.Pleural rub: indicates inflammation of the parietal and visceral layers of the pleura.
Stiff creaking sound heard throughout inspiration and expiration. Causes include
pleurisy.Diminished or absent breath sounds: indicate lack of ventilation and/or respiration.
Causes include pneumothorax, pleural effusion, gas trapping, and collapse
Stridor: Loud high-pitched crowing or honking sound louder in upper airway. The
causes may include laryngeal or tracheal inflammation or spasm from epiglottitis,
croup, or aspiration of a foreign object can cause stridor.7.4.4. Abnormal percussion sounds
Dullness: indicates a solid structure, a consolidated or collapsed area of lung, or a
fluid-filled area, which produces a dull note on percussion. Causes include pleural
effusion, infection, and lung collapse.Hyper-resonance: indicates a hollow structure, which produces a hyper-resonant
note on percussion. Causes include pneumothorax.7.4.5. Abnormal findings from inspection of thorax
Normal adult: Anterior-posterior: lateral ratio is 1:2, wider than it is deep, oval
shaped. Cone shaped from head to toe.Kyphoscoliosis: With kyphosis, the thoracic spine curves forward, compressing
the anterior chest and reducing inspiratory lung volumes. With scoliosis, a lateral
S-shaped curvature of the spine causes unequal shoulders, scapulae, and hips. In
severe cases, asymmetry may impede breathing.Barrel chest: Anterior-posterior: lateral ratio near 1:1, round shaped. Ribs are more
horizontal and costal margin is widened. Barrel chest is associated with COPD,
chronic asthma, and normal aging.Pectus excavacum: Depression in lower part of an adjacent to sternum. Congenital
condition may compress heart or great vessels and cause murmurs.Pectus carinatum (pigeon chest): Sternum is displaced anteriorly, depressing the
adjacent costal cartilages. Congenital condition with increased anteroposterior
diameter.Flail chest: Sternum is displaced anteriorly, depressing the adjacent costal
cartilages. It may be a congenital condition with increased anteroposterior diameter.7.4.6. Abnormal findings from palpation of thorax and neck
Tender areas: may indicate muscle strain, rib fracture, or soft tissue damage. With
trauma, air can enter lungs and escape, creating a crackling sensation (crepitus).
Subcutaneous emphysema migrates and may be found in the head and neck. If the
amount is large, mark borders with a pen to note changes.Asymmetrical movements: indicate collapse or blockage of lung. Patients with
muscle weakness, respiratory disease, recent surgery, chest wall abnormalities, or
obesity may have reduced chest expansion.Tactile fremitus: Conditions that may lead to decreased or absent fremitus include
obstructed bronchus, COPD, pleural effusion, fibrosis, tumor, pneumothorax,
obesity, or an extremely large chest. Increased fremitus may accompany severe
localized pneumonia or lung tumor.Tracheal deviation: There are several causes for a tracheal deviation, and the
condition often presents along with difficulty breathing, coughing and abnormal
breath sounds. The most common cause of tracheal deviation is a pneumothorax,
which is a collection of air inside the chest, between the chest cavity and the lung.7.4.7. Abnormal findings from general inspection
Breathlessness, use of accessory muscles, and exhalation with pursed lips:
The combination of mentioned signs indicates the evidence of respiratory distress.Respiratory movements and rate: respiratory rate is 12 to 20 breaths per minute
for adults, with regular rhythm. Tachypnea is greater than 24 breaths per minute;
bradypnea is less than 10 breaths per minute.Oxygen saturation: oxygen saturation level normal is 95% to 100%. Pulmonary
embolism produces hypoxemia.Lymph nodes enlargement: Patients with pneumonia may present with unusually
enlarged mediastinal lymph nodes, which are most likely, a result of a strong
immune response to pneumonia.7.4.8. Abnormal respiratory pattern
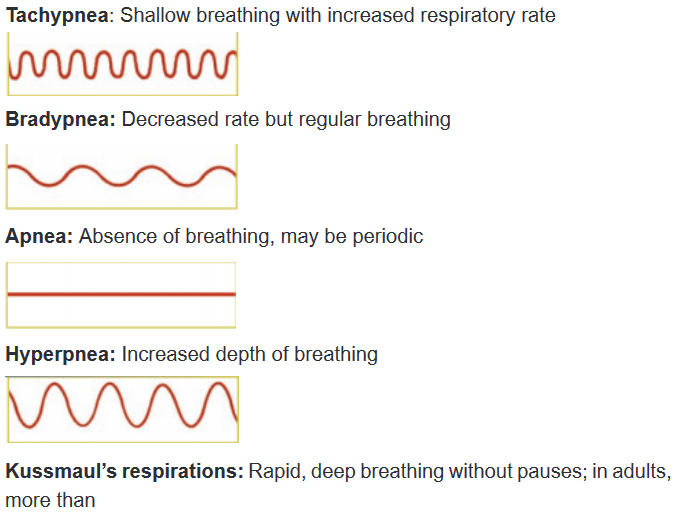
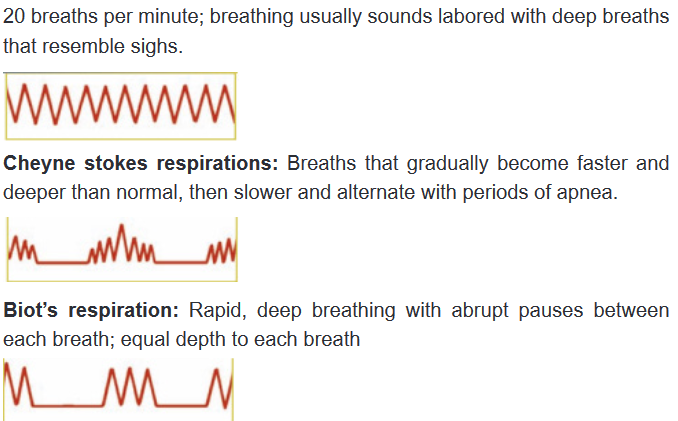
7.4.9. Common associated nursing diagnosis and interventions
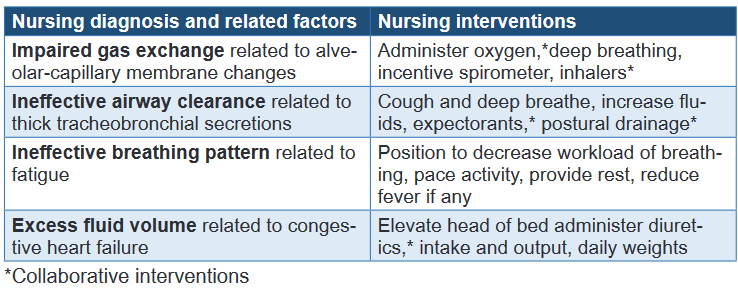
Self-assessment 7.4.
1) When multiple ribs are fractured, paradoxical movements of the chest
may occur. As the diaphragm pulls down during inspiration, negative
pressure causes the injured area to cave inward; during expiration it
moves out. This situation happens in case of:
b) Barrel chest
c) Flail chest
d) Kyphoscoliosis
e) Pectus carinatum2) The normal level of oxygen saturation is:
a) 100%
b) 95%
c) 90-100%
d) 95-100%3) Tachypnea is a condition in which respiratory rate becomes greater than:
a) 24 breaths per minute
b) 20 breaths per minute
c) 22 breaths per minute
d) None of the above4) The lymph node enlargement observed during respiratory assessment
may indicate:
a) Bronchial asthma
b) Respiratory distress
c) Pulmonary embolism
d) Pneumonia5) Recall at least four (4) respiratory abnormal patterns that may be assessed?
6) List two normal breath sounds obtained through lungs auscultation?
7) Differentiate wheezes from crackles abnormal lung sounds?
8) Outline two nursing diagnoses related to respiratory system?
End unit assessment 7.
Select the bests answer, only one option is accepted:
1) Respiratory history taking is the key element of respiratory assessment
to:
a) Valid diagnosis
b) To make a therapeutic plan for patient
c) To help health care provider filling patient’s file
d) To prevent complications related to the patient’s diagnosis2) Dyspnea due to respiratory problems cannot be differentiated at first
glance from dyspnea due to cardiac disease, neuromuscular weakness,
or simple obesity, the following questions can be asked to explore the
origin of dyspnea but the one has no impact on respiratory history taking:a) What makes the breathing worse?
b) Does anything make breathing better?
c) What is family planning used method?
d) What can’t you do because of the breathlessness?3) Wheezes are sounds that are heard continuously during inspiration
or expiration, or during both inspiration and expiration .They are most
commonly heard at end inspiration or early expiration and they are caused
by:
a) Airways narrowed by constriction,
b) Air passing through a solid structure,
c) Laryngeal or tracheal inflammation,
d) A hollow structure producing hyper-resonant sound4) There are several causes for a tracheal deviation observed through
palpation or inspection of neck. The condition often presents along with:
a) Cyanosis
b) Pallor
c) Poor oxygen saturation
d) Difficult breathing, coughing and breath sounds5) The most common cause of tracheal deviation is:
a) Pneumonia
b) Pneumothorax
c) Bronchial asthma
d) Chest asymmetry6) Patients with pneumonia may present with unusually enlarged mediastinal
lymph nodes, which are most likely, a result of:
a) Neck indicate muscle strain
b) Thick tracheo-bronchial secretions
c) Alveolar-capillary membrane changes
d) A strong immune response to pneumonia7) The impaired gas exchange is the respiratory nursing diagnosis observed
among patients consulted for respiratory problem; the most related
nursing factor include the following:
a) Thick tracheo-bronchial secretions
b) Alveolar-capillary membrane change
c) Increased fluid volumed) Fatigue
8) The nursing interventions to perform towards patient with ineffective
airway clearance include the following except one:
a) Increase fluids, expectorants
b) Administer anti-histamine drugs
c) Cough and deep breathe
d) Postural drainage
9) Outline the sequences of respiratory focused physical examination?
10) List four respiratory abnormal pattern findings ?UNIT 8: GROWTH AND DEVELOPMENT
Key unit competence:
Analyse the concepts and theories of growth and development in interpersonal
relationships.
8.1. Definitions
Learning activity 8.1.
https://www.medicalnewstoday.com/articles/154874
Read the link above and answer to the following questions:
1) What is psychology?
2) What is developmental psychology?8.1.1. Psychology
Psychology is the study of mind and behavior, it encompasses the biological
influences, social pressures, and environmental factors that affect how people think,
act, and feel. Psychology is defined as a science which studies mental processes,
experiences and behavior in different contexts.The four main goals of psychology are to describe, explain, predict and change
the behavior and mental processes of others.a) To describe
Describing a behavior or cognition is the first goal of psychology. This can enable
researchers to develop general laws of human behavior.b) To explain:
Once researchers have described general laws behavior, the next step is to explain
how or why this trend occurs. Psychologists will propose theories which can explain
a behavior.c) To predict
Psychology aims to be able to predict future behavior from the findings of empirical
research. If a prediction is not confirmed, then the explanation it is based on might
need to be revised.d) To change
Once psychology has described, explained and made predictions about behavior,
changing or controlling a behavior can be attempted.8.1.2. Developmental psychology
Developmental psychology is the development of human being’ cognitive, emotional,
intellectual, and social capabilities and functioning over the course of a normal life
span, from infancy through old age.Developmental psychology is a scientific approach which aims to explain growth,
change and consistency though the lifespan. Developmental psychology looks at
how thinking, feeling, and behavior change throughout a person’s life.A significant proportion of theories within this discipline focus upon development
during childhood, as this is the period during an individual’s lifespan when the most
change occurs.The three goals of developmental psychology are to describe, explain, and to
optimize development.a) To describe development
It is necessary to focus both on typical patterns of change (normative development)
and individual variations in patterns of change.b) To explain development
Developmental psychologists must also seek to explain the changes they have
observed in relation to normative processes and individual differences.c) To optimize development
Developmental psychologists hope to optimize development, and apply their
theories to help people in practical situations (e.g. help parents develop secure
attachments with their children).Self-assessment 8.1
1) Define psychology
2) List and explain at least two goals of psychology
3) Define developmental psychology
4) List and explain at least two goals of developmental psychology8.2. Growth and development
Learning activity 8.2.
Most people use the terms “growth” and “development” interchangeably and accept
them as synonymous. But in reality, the meanings of these two terms are different.8.2.1. Growth concept and definition
Growth is physical change and increase in size which can be measured quantitatively.
The pattern of physiological growth is similar for all people where the growth rate
varies throughout the lifespan. Growth is more rapid during the antenatal, neonatal,
infancy and adolescent stages and slower during childhood and minimal during
adulthood.Growth refers to physical increase in some quantity over time. It includes changes
in terms of height, weight and different organs of the child’s body. It means that
growth involves all those structural and physiological changes that take place within
individual during the process of maturation.Hurlock has defined Growth as “change in size, in proportion, disappearance of old
features and acquisition of new ones”.Measuring Growth
There are various measurements that are used to measure growth. These are:
Weight, Height, Head circumference, Mid-upper arm circumference (MUAC), and
the eruption of teeth.8.2.2. Development: concept and definition
Development is an increase in the complexity of function and skill progression. It
is the capacity and skill of a person to adapt to the environment. Development is
the behavioral aspect of growth (e.g. a person develops the ability to walk, to talk
and to run).Development is the progressive acquisition of various skills such as head support,
speaking, learning, expressing the feelings and relating with other people. Each
child follows a unique path in growth and development that is laid down from the
beginning of life by what he has inherited from both parents genetically. However thus
may be changed by different factors such as infections, lack of care, psychological
trauma, bad education, and malnutrition.The normal well-fed infant who is protected from infections develops quickly,
particularly during the first 3 months. It is very important to know the age ranges
when most children acquire certain skills. The various skills the baby and a young
child learn are called milestones. In monitoring development, notice at what age
the child achieves various milestones, such as smiling at the mother, sitting without
support, grasping objects with his/her hands, standing, walking and talking.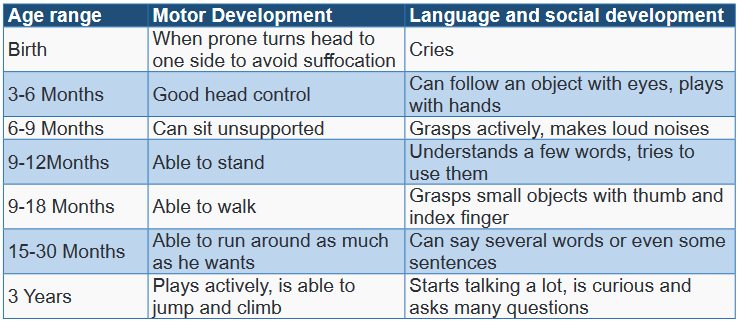
Growth and development are independent and interrelated processes. For example,
an infant’s muscles, bones and nervous system must grow to a certain point before
the infant is able to sit up or walk. Growth generally takes place during the first 20
years of life; development takes place during that time and also continues after that
point.Stages of growth and development
The rate of a person’s growth and development is highly individual; however, the
sequence of growth and development is predictable. Stages of growth usually
correspond to certain developmental changes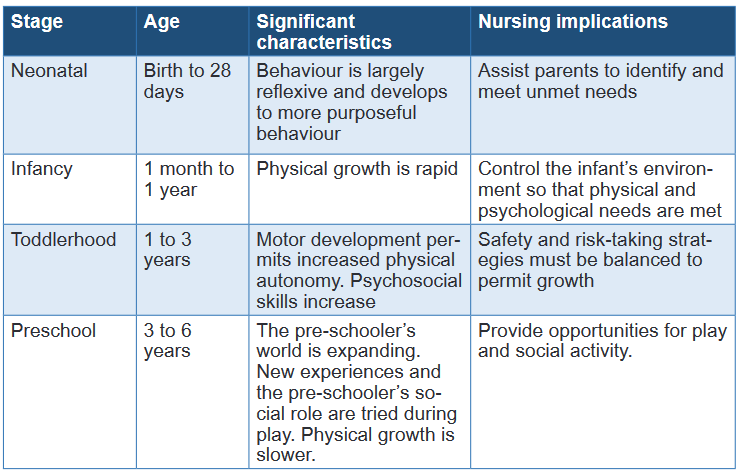
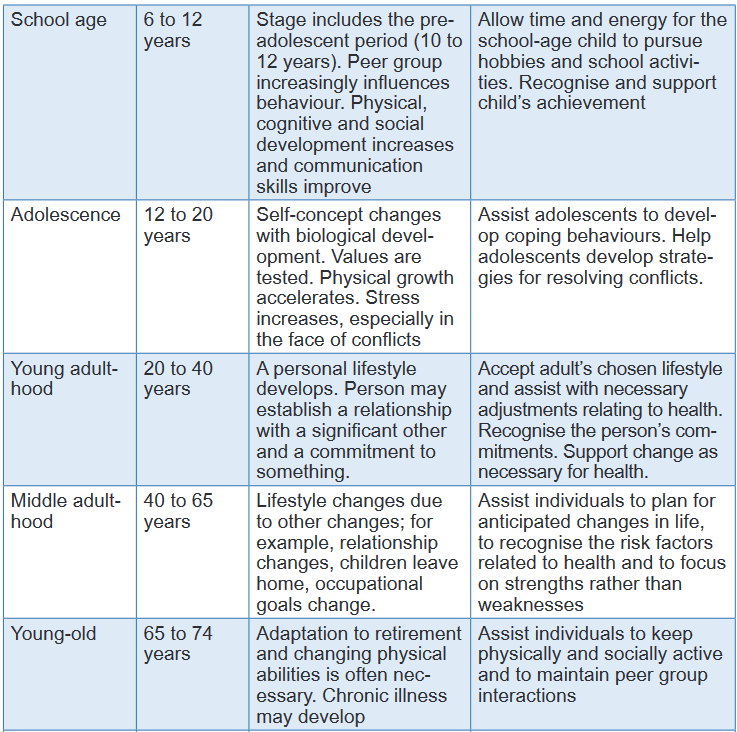
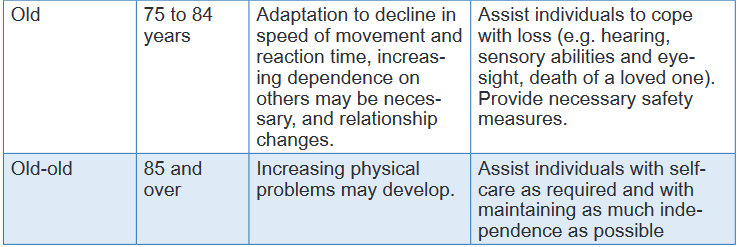
Self-assessment 8.2.
1) Make a brief difference between the concept of growth and development
2) What is milestone8.3. Principles of human development
Learning activity 8.3.
Open and read the following link and answer to the questions below
https://ddceutkal.ac.in/Syllabus/MSW/PAPER-3.pdf.
1) list the different principles of human developmentThere are several basic principles that characterize the pattern and process of
growth and development. These principles describe typical development as a
predictable and orderly process. Even though there are individual differences
in children’s personalities, attitudes, behaviour and timing of development, the
principles and characteristics of development are universal patterns Development involves change
The human being is undergoing changes from the moment of conception to the
time of death. There are different types of change that occur such as changes in
size, proportions, disappearance of old features and acquisition of new features
etc. Development is a continuous process
Development continues throughout the life of an individual. The process of human
development starts with simple acts and progresses to complex or integrated acts.
This process takes place in interaction with the environment in which a person lives.
One stage of development is the basic framework for the next stage of development.
A child has limited knowledge and experiences about his environment. But as he
develops, he acquires more information through explorations and adds to the skills
already acquired and the new skills become the basis for further achievement and
mastery of skills. For example, the child is able to write and draw, he must have
developed a hand control to hold a pencil and crayon. Development follows a direction and uniform pattern in an orderly
manner
(i) Development proceeds from the center of the body outward. This is the principle
of proximodorsal development that describes the direction of development (from
nearer to far apart). It means that the spinal cord develops before outer parts of the
body. The child’s arms develop before the hands and the hands and feet develop
before the fingers and toes.(ii) Development proceeds from the head downwards. This is called the
cephalocaudal principle. According to this principle, development occurs from head
to tail. The child gains control of the head first, then the arms and then the legs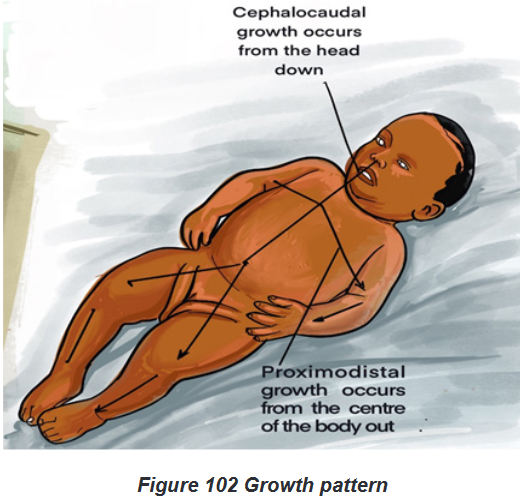
Individual Differences in the Development Process
Even though the pattern of development is similar for all children but the rate of
development varies among children. Each child develops as per his abilities and
perception of his environment. Children differ from each other both genetically
and environmentally. So, both biological factor and environmental situations have
their impact on individual’s development which leads to individual differences in
development. Development depends on maturation and learning
Maturation refers to the sequential characteristic of biological growth and
development. The biological changes occur in sequential order and give children
new abilities.Changes in the brain and nervous system account largely for maturation. The child’s
environment and the learning that occurs as a result of the child’s experiences
largely determine whether the child will reach optimal development. An enriched
environment and varied experiences help the child to develop his/her potential.Learning can either help or hinder the maturational process depending on what is
learned. Development is predictable
Human development is predictable during the life span. Although this development
is influenced by both genetic and environmental factors, however, it takes place in
a pre-defined manner. Specific areas of development, (such as: different aspects
of motor development, emotional behavior, speech, social behavior, concept
development, goals, intellectual development, etc) follow predictable patterns. For
example, the growth of the child in height and weight continues up to a certain age. Early development is more critical than later development
Certain stages of growth and development are more critical than others. It is known,
for example, that the first 10 to 12 weeks after conception are critical. The incidence
of congenital anomalies as a result of exposure to certain viruses, chemicals or
drugs is greater during this stage than others.Milton said that the childhood shows the man, as morning shows the day and also
Erikson states that childhood period is the scene of man’s beginning as man. He
explains that if parents gratify the needs of the child for food, attention and love,
his perception towards people and situation remains positive throughout his life.
He develops positive attitudes, feels secure, emotionally stable and adjust well
with the environment. If negative experiences occur during early life of the child,
maladjustments may take place. Development involves social expectations
In every society there are certain rules, standards and traditions which everyone is
expected to follow. Development is determined by social norms and expectations of
behaviors form the individuals. Children learn customs, traditions and values of the
society and also what behaviors are expected from them. As societies are evolving,
changing traditions and cultural patterns of a society are learned automatically by
children during their development process. Development has potential hazards
Development may be hindered by various hazards such as physical, environmental
or psychological type. These hazards may be originated from the environment in
which the child grows or due to hereditary factors which may have negative impact
on physical as well as socio-psychological development of the child. Happiness varies at different periods of development
Childhood is the happiest period of life and puberty is the unhappiest. The patterns
of happiness vary from child to child and it is influenced by the background process
of the child.Self-assessment 8.3.
1) Development is a never-ending process. This statement is related which
principle of development?
a) Principle of continuity
b) Principle of integration
c) Principle of interaction
d) Principle of inter relationship2) This is not a principle of development
a) Development is continuous
b) Development is consistent
c) Development is lifelong
d) None of the above3) The law of development direction includes
a) Cephalocaudal law
b) Proximodistal law
c) Both a and b
d) Neither a nor b4) Which of the following statement is incorrect about the principles of child
development?
a) Development follows a definite and predictable pattern
b) All individuals are similar in their development
c) Development is product of hereditary and environment
d) Development works on the principle of integration5) Out of the following, which is not correct principle in the context to growth
and development?
a) Foot to head
b) From near to distant
c) Head to foot
d) Interaction of heredity and environment6) A child first learns moving his hand, then fingers and then hand and fingers
together. Which principle of growth and development is represented by
this example?
a) Principle of continuity
b) Principle of directional development
c) Principle of general to specific
d) Principle of individual differences
8.4.1. Comparison of growth and development
Growth mainly focuses on quantitative improvement while development
is associated with both qualitative and quantitative improvement
For instance, growth is associated with measurable changes in weight and height.
When your child’s weight increases from 35 kilograms to 40 kilograms, then the
5kilogram increment is attributed to growth. On the other hand, development isidentified when substantial changes in Intelligence Quotient (IQ) are recorded in
your child’s brain power. For instance, your child’s IQ level is relatively low during
childhood but can improve significantly into adulthood. Your child’s IQ level can
improve from 50 to 90 after improving their creative and critical thinking skills. Growth ends at maturation while development continues until an
individual’s demise (death).
As a teacher or parent, it is important to note that growth ends at maturation. Your
child will experience various changes associated with growth between childhood and
maturation at adolescence. This means that your teaching approach will be different
at age 6 and age 15. At 6 years, your child needs simplified information that they can
understand because their brain can only process basic information. At 15 years, your
child’s brain has improved significantly, and they are in a unique position to grasp and
retain complex information based on their improved information processing skills. Growth is dependent on cellular changes while development is
dependent on organizational transformation
Growth begins at conception and progresses into adulthood. From conception, your
child’s body experiences massive changes based on changes in cellular growth.
An increase in cellular size and number indicates that your child is undergoing
growth. Development is often witnessed at a home or school environment when
your child experiences skillset changes. This simply means that any skills learnt
such as reading or arithmetic are indicative of your child’s development changes.
The older they get, the more likely they are to understand complex skills associated
with computation and reasoning. Growth is external while development is internal in nature
Regardless of your location or occupation, you can observe your child’s growth
based on visible external features. These features include increased body parts
sizes such as hands, legs, ears, and much more. These changes usually manifest
over time based on improved nutrition and general wellbeing. It is important to note
that family instability can also affect your child’s proper growth. Too much stress
from domestic strife subjects your child to stunted growth.Unlike growth, development is an internal process and isn’t visible by the naked eye.
Instead, it requires a comprehensive evaluation of your child’s reasoning, creativity
and innovation to ascertain their development status. This can be achieved by
setting various tests designed to evaluate your child’s IQ in relation with creativity
and reasoning. Based on their performance, you should be in a unique positionto accurately determine their development level and the changes that ought to be
made to rectify the situation. Growth dictates changes in physical appearance while development
dictates change in the character of an individual
Growth is easily discernible based on changes in physical appearance. These
changes manifest over time and include increased body size and voice intonation.
Whether such changes are visible based on hair transformation or skin tone, you
can rest assured knowing that your child is experiencing growth changes.On the other hand, development pays much emphasis in the character changes
of an individual. Your child might have been disobedient during their early age but
over time, they are likely to transform into a mature young adult. With each passing
day, they outgrow certain habits that can only be traced back to character changes. Growth takes place within a limited scope of time while development
takes place within a vast scope of time
This means that growth spans from conception to adolescence depending on your child’s
growth rate. During this period, your child undergoes progressive body changes designed
to transform them into adults. By 25 years of age, your child’s growth rate will have peaked.Development isn’t confined by time or age. Your child can acquire excess of skills
to handle various tasks and challenges regardless of their location or background.
The best part about skill acquisition is that it can still happen beyond 35-year-old if
the determination and commitment exist. Growth focuses on one aspect of your child’s life On the other hand,
development focuses on several aspects of your child’s life such as
emotional state, intelligence and interpersonal skills.
Naturally, growth is a size-oriented process from conception to adulthood. With
every increase in body size, you can monitor your child’s growth rate.On the other hand, development is an all-inclusive process designed to analyze
various aspects of your child’s life. This usually stems from the need to evaluate
their capacity to interact with their peers and adults in an effective way. While their
interpersonal skills might be unpolished at a young age, your child is expected to
make improvements based on their advanced critical thinking and reasoning skills
as they get older.The comparison between growth and development is summarized in the table below:
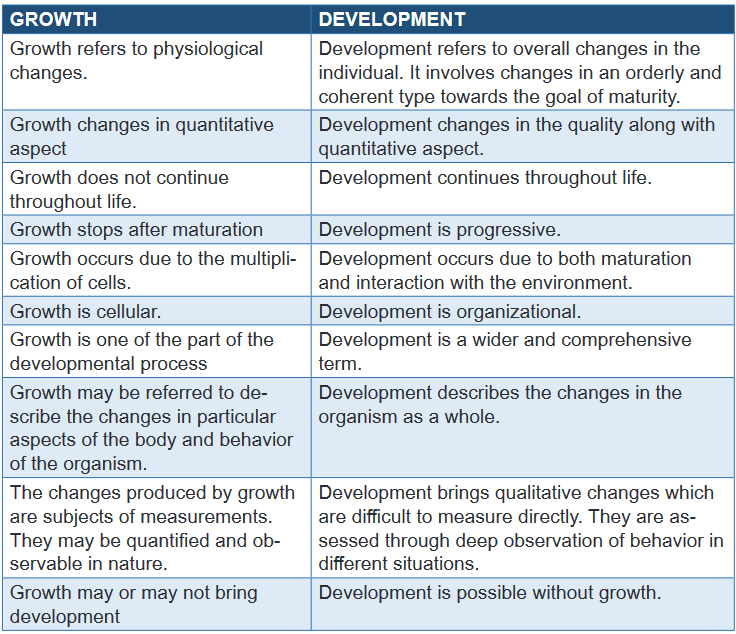
Self-assessment 8.4.
1) It refers to an increase in size evident through physical change
a) Growth
b) Development
c) All of the above
d) None of the above2) It refers to a process of gradual transformation. It is an improvement in
the level of functioning based on the acquisition of skills. It isn’t easily
identified from a glance but only through a comprehensive evaluation of
your child’s performance on various skills and memory retention.
a) Growth
b) Development
c) All of them
d) None of them3) When your child increases in height and weight, is he/she experiencing
a growth process?a) Yes
b) No4) Which of the following best describes Development?
a) It mainly focuses on quantitative improvement
b) It ends at maturation
c) It continues throughout life5) Why is it important to understand the differences in human growth and
development?
a) This knowledge is crucial in helping you formulate ideal learning
styles to disseminate various learning concepts.
b) This knowledge will hinder parents to monitor their children closely
c) This knowledge will confuse learning process8.5. Characteristics of normal and abnormal growth
and developmentLearning activity 8.5.
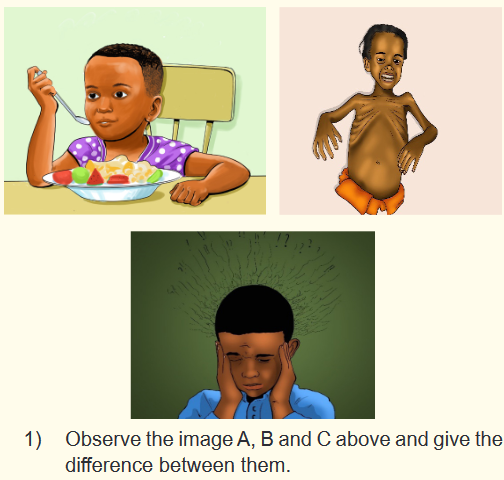
8.5.1. Overview of growth and development
Growth has been described as the work of childhood. Under normal circumstances,
growth proceeds in a predictable fashion from conception to adulthood. Abnormal
growth can be an indicator of a pathologic condition of any organ system as well as
a psychological problem.a) Characteristic of normal growth and development
The growth is considered as physical and developmental milestone that most
children will attain at a specific age. Children undergo various changes in terms
of physical, speech, intellectual and cognitive development gradually until
adolescence. Specific changes occur at specific ages of life when we consider
developmental milestone. Children development stages are organized as follow:
newborn, infancy, toddle, pre-school, school age and adolescent.A newborn is defined as a baby from birth to 2 months. During neonatal period, a
normal newborn reacts automatically to external stimuli, turn their head from side
to side, turn towards sounds and cry to indicate a need.A child from birth to one year is known as an infant. At three to six months of age,
infants can recognize familiar faces, begin to babble, control their head movements
and bring their hands together. By six to nine months of age, infants start sitting
without support, may bounce when held in a standing position and respond to
people calling their name. Infants start communicating with gestures. Between nine
and 12 months old, children can point at things, pick up objects, crawl and even
stand with support, can imitate sound and gestures.A Child between one and three years of age is a toddler. They can stand alone,
learn to walk without help, begin to run and climb stairs with short steps. These
kids can make bye-bye gesture, hold a pencil or crayon, draw a circle, learn to say
several words and even short sentences and even follow simple instructions.A preschool child is from three to five year of age. At this stage, the child’s motor
skills become advanced. Children can throw and catch a ball, skip and hop, learn to
dress themselves and draw proper structures such as a flower. They can speak a
complete, long sentence and even two to three sentences in a stretch easily. With
toilet training, they begin to go to the toilet in the bathroom and use the facility all by
themselves by the age of four years old.School-age child is between 6 to 12 years. School-age children most often have
smooth and strong motor skills. However, their coordination, endurance, balance,and physical abilities vary. This variability affects a child’s ability to write precisely,
dress appropriately, and perform certain tasks, such as making beds or doing
dishes.The adolescence is a period from 10 to 19 years, it is considered as a transitional
phase from childhood to adulthood. In this period, specific characteristics are evident
such as biological changes on secondary sexual characteristics, appearance
consciousness, attraction towards opposite sex, logical and constant thinking,
easily react without considering the pros and cons, select the best career to follow
and determine hobbies.b) Characteristic of abnormal growth and development
If a child shows a very slow or a very rapid growth in relation to height or weight per
age, motor and intellectual capacity need to be examined by a competent health
care provider. The main factors that influence child’s growth are genetic, biological,
nutrition and physical activities.Poor nutrition can make the child more likely to get sick and miss school. A good
breakfast is very important to prevent tiredness and feel motivated.Malnutrition is defined as deficiencies, excesses, or imbalances in a person’s
nutrient intake. Malnutrition includes undernutrition (wasting, stunting, underweight),
inadequate vitamins or minerals and over nutrition which is represented by
overweight and obesity.8.5.2. Biological influences on human growth and behaviors
Early child development is influenced by a wide variety of both biological and
environment factors. Biological factors can play a particularly important role in early
development. These factors influence a child in both positive and negative ways.
They can affect children throughout their development, particularly during critical
times such as the prenatal period and early childhood.Biological factors include
a) Genes
Heredity is a biological process through which the transmission of physical
characteristics takes place from parents to their children. It greatly influences the
different aspects of growth and development i.e. height, weight and structure of
the body, color of hair and eye, intelligence, aptitudes and instincts. Diseases and
conditions such as heart disease, diabetes, obesity and so on can also be passed
through genes, thereby affecting growth and development of the child.b) Hormonal factors
There are multiple glands in the human body. Each of them secrets its own fluid. This
is known as hormone. It is a type of biological component that helps to increase and
decrease the activity of various organs of the human body. Hormone is an important
factor that affects human growth and development in many ways from birth and
its normal functioning and emission is essential for the normal and harmonious
growth and development of human beings. Their timely functioning is critical for
normal physical growth and development in children. Imbalances in the functioning
of hormone-secreting glands can result in growth defects, obesity, behavioral
problems and other diseases. For example, during puberty, the gonads produce
sex hormones which control development of the sex organs and the appearance of
secondary sexual characteristics in boys and girls.c) Nervous system
The nervous system controls a person’s entire physical activity and affects its
growth and development. When a person’s nervous system is defective, his normal
growth and development is disrupted.
d) Physical weakness
Physical weak children are always lagging behind in terms of growth and
development. They often suffer from illness, which affects their physical, mental,
social and emotional growth and development.e) Defective constitutional make-up
Some of the defective body structures are ugly face, abnormally low height,
abnormally high weight etc. These give rise to feelings of inferiority among
individuals. As a result, individuals face social adaptation problems, which affect
their normal growth and development.f) Sex
Sex acts as an important factor of growth and development. There is difference in
growth and development of boys and girls. The boys in general are taller, courageous
than girls but girls show rapid physical growth in adolescence and excel boys. In
general, the body constitution and structural growth of girls are different from boys.
The functions of boys and girls are also different in nature.8.5.3. Factors affecting human development
Growth and development are dependent on a number of factors. Knowledge of these
factors helps the nurse to intervene to promote positive growth and development
of the individual.a) Genetic
The genetic inheritance of each individual is established at conception. It remains
unchanged throughout life and determines human characteristics such as gender,
physical characteristics (eye color, height, hair color) and to some personality.b) Temperament (personality)
Temperament (the way individuals emotionally respond to their external and
internal environment) sets the stage for the interactive dynamics of growth and
development. Temperament persists throughout the lifespan, though attention
must be taken to infants and children to irreversibly categorize them as being of a
particular temperament.c) Family
Families have the most profound impact in nurturing a child and determining the
ways in which they develop psychologically and socially. Whether they are raised by
their parents, grandparents or foster care, they need basic love, care and courtesy
to develop as healthy functional individuals. The most positive growth is seen
when families invest time, energy and love in the development of the child through
activities, such as reading to them, playing with them and having deep meaningful
conversations. Families that abuse or neglect children would affect their positive
development. These children may end up as individuals who have poor social skills
and difficulty bonding with other people as adults.d) Nutrition
Growth and development are dependent on adequate nutrition from conception
and throughout the lifespan. For example, poorly nourished children are more likely
to have infections and other preventable challenges to health and wellbeing than
are well-nourished children. Nutrition is a critical factor in growth as everything the
body needs to build and repair itself comes from the food we eat. Malnutrition can
cause deficiency diseases that adversely affect the growth and development of
children. On the other hand, overeating can lead to obesity and health problems
in the long run, such as diabetes and heart disease. A balanced diet that is rich in
vitamins, minerals, proteins, carbohydrates and fats is essential for the growth and
development of the brain and body.e) Environment
Where you live also has a great influence on how your children turn out to be.
The schools they attend, the neighborhood they live in, the opportunities offered
by the community and their peer circles are some of the social factors affecting a
child’s development. Living in an enriching community that has parks, libraries and
community centres for group activities and sports all play a role in developing the
child’s skills, talents, and behaviour. Uninteresting communities can push some
children to not go outside often but play video games at home instead. Even the
weather of a place influences children in the form of bodily rhythms, allergies and
other health conditions.f) Health and exercise
Illness or injury can alter the rate and patterns of growth and development.
Prolonged or chronic illness may further alter developmental processes, often
most notably physical development. Being hospitalized is stressful for a child
and their family and can alter the child’s coping mechanisms, which may in turn
alter their cognitive, psychosocial and emotional development.
The word exercise here does not mean physical exercise as a discipline or children
deliberately engaging in physical activities knowing it would help them grow.
Exercise here refers to the normal playtime and sport activities which help the body
gain an increase in muscular strength and put on bone mass. Proper exercise
helps children grow well and reach milestones on time or sooner. Exercise also
keeps them healthy and fights off diseases by strengthening the immune system,
especially if they play outside. This is because outdoor play exposes them to
microbes that help them build resistance and prevent allergies.g) Socio-economic status
The socio-economic status of a family determines the quality of the opportunity a
child gets. Studying in better schools that are more expensive definitely has benefits
in the long run. Well-off families can also offer better learning resources for their
children and they afford special aid if the kids need it. Children from poorer families
may not have access to educational resources and good nutrition to reach their
full potential. They may also have working parents who work too many hours and
cannot invest enough quality time in their development.Self-assessment 8.5.
1) Outline 5 factors that affecting human development
2) Discuss how family and socio-economic status influence human
development.
3) Explain how health condition may affect human development
4) The genetic of each individual is established at adulthood and it remains
unchanged throughout life and determines human characteristics such
as gender and physical characteristics.
a) True
b) False8.6. Theories of lifespan and development
Learning activity 8.6.

Observe the image above and respond to the following questions:
1) How many people do you see in this image?
2) Estimate the age of each individual in the image
3) According to everyone activity in the image, do you think is corresponding
to his age?Lifespan development explores how we change and grow from conception to
death. This field of psychology is studied by developmental psychologists and they
have developed different developmental theories including cognitive development,
psychosocial and sociocultural theories of development.8.6.1. Cognitive theories of child development
Cognitive development refers to the manner in which people learn to think, reason
and use language. It involves a person’s intelligence, perceptual ability and ability
to process information. Cognitive development represents a progression of mental
abilities from illogical to logical thinking, from simple to complex problem solving
and from understanding concrete ideas to understanding abstract concepts.
The most widely known cognitive theorist is Jean Piaget. According to him, cognitive
development is an orderly, sequential process in which a variety of new experiences
(stimuli) must exist before intellectual abilities can develop.
Piaget’s cognitive developmental process is divided into five major phases:
the sensorimotor, the pre-conceptual, the intuitive thought, the concrete
operations and the formal operations phase.
A person develops through each of these phases; each phase has its own unique
characteristics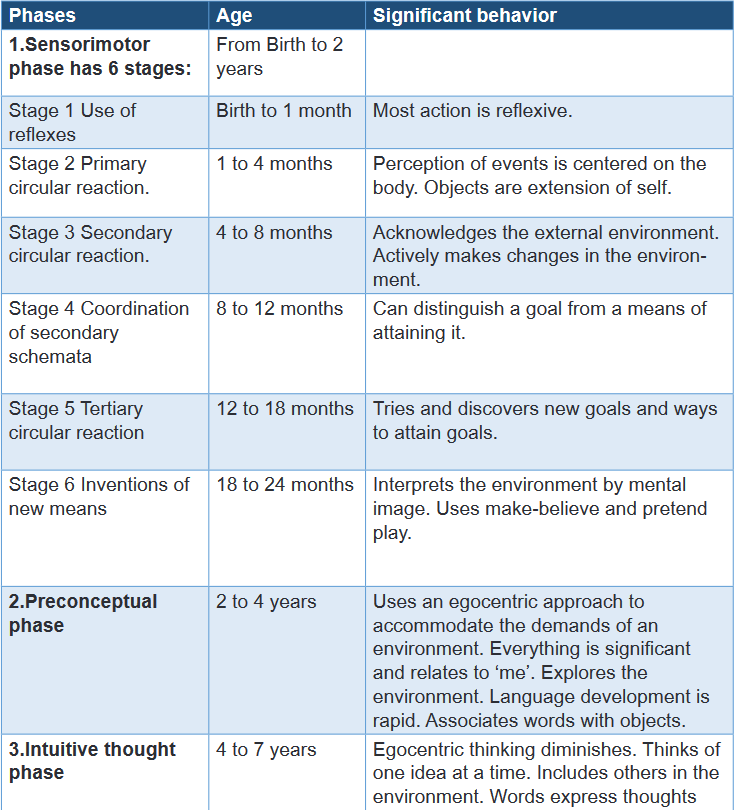
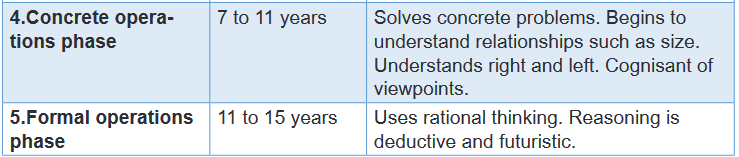
8.6.2. Psycho-social theories of development
Psychosocial development refers to the development of personality. Personality
is complex concept that is difficult to define, can be considered as the outwards
(interpersonal) expression of the inner (intrapersonal) self. It encompasses a
person’s temperament, feelings, character traits, independence, self-esteem, self-
concept, behavior, ability to interact with others and ability to adapt to life changes.Psychosocial theories focus on the nature of self-understanding, social
relationships, and the mental processes that support connections between
the person and his/her social world.
Erik H. Erikson believed that people continue to develop throughout life.
Erikson believed that the more success an individual has at each developmental
stage, the healthier the personality of the individual and he proposed that personality
development takes place all through the life span. Erikson suggested that how we
interact with others is what affects our sense of self.Erikson proposed that we are motivated by a need to achieve competence in certain
areas of our lives. According to psychosocial theory, we experience eight stages of
development over our lifespan from infancy through late adulthood. At each stage
there is a conflict, or task, that we need to resolve. Successful completion of each
developmental task results in a sense of competence and a healthy personality
however failure to master these tasks leads to feelings of inadequacy. According to
Erikson, the environment is highly influential in development.Erikson emphasized that people must change and adapt their behavior to maintain
control over their lives. In his view, no stage in personality development can be
bypassed, but people can become fixated at one stage or regress to a previous
stage under anxious or stressful conditions.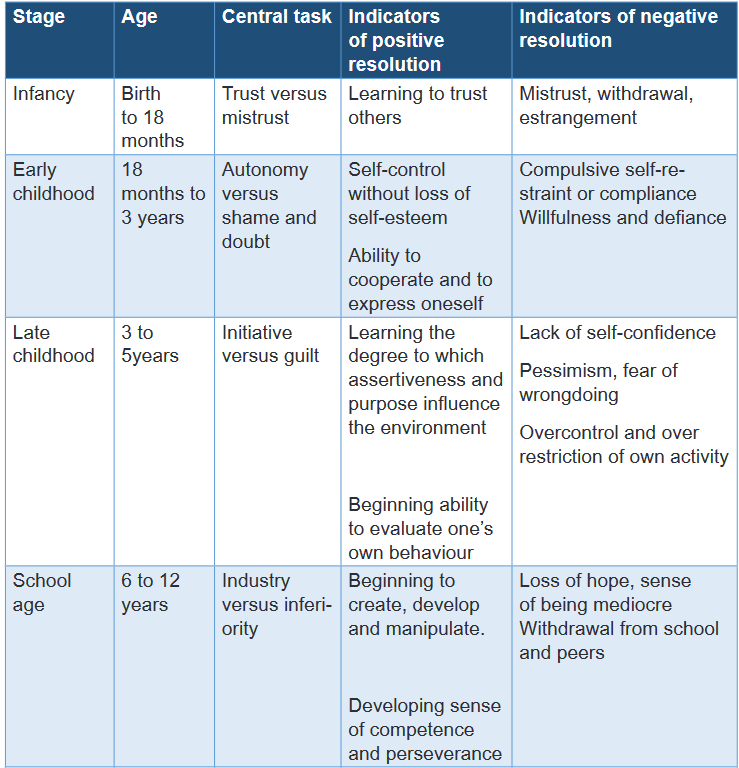
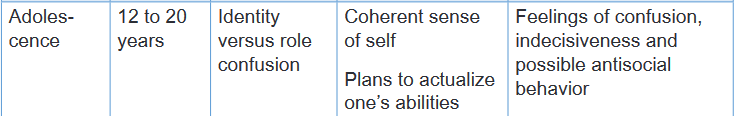
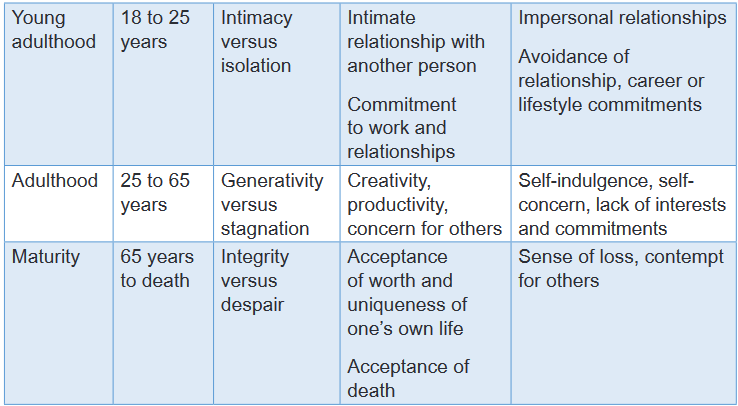
1.1.1. Socio-cultural theory of development (Vygotsky 1896-1934)

Sociocultural theory is an emerging theory in psychology that looks at the important
contributions that society makes to individual development. This theory stresses
the interaction between developing people and the culture in which they live.
Sociocultural theory also suggests that human learning is largely a social process.
Sociocultural theory focuses not only how adults and peers influence individual
learning but also on how cultural and beliefs affect how learning takes place.This theory has been developed by Vygotsky, who believed that each culture
presents unique differences. Because cultures can vary so dramatically, Vygotsky’s
sociocultural theory suggests that both the course and content of intellectual
development are not as universal as Piaget believed. He states that children
are born with basic biological constraints on their minds. Each culture, however,
provides tools of intellectual adaptation. These tools allow children to use their
abilities in a way that is adaptive to the culture in which they liveSelf-assessment 8.6.
1) Match theory to the theorist
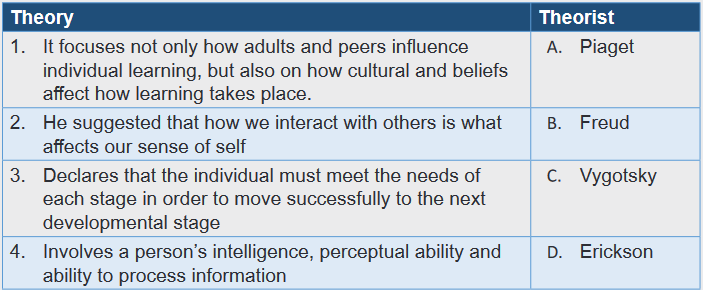
End unit assessment 8.
1) Multiple choice questions
A) Your teacher, Alex compared your recent IQ test with last year. He then
found out that you improve from 60 to 90. Which process did he use in
identifying your IQ?
a) Growth
b) Development
a) None of the aboveB) At 12 months your baby boy started to talk. Under what process does
talking belongs?
a) Growth
b) Development
c) None of the aboveC) Your grandmother noticed that you have grown 1 meter for the span of 6
years. Which process did she use in describing your progress?
a) Growth
b) Development
c) None of themD) After 1 month of holiday your weight increases from 35 kilograms to 40
kilograms, then the 5 kilogram increment is attributed to growth?a) Yes
b) NoE) Even at 50 years, you can still solve the Rubik’s cube in 10 seconds.
Under what process is this?
a) Growth
b) Development
c) None of the above2) Give the difference between psychology and developmental psychology
3) Define growth
4) Outline the measurement of growth
5) Define development
6) Differentiate proximodistal development from cephalocaudal principle
7) Outline at least five principles of development
8) Discuss how nutrition and environment influence human development
9) Outline five major phases of Piaget’s cognitive development
10) Who is the founder of socio-cultural theory?
UNIT 9: PERSONALITY
Key unit competence:
Explain the concepts of personality and behavior developmentIntroductory activity 9
Observe the pictures below and answer the asked questions
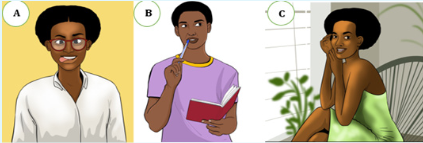
1) What do you see on pictures above?
2) What are differences between pictures A, B and picture C?
3) On your point of view, how do you interpret the picture B9.1. Personality and behavior
Learning activity 9.1.
1) Define personality
2) Define behavior9.1.1. Personality: concept and definition
The term personality is often understood in terms of social attractiveness. A good
personality is considered to be one who impresses other people and who has the
ability to get on well with others. Those who do not possess such ability are said to
have relatively poor personality.Psychologists have attempted to explain the concept of personality in terms of
individuality and consistency. We often observe that people differ a great deal in the
ways they think, feel and act and that too to different or even same situations. This
distinctive pattern of behavior helps one to define one’s identity. Another important
notion in defining the concept of personality is consistency.In other words it can be stated that the concept of personality also rests on the
observation that a person seems to behave somewhat consistently in different
situations over different time.The personality is the special combination of qualities in a person that makes that
person different from others, as shown by the way the person behaves, feels, and
thinks.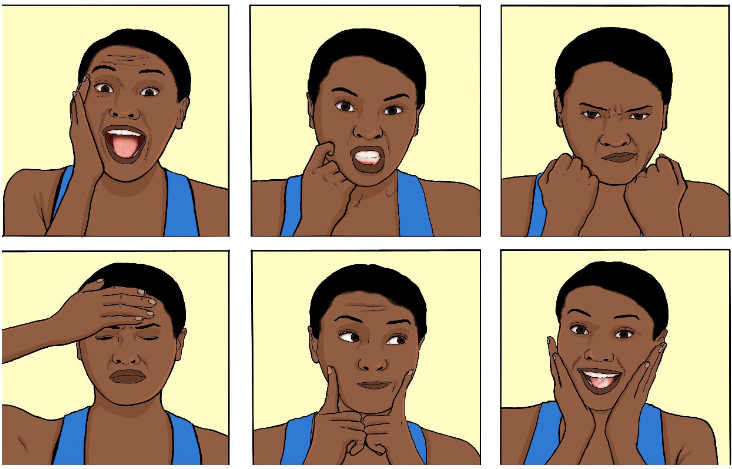
One person can behave differently based on the situation she/he is facing.
Behavior is the way in which one acts or conducts oneself, especially towards
others. It is the way in which an animal or person behaves in response to a particular
situation or stimulus.Types of behaviours
A study on human behaviour has revealed that 90% of the population can be
classified into four basic personality types: Optimistic, Pessimistic, Trusting and
Envious.
Optimists: See the positive side of things. They expect things to turn out
well. They believe they have the skill and ability to make good things happen. Pessimistic: Is defined as “the attitude that things will go wrong and
that people’s wishes or aims are unlikely to be fulfilled. A person with a
pessimistic personality tends toward a more negative or some might say
realistic view of life. Trusting: Trust is a set of behaviors, such as acting in ways that depend
on another. Trust is a belief in a probability that a person will behave in
certain ways. Trust is an abstract mental attitude toward a proposition that
someone is dependable. Trust is a feeling of confidence and security that a
partner cares. Envious: Envious behavior means feeling or showing unhappiness over
someone else’s good fortune and a desire to have the same.
Envious people tend to feel hostile, resentful, angry and irritable. Such
individuals are also less likely to feel grateful about their positive traits
and their circumstances. Envy is also related to depression, anxiety, the
development of prejudice, and personal unhappiness.Self-assessment 9.1.
1) Define personality
2) Explain what good personality meant?9.2. Theories of personality
Learning activity 9.2.
A talkative man G who is your neighbor, complains to you for not being
compatible with his wife. He tells that his wife is irresponsible and he wants to
leave her. As an associate nurse, you plan to make further assessment in that
family to know the root cause of planning to leave the family. While you meet
both the man and the woman, the woman does not speak anything. In return,
the man reacted stipulating that the woman does not trust him and does not
want to perform her responsibilities.The man added that the woman told him angrier to have resemblance figure as
her father who used to maltreat her mother.According to the case described above:
1) Do you have a clue on personality theory? List different personality
theories you know
2) From your understanding what personality problem has the woman, and
the man?9.2.1. Psychodynamic theories of personality
a) Sigmund Freud theory
Sigmund Freud believed that personality is made up of three components.
The id is our impulse energy. It is responsible for all our needs (nourishment,
appreciation) and urges (sexual instinct, hate, love and envy). According to Freud,
the id seeks immediate satisfaction of our needs without referring to logic or morals.
It is demanding, impulsive, blind, irrational, antisocial, and selfish and lust oriented.The superego, or conscience, represents morality as well as the norms of society.
It contains all the ideals for which an individual strives and makes us feel guilty if we
fall short of these standards. The superego essentially is our standard of perfection
the person we want to be. While the id strives for pleasure and the superego for
perfection. The ego acts to moderate the two. It works on the reality principle,
mediating the competing demands of the id and the superego and choosing the
most realistic solution for the long term.Suppose, for instance, that you had a desire to splurge your paycheck on drinks
and partying. That’s your id talking. The superego would be yelling that your idea
is foolish and immoral, and you’re a bad person for even thinking it. The ego will
balance your desire for instant gratification and your desire for responsibility by
figuring out a sensible, rainy-day savings plan with enough left over for some fun
on the weekend.Freud also emphasized the importance of early childhood experiences on the
development of personality. He believed that analyzing the harms of the past could
unlock a person’s development in the future. The harms, Freud believed, were
mostly caused by parents during the person’s childhood.Freud’s views do not meet with absolute approval, and many critics have questioned
the scientific foundation of his work. However, it remains a foundation of modern
psychoanalysis, where people regress or go deeper into their unconscious
personality to resolve the conflicts they’re facing.b) Alfred Adler’s theory of personality
Adlerian therapy, also known as individual therapy, emphasizes the individual’s
ability to bring about positive change in his or her own life. Adlerian therapy consists
of four stages: engagement, assessment, insight, and reorientation. In Adler’s
theory, individuals work to overcome feelings of inferiority and to act in ways thatbenefit the social interest.
In Adler’s approach to therapy, termed individual psychology or Adlerian psychology,
therapy progresses through a series of four stages:1. Engagement where the client and therapist begin to establish the therapeutic
relationship. The relationship should consist of collaboration towards addressing
the client’s problems. The therapist should offer support and encouragement.2. Assessment: The therapist works to learn more about the client’s
background, including early memories and family dynamics. In this part of therapy,
the therapist attempts to understand how the client may have developed certain
styles of thinking that are no longer helpful or adaptive for them.3. Insight: The therapist offers an interpretation of the client’s situation. The
therapist suggests theories about how past experiences may have contributed to
issues the client is currently experiencing; importantly, the therapist leaves it up to
the client to decide whether these theories are accurate and useful.4. Reorientation: The therapist helps the client to develop new strategies that
the client can use in daily life.One of Adler’s most well-known views is that everyone feels inferior at some point
in their lives (i.e. worries that one is not achieving enough). These sentiments of
inadequacy support the pursuit of goals in mentally healthy people, motivating them
to work toward self-improvement. Individuals can achieve great things and make
a significant contribution to society as a whole by learning positive ways of coping
with feelings of inadequacy.Some people, on the other hand, have a hard time coping with feelings of inferiority,
which makes them depressed. Others may act selfishly in order to feel superior
to others in order to cope with feelings of inadequacy in ineffective ways. The
therapist in Adlerian treatment works with the client to provide the support and
encouragement they need to cope more successfully with feelings of inadequacy
and build healthy techniques to overcome these sentiments.According to him, someone with a high level of social interest may go out of their
way to help others, whereas someone with a low level of social interest may bully
or act antisocially. Importantly, social interest levels might fluctuate over time. A
therapist can assist a client in increasing his or her social interest.9.2.2. Trait Theory of Personality
Traits are psychological dimensions such as extroversion, tidiness, emotional
stability, and curiosity. Traits have proven extremely useful for describing personality
and predicting people’s characteristic patterns of thinking, feeling, and behaving Openness: how open-minded you are and how much you like to try new
things (creative, curious, cultured) Conscientiousness or how reliable, organized and diligent you are
(Hardworking, organized, dependable) Extraversion (this is spelled with an “a” in personality psychology), or
whether you draw energy from interaction with others. People who score low
on extraversion (introverts) gain energy from inside themselves. Extraverts
gain energy from people. They tend to be assertive and have the gift of the
gab.
Agreeableness or how friendly, tolerant and compassionate you are
(cooperative, warm, agreeable). Neuroticism (emotional instability), which refers to emotional instability
and the level of negative emotions a person has. People with high levels of
neuroticism tend to be moody and tense.9.2.3. Humanistic theory of Personality
The key agent of the humanist movement is Abraham Maslow. Maslow believed
that personality was not a matter of nature or nurture but of personal choice.
Specifically, he suggested that people possess free will and are motivated to pursue
the things that will help them reach their full potential as human beings.The humanistic perspective emphasized the importance of using free will to become
the best human a person can possibly be. It is different from the other theories in
believing that people are fundamentally good. People are always looking for new
ways to improve, learn and grow, say the humanists, and it’s these choices that
determine our personality and behavior.Abraham Maslow proposed a hierarchy of five innate human needs that activate
and direct human behavior. Maslow described these needs as instinctoid, by which
he meant that they have a hereditary component. Although we come equipped
with these needs at birth, the behaviors we use to satisfy them are learned. In the
hierarchy of needs, each person’s physiological needs are arranged in order of
importance. Lower needs must be partially satisfied before higher needs become
influential. Hungry people feel no urge to satisfy the higher need for esteem whenthey are preoccupied with satisfying their physiological need for food. Safety needs:
security order, and stability. Belongingness, esteem needs (from self and others).
Lastly needs for self-actualization.9.2.4. Behavioural theories
Behavioural theory seeks to explain human behaviour by analysing the antecedents
and consequences present in the individual’s environment and the learned
associations he or she has acquired through previous experience.Behaviourism is the theory that people’s behaviour is the result of the rewards
and punishments they have experienced in the past. Applied to personality,
behaviourism is the view that people are different from one another because they
have experienced different patterns of rewards and punishments, which have
reinforced different behaviours in different people; therefore, they have developed
different personalities. Example: A person whose parents laughed at her jokes all
the time might end up making more jokes later in her life than someone whose
parents did not react when she made jokes.Behaviourism is only concerned with observable stimulus-response behaviours, as
they can be studied in a systematic and observable manner9.2.5. Comparison of personality theories
The study of personality has a broad and varied history in psychology, with an
abundance of theoretical traditions. The major theories include six different
personality theories:
Psychoanalytic theory,
Behaviourist theory
Humanistic theory,
Trait theory,
Social-cognitive theory,
Biological theory.9.2.6. Comparison of personality theories
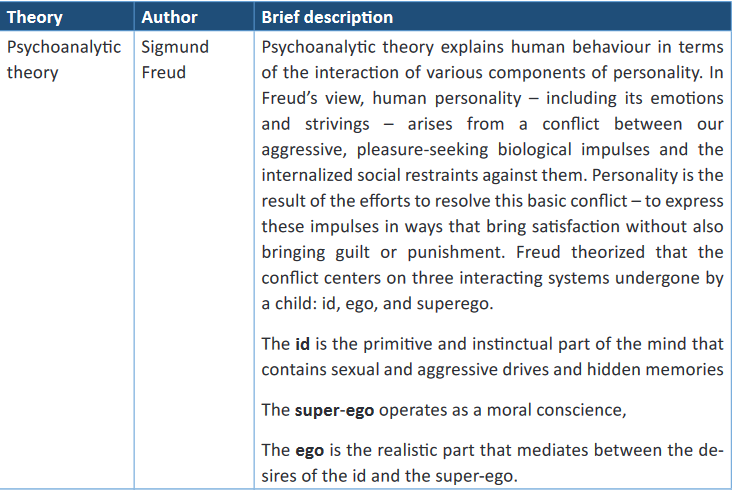
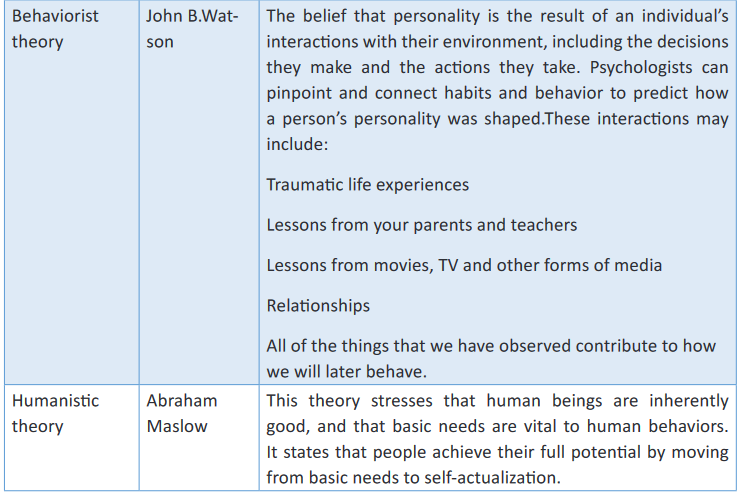
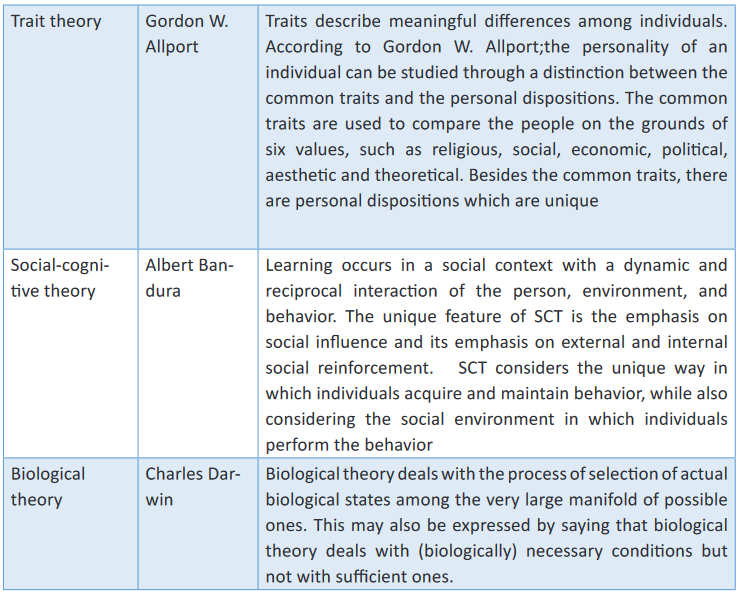
9.2.7. Structuring personality
Is the ordering of the personality with regard to its basic elements and their union
with one another?Personality structure: “The personality structure of one individual can be alike to
or vastly different from another person, regardless of their relation to one another.”a) Topographical aspects of mind
The famed psychoanalyst Sigmund Freud believed that behavior and personality
were derived from the constant and unique interaction of conflicting psychological
forces that operate at three different levels of awareness: the preconscious,
conscious, and unconscious. He believed that each of these parts of the mind
plays an important role in influencing behavior.The preconscious consists of anything that could potentially be brought into the
conscious mind. The conscious mind contains all of the thoughts, memories,
feelings, and wishes of which we are aware at any given moment. This is the aspect
of our mental processing that we can think and talk about rationally. This alsoincludes our memory, which is not always part of consciousness but can be retrieved
easily and brought into awareness. The unconscious mind is a reservoir of feelings,
thoughts, urges, and memories that are outside of our conscious awareness. The
unconscious contains contents that are unacceptable or unpleasant, such as
feelings of pain, anxiety, or conflict.9.2.8 Dynamic aspects of mind
The mind has an internal structure three parts with separate motivations: Id
(irrational and emotional part of the mind); the Ego (rational part); and the Superego
(the moral part). Freud came to see personality as having three aspects, which
work together to produce all of our complex behaviors: the Id, the Ego and the
Superego. All 3 components need to be well balanced in order to have good amount
of psychological energy available and to have reasonable mental health. However,
the Ego has a difficult time dealing with the competing demands of the Superego
and the Id. According to the psychoanalytic view, this psychological conflict is an
intrinsic and pervasive part of human experience. The conflict between the Id and
Superego, negotiated by the Ego, is one of the fundamental psychological battles
all people face. The way in which a person characteristically resolves the instant
gratification vs. longer-term reward dilemma in many ways comes to reflect on their
“character”. Id, Ego and Superego come under the dynamic aspects of personality.
The dynamic aspects of self-according to Freud refer to the agents through which
conflicts arising in the instincts are resolved. The adult develops ego and superego
out of id through conflicts in the earlier periods of lifeSelf-assessment 9.2.
1) Which component of our personality are we born with, according to Freud
that permits our basic wants to be met?
a) ID
b) Ego
c) Superego
d) No answer2) Which aspect of our personality, according to Freud, recognizes that
other people have needs and that being selfish might harm us in the long
run?
a) Ego
b) Superego
c) Id
d) No answer3) The id, ego and superego can be the best characterized as
a) Located in our brain
b) Part of cortex
c) System that make up personality
d) A and b are correct4) According to Freud, which part of our personality is the moral part that
develops due to the moral and ethical restraints placed on us by our
caregivers?
a) Id
b) Ego
c) Superego
d) No answer5) Which of the following is not one of the big personality traits?
a) Open to new experiences
b) Agreeableness
c) Locus of control
d) Neuroticism6) Which of the following are considered tenants of personality according to
trait theorists?
a) There are only 5 personality trait, people are born with and retain
the same traits throughout their life and they are entirely based on
nature
b) Traits are relatively stable over time, traits influence behavior
c) Traits change based on situation and exposure, trait are affected by
behavior and they do not affect each other (friendly and unfriendly at
once)
d) Traits can be used to predict a person’s behavior and all people
have the same definable traits7) According to Freud, displacement, sublimation and projection are all types
of what?
a) Behavior need
b) Defense mechanism
c) Behavior change
d) Psychosocial stage8) In Freud’s topographic model, the ‘çensor’ guards the border between …
a) The Conscious and the Preconscious
b) The Preconscious and the Unconscious
c) The Conscious and the Unconscious
d) The Ego and the Id9) Which of the following statements is true of the Ego, according to Freud?
a) It exists prior to the Id
b) It follows the ‘pleasure principle’
c) It lends its libidinal energy to the Superego
d) None of the above10) Explain the difference between social and behavior theory
9.3. Defense mechanism
Learning activity 9.3.
Y, a teacher, he has the conflict at with his wife and the beats her in the morning.
When he enters the classroom, he verbally abuses the pupils before giving
them an assignment. He awarded them 0 out of 10 without marking them and
told them that they didn’t know anything, and the pupils responded that those
grades were not for them. According to the case described above:
1) In your opinion, what do you think occurred to this teacher,?Defense mechanism is an often unconscious mental process (such as repression)
that makes possible compromise solutions to personal problems.
Freud believed that part of the reason so much of personality resides in the
unconscious is because many motives, thoughts, and feelings are threatening for
us to admit to ourselves. Thus, we develop means to keep those aspects outside of
our consciousness by developing self-protective strategies.Types of defense mechanisms
Denial is the act of refusing to recognize the existence of something.
Repression is the act of forcing something out of your mind so that you
don’t have to worry about it. You don’t overtly refute it; instead, you choose
to ignore it and eventually forget about it. Reaction formation is convincing yourself of the opposite of what is actually
true.
Projection is blaming someone else for a negative feature or thinking.
Rationalization is the process of coming up with a logical, rational (but
false) reason for a shameful idea or action.
Intellectualization is the process of turning a potentially dangerous feature
or thought into a cold, rational truth.
Displacement is the act of guiding an undesired impulse toward a more
acceptable outcome.
Regression is reverting to an earlier stage of life development when you
are faced with conflict
Sublimation is the process of transforming shameful desires into
something honorable; it is the process of redirecting energy to something
more acceptable..
Compartmentalization Separating your life into independent sectors may
feel like a way to protect many elements of it. Like when you choose to not
discuss personal life issues at work, you block off, or compartmentalize, that
element of your life. This allows you to carry on without facing the anxieties
or challenges while you’re in that setting or mindset.Self-assessment 9.3.
1) Match the types of defense mechanism in A (Types of defense mechanism)
with their respective definitions in column B (their definitions)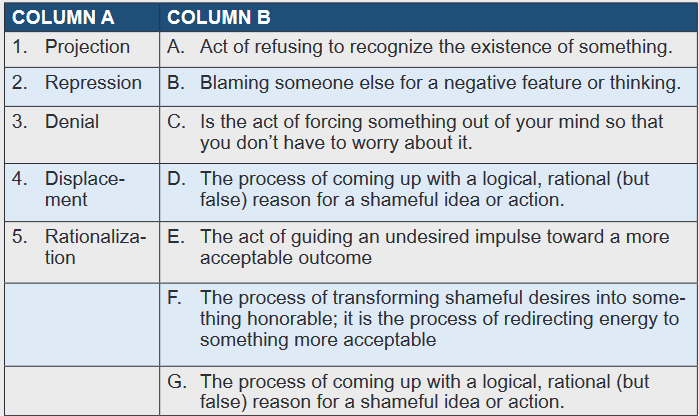
9.4. The five-Factor Model of personality
Learning activity 9.4.
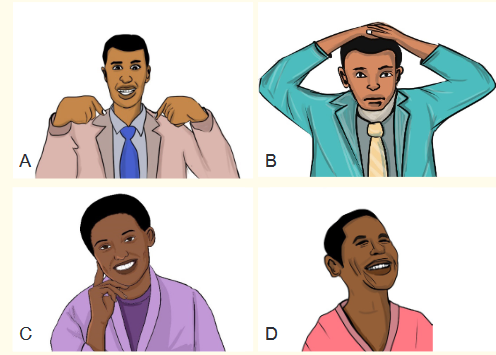
Observe pictures above and answer following questions:
1) What is a difference between pictures above?
2) From your understanding how can you interpret pictures A,B,C and D ?9.4.1. Concept of The five-factor model of personality (FFM)
The five-factor model of personality (FFM) is a set of five broad trait dimensions
or domains, often referred to as the “Big Five”: Extraversion, Agreeableness,
Conscientiousness, Neuroticism (sometimes named by its polar opposite,
Emotional Stability), and Openness to Experience (sometimes named Intellect). Extraversion
The quantity and intensity of preferred interactions, degree of activity, need for
stimulation, and capacity for delight are all indicators of extraversion. Extraverts are
outgoing, lively, talkative, person-oriented, optimistic, fun-loving, and affectionate,
whereas introverts are reserved (but not unpleasant), somber, distant, independent,
and quiet. Introverts are neither sad nor negative, but they lack the enthusiastic
high spirits that are characteristic of extraverts. Agreeableness
Agreeableness, like Extraversion, is an interpersonal attribute that describes the
types of relationships that a person prefers on a scale of compassion to antagonism.
Softhearted, good-natured, trustworthy, helpful, forgiving, and altruistic people havea high A score. They are receptive and sympathetic, and they feel that most others
want to and will behave in the same way they do. Those with a low Agreeableness
score (referred to as hostile) are cynical, rude or even abrasive, distrustful,
uncooperative, and impatient, as well as being manipulative, spiteful, and cruel.Conscientiousness
It measures how well goal-directed behavior is organized, persistent, controlled,
and motivated. Those with a high level of conscientiousness are organized,
dependable, diligent, self-directed, scrupulous, ambitious, and persistent, whereas
those with a low level of Conscientiousness are aimless, unreliable, lazy, careless,
lax, neglectful, and hedonistic. Neuroticism
It describes a long-term state of emotional adjustment and instability. Individuals
with a high level of neuroticism are more likely to experience mental anguish.
Negative affectivity, such as angry anger, depression, anxiety, and volatility, are all
symptoms of high neuroticism, but neuroticism also includes stress sensitivity, self-
consciousness, excessive cravings, urges, and difficulties enduring the frustration
created by not acting on one’s urges. Openness to Experience
Openness to Experience is less widely studied than either Neuroticism or
Extraversion, and is frequently misconstrued, as the alternative name of intelligence
suggests. Openness to Experience, on the other hand, is distinct from ability and
intellect in that it entails the deliberate pursuit and appreciation of experiences for
their own sake. Individuals who are open are more curious, imaginative, and willing
to explore unusual ideas and values than those who are closed; they experience
the full range of emotions more intensely than those who are closed. Closed people
(those with a low level of Openness to Experience) are more traditional in their
views and attitudes, conservative in their tastes, and dogmatic and rigid in their
convictions; they are behaviorally stiff and emotionally unresponsive.9.4.2. Developing personality
Personality development is the development of the organized pattern of behaviors
and attitudes that makes a person distinctive. Personality development occurs by
the ongoing interaction of temperament character, and environment. Personality
development helps an individual to gain confidence and high self-esteem.Personality development also is said to have a positive impact on one’s
communication skills and the way he sees the world. Individuals tend to develop a
positive attitude as a result of personality development. Infancy
An infant goes through the first stage of development throughout the first two years
of life: learning basic trust or mistrust (hope). The newborn learns trust and security,
as well as a basic optimism, after being well-nurtured and loved. When a newborn
is mistreated, he or she grows uneasy and learns “fundamental mistrust.” Toddlerhood
The second stage occurs between the ages of 18 months and two years and
three to four years in early childhood. It’s about Learning Autonomy vs. Shame. If
the child has been well-parented, he or she will emerge from this stage with self-
assurance and a sense of control. Depending on the temperament of the child, the
early stages of this period can also include tempestuous tantrums, stubbornness,
and negativism. Preschool
The third stage occurs during the “play age,” or the later preschool years from
about three to entry into formal school. The developing child goes through Learning
Initiative or Guilt (Purpose). The child learns to use imagination; to broaden skills
through activeplayand fantasy; to cooperate with others; and to lead as well as
to follow. If unsuccessful, the child becomes fearful, is unable to join groups, and
harbors guilty feelings. The child depends excessively on adults and is restricted
both in the development of play skills and in imagination. School age
The fourth stage, Learning Industry or Inferiority (Competence) , occurs during
school age, up to and possibly including junior high school. The child learns to
master more formal skills like relating with peers according to rules ,progressing
from free play to play that is structured by rules and requires teamwork (team
sports) and learning basic intellectual skills (reading, arithmetic). At this stage,
the need for self-discipline increases every year. The child who, because of his or
her successful passage through earlier stages, is trusting, autonomous, and full
of initiative, will quickly learn to be industrious. However, the mistrusting child will
doubt the future and will feel inferior. Adolescence
Adolescents are starting to think abstractly and can comprehend their own self-
identity and personalities. The teenager begins to think about identity issues such
as: Who should I be? What should I place a premium on? And what kinds of hobbies
should I pursue? To establish a strong sense of self-identity, the teen must answer
these questions. This stage is characterized by the exploration of multiple roles and
personalities.From the ages of 13 to 14, the fifth stage, Learning Identity or Identity Diffusion
(Fidelity), occurs during adolescence. During this period, the young person develops
self-assurance rather than self-doubt, and experiments with many constructive roles
rather than embracing a bad identity such as delinquency. In later adolescence, a
defined sexual identity is established, and the well-adjusted teenager looks forward
to achievement. The adolescent seeks leadership (someone to inspire him or her)
and develops a set of values to live by throughout time.
Parents are usually the first to recognize that their child has a problem with emotions
or behaviors that may point to a personality disorder. Young adult
The development of close emotional relationships with other people is a struggle
for a young adult. In this context, the term “intimate” refers to social and emotional
interactions with others rather than sexuality. Those who do not develop a sense of
intimacy, on the other hand, become separated from social contact. Middle-aged adult
Adults in their forties and fifties have a strong desire to leave their mark on the world,
to create something of lasting value and importance. Finding a sense of direction
in life is a major theme. When a person fails to generate something meaningful, he
or she becomes stuck and stops moving forward; as a result, the individual may
become selfish and self-absorbed. Old adult
It is natural in old age to reflect on one’s life and what has been done. Integrity is
developed by people who feel good about what they have done. For people who
have received negative evaluations, there is sadness, as well as a sense of regret
and guilt for the life they have livedSelf-assessment 9.4
1) The big five model of personality contains the following dimensions:
a) Psychotism, neurocism, extraversion, openness, agreeableness
b) openness, conscientiousness, extraversion, agreeableness,
narcissism
c) openness, narcissism, psychotism, conscientiousness, extraversion
d) conscientiousness, agreeableness, neuroticism, openness,
extraversion2) Which of the following is not one of the Big 5?
a) Agreeableness
b) Introversion
c) Neuroticism
d) Conscientiousness3) M. is friendly, always willing to help others and compassionate. We would
expect Lana to score highly on:
a) Extraversion
b) Agreeableness
c) Neuroticism
d) Openness to experience4) John is self-disciplined, focused on achievement and keen to do his duty.
He would be expected to score highly on:
a) Neuroticism
b) Agreeableness
c) Extraversion
d) conscientiousness5) Talkative vs. silent; frank, open vs. secretive; adventurous vs. cautious;
sociable vs. reclusive; these traits describe which dimension of
personality?
a) Agreeableness
b) Conscientiousness
c) Extraversion
d) Culture6) According to Erikson’s eight stages of psychosocial development, during
which age does the psychological stage of trust vs. mistrust develop?a) early childhood
b) infancy
c) adolescence
d) adulthood7) Which of the following is NOT one of the Erikson’s stages of psychosocial
development?
a) Industry vs. Inferiority
b) Trust vs. Mistrus
c) Life vs. Death
d) All of the above are stages8) At what time of life does Erikson stage Industry vs. Inferiority occur?
a) old age
b) adolescence
c) School age
d) infancy9.5. Determinants of behavior
Learning activity 9.5.
When Mr. K and her sister G were in a holidays of end year accompanied their
parents in a marriage party in Eastern province of the country; they remained
there for 2 days because they wanted to visit other student in the village. When
their parents were coming back to Kigali where they live, their car got a severe
accident and both died on site! After burial when K and G went to back to
the school Mr. K remained quiet and did not tell the situation to any one of
classmates while his sister G was constantly crying and telling her friends
about the death of their parents
Answer following questions:
1) In your opinion, what is the reason why Mr. K was so silent?
2) In your opinion, why did his sister tell her friends about her experience?
3) From your understanding, why females talk a lot compared to males?Human behavior is any activity or human activity, both of which can be observed
directly (overt behavior), or which cannot be observed by others (covert behavior)For years psychologists have debated whether human behavior is something
we are born with or something we acquire - the “nature/nurture” debate. There
are four determinants of behavior; prewiring (nature), formative years (nurture),
contemporary society, and creativity. Each have had an important role to play in
the evolution of human kind, namely in the first, second, and third watersheds of
that evolution. Prewiring
The first determinant of our behaviour is “instinct” or “prewiring”, a genetic inheritance
that predisposes us to behave in particular ways. This is the “nature” argument. “I
am the way I am because I was born this way and, given that is the way I am
wired, there is nothing that can be done to change my behaviour.” (If this argument
was totally true, I would not try to learn anything. I either have natural ability or I
do not). Perhaps it is partially true. Prewiring can be demonstrated by the nest-
building practices of birds and the web-spinning of spiders. This is not behaviour
that they have to learn. It is instinct. They have no choice. Prewiring can also be
demonstrated in the human species by psychological differences between men
and women. Women, on average, have greater oral ability. Men, on average, have
higher spatial ability and are more competitive. On these characteristics the human
species has no choice. This is the way we are prewired. Formative Years
The second of the determinants of our behaviour is learned in our formative years
from our experiences with siblings, with parents or with guardians. A child arrives
in the world wishing to survive. It quickly realizes that resources for that survival
come from parents and so the child quickly discovers through trial and error what
strategies will maximize those resources. Further, the child needs to establish for
itself an ecological niche, one in which it is differentiated from others also competing
for resources. The greatest competitors for resources in a child’s life are its parents
and its siblings. Contemporary Society
The third of the four determinants of our behaviour is the contemporary society in
which each of us finds ourselves. People seem to quickly pick up social mannerisms
such as accents and gestures when they relocate between countries or cultures.
It is a case of the unconscious application of the maxim “When in Rome, do as the
Romans do.” Accents are a very obvious example. We acquire them unconsciously
in order to fit in. The need for acceptance, for belonging, for not being too different(in other words the need for “affiliation”) is prewired within us, probably strongly
influencing the second and third determinants of behaviour.
Similarly our oral communication is underpinned by our prewired need to
communicate between members of our species; our introversion or extraversion,
coupled with the language we speak is influenced by our formative years; yet our
ideographic language is contemporary, subtlety changing.
Behaviours based upon those of contemporary society are quite malleable. Our
adaptability as a human species attests to that. Creativity
The fourth determinant of our behaviour is imagination, creativity or innovation,
the ability to imagine and/or construct something hitherto unknown. Although the
bounds of our creativity, the range within which our creativity can occur, is limited
by prewiring, by formative years and by contemporary society (technology, for
example) we’ll never know what those bounds are until we push them.Behaviours based on creativity are the easiest to change. Hence “good ideas”
are very fragile. The conservatism of the human species (anchored to prewiring,
formative years, and contemporary society) attests to the extent to which creativity
is not a strong behavioral determinant.In Summary, It is suggested that our behaviour is influenced by our prewiring, by
our formative years, by the behaviour of those around us which we model, and by
our creativitySelf-assessment 9.5
1) Behavior refers to:
a) Action or reaction of the object or organism, usually in relation to
the environment.
b) Action of human beings only.
c) Reaction of human beings against any action from others.
d) None of the above.2) Which of the following is not a covert behaviour?
a) Thinking
b) Feeling
c) Dreaming
d) Talking3) Which of the following is not an overt behaviour?
a) Dreaming
b) Walking
c) Laughing
d) Fighting4) Choose the letter corresponding to the right response
Behaviors based on …………..……are the easiest to change and is not
a strong behavioral determinant.
a) Prewiring
b) Formative Years
c) Creativity
d) Contemporary Society5) State 4 determinants of human behavior
9.6. The six Stages of Behavior Change
Learning activity 9.6
Observe well images above and answer questions
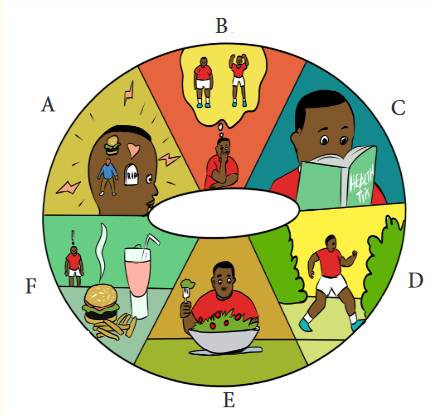
1) Describe the meaning of images A, B, C, D, E and F
2) From your understanding what steps of behavior change?Behaviour change, in context of public health, refers to efforts put in place to change
people’s personal habits and attitudes, to prevent disease. Behaviour change in
public health can take place at several levels and is known as social and behaviour
change. Change occurs gradually and relapses are an inevitable part of the process.
People are often unwilling or resistant to change during the early stages, but they
eventually develop a proactive and committed approach to changing a behaviour. Stage 1: Pre-contemplation
The earliest stage of change is known as precontemplation. During the pre-
contemplation stage, people are not considering a change. People in this stage
are often described as “in denial,” because they claim that their behavior is not a
problem. In some cases, people in this stage do not understand that their behavior
is damaging, or they are under-informed about the consequences of their actions. Stage 2: Contemplation
During this stage, people become more and more aware of the potential benefits of
making a change, but the costs tend to stand out even more. This conflict creates
a strong sense of ambivalence about changing. Because of this uncertainty, the
contemplation stage of change can last months or even years. Stage 3: Preparation
During the preparation stage, you might begin making small changes to prepare for
a larger life change. For example, if losing weight is your goal, you might switch to
lower-fat foods. If your goal is to quit smoking you might switch brands or smoke
less each day. You might also take some sort of direct action such as consulting a
therapist, joining a health club, or reading self-help books. Stage 4: Action
During the fourth stage of change, people begin taking direct action in order to
accomplish their goals. Oftentimes, resolutions fail because the previous steps
have not been given enough thought or time. Stage 5: Maintenance
The maintenance phase of the Stages of Change model involves successfully
avoiding former behaviours and keeping up new behaviours. If you are trying to
maintain a new behaviour, look for ways to avoid temptation. Try replacing old
habits with more positive actions. Reward yourself when you are able to successfully
avoid a relapse. Stage 6: Relapse
In any behaviour change, relapses are a common occurrence. When you go through
a relapse, you might experience feelings of failure, disappointment, and frustration.The key to success is to not let these setbacks undermine your self-confidence. If
you lapse back to an old behaviour, take a hard look at why it happenedSelf-assessment 9.6.
1) Considering six stages of behavior change. A person who does not
regularly exercise makes a plan to exercise in the upcoming month. He
schedules an appointment to speak with his healthcare provider. Which
stage of stages of behavior change does this best describe?
a) Pre contemplation
b) Contemplation
c) Preparation
d) Action2) Doctor tells persons that they’re at risk of developing hypertension unless
they make healthier choices, like daily walks and a better diet. Person
may think there’s nothing wrong with them. Here’s what the stages may
look like for them:
a) Maintenance
b) Contemplation
c) Pre contemplation
d) Relapse3) Your Dad is a drunker, where he takes 5 SKOL a day. As his child who
have information about health you are explaining to him the side effects
and complications of alcohol. He understand that and he starts reading
books to see if what you are saying is true. At which stage of behavior
change does this father is
a) Contemplation
b) Contemplation
c) Preparation
d) Action9.7. Motivation and motivation theories
Learning activity 9.7.
When employer H. arrived at the management centre, he found that some
of the staff were constantly in training and others were not. After collecting
information, he sought out how to help employees to improve their skills. To do
that, he has made a list of employees who will be attending the training and
looking for training that will take place away from their workplace where they
will get money to help them to find accommodation and to attend quiet training
without interfering work and the training1) In your opinion what was intension of the manager to the staffs?
9.7.1. Motivation
Motivation is something that pushes people to do action or feel a certain way.
Motivating someone entails encouraging and inspiring them. Turning on or igniting a
feeling or action is sometimes referred to as motivation. Motivation is quite powerful.
It has the ability to persuade, convince, and motivate you to take action. Motivation,
in other terms, can be defined as a driving force for action. It is a power capable
of completely altering your life. Our lives are propelled forward by motivation. It is
motivated by a desire to succeed. There is no pride in life without success; there is
no happiness or excitement at work or at home. Life can often feel like a skewed
wheel that takes you on a rocky trip. Complacency is the worst enemy of motivation.
Complacency breeds frustration, and frustrated people give up because they can’t
figure out what’s important.You can proceed to attain your goal and motivate others after you comprehend the
principle that motivates the motivator. Your desire and attitude are your internal
motivator. It spreads quickly. The key to achieving the response you want from
others is to have a positive attitude. How can one keep focused and motivated?
There are two sorts of motivation: intrinsic (internal) and extrinsic (external).a. External motivation
Extrinsic motivation is defined as conduct that is influenced by external incentives.
These incentives can be monetary or academic in nature, or intangible in nature, such
as acclaim or celebrity. Extrinsically motivated people will continue to do something
even if it isn’t enjoyable or rewarding in and of itself for example, doing something
at work that you don’t find enjoyable or gratifying in order to earn a living. Extrinsicmotivation is used in operant conditioning, which is when someone or something is
trained to behave in a certain way as a result of a reward or punishment. Although
extrinsic drive can be beneficial in some instances, it can also contribute to burnout
or a loss of effectiveness over time.b. Internal motivation
Internal motivation is the satisfaction that comes from completing a task, not for the
sake of achievement or victory. It’s more than just attaining a goal; it’s a sense of
accomplishment. A rewarding sensation is not obtained by achieving an unworthy
goal. Because internal motivation comes from inside and manifests as self-
motivated, it is long-lasting. To achieve, motivation must be found and continually
strengthened. Keep your objectives in sight and read them every morning and
evening. Recognition and accountability are the two most powerful motivators.
Being valued, treated with respect and decency, and having a sense of belonging
are all aspects of recognition. A sense of belonging and ownership is produced by
taking on responsibilities. People do not believe they are being treated as things.
They believe they are a valuable member of a team. The satisfaction of doing the
right thing is motivating in and of itself.Intrinsic and extrinsic motivation can sometimes complement each other to help
you complete a task. If you have a job and are working on a project, for example,
you may be extrinsically motivated to complete it in order to meet a teammate’s
deadline. You may be organically motivated to complete the assignment because
you enjoy working on it and want to do a good job.9.7.2. Motivation theory
a. Content theories
The idea that motivation is based on the needs of the individual is emphasized in
content theories. Need can be defined as a state in a person’s life that motivates
them to act and engage in certain behaviours. Individual needs, and thus motivation
levels, vary, according to content theorists. These theories are often known as needs
theories since they are generally associated with a perspective that emphasizes
the need of figuring out “what” motivates us. They try to figure out what our “needs”
are and then link motivation to meeting those needs. The following are some of the
most important content theories:i. Maslow’s hierarchy of needs
Maslow’s hierarchy of needs is a motivation theory that argues that an individual’s
conduct is dictated by five categories of human needs. Physiological needs, safety
needs, love and belonging needs, esteem needs, and self-actualization needs are
some of these needs.When a lower need is met, it no longer motivates behaviour; instead, the next higher
need takes over. The five needs are arranged in a logical order. When lesser wants
are met, higher needs become more significant. Higher-order motivation comes
from higher-order needs. Priorities fluctuate from person to person. The approach
aids managers in determining which specific demands are important to employees
and, as a result, appropriate motivators.ii. Alderfer’s ERG Theory
Alderfer developed a model of motivation aligning with Maslow’s motivation theory
by reducing the five needs suggested by Maslow to three needs. These needs are
Existence, Relatedness and Growth. According to Alderfer, there is no hierarchy
of needs and any desire to fulfil a need can be activated at any point in time. This
results in the lower level needs not requiring to be satisfied in order to satisfy a
higher level need.Existence needs: include the necessity for material and energy exchange, as well
as basic physiological and safety requirements.Relatedness needs: interactions with human surroundings, sharing or mutuality
process; desire for interpersonal relationships and attention; is similar to Maslow’s
social needs and part of the esteem needs.Growth needs: People make creative or productive efforts for themselves; personal
growth and development are part of Maslow’s esteem and self-fulfillment wants.
Unlike Maslow, more than one degree of need might be applicable at the same time
here. There is no hierarchy; people may attempt to meet their own development
needs, but not all relatedness needs are met.iii. McClelland’s needs
David McClelland proposed a motivational model that divided demands into three
categories: achievement, affiliation, and power. He claimed that numerous motives
govern an individual’s conduct at any given time. However, in most instances, one
or two motives predominate, and motivation varies according to the demands.Need for Achievement: People who have a high need for achievement want to
succeed, thus they favor moderate risks. They select those tasks in which they
can take personal responsibility for solving issues. Achievers need feedback on a
frequent basis to keep track of their development. High performers should be given
demanding projects with reachable goals by management.Need for Affiliation: Those with a strong need for affiliation seek out positive
interactions with others and want to be accepted by them. Companionship and
mutual aid are important to such persons. Individuals with a high level of affiliation
seek jobs that allow them to contact with others on a regular basis. They have a
tendency to follow the conventions of their workplace. Managers should establish
an environment that fosters supportive interpersonal relationships for persons
seeking affiliation, as this type of group formation leads to goal achievement.Need for Power: The desire to influence people expresses the yearning for power.
People that are looking for power are often vocal and strong. They are prepared to
engage in a fight. There are two forms of power needs: personal and institutional.
Those who crave personal power want to command others, and this desire is
frequently viewed as bad. People who need institutional power desire to oversee
other people’s efforts to achieve the organization’s goals. It has been observed that
managers who have a strong desire for institutional power are more effective than
those who have a strong desire for personal power.iv. Herzberg’s two-factor theory
Frederick Herzberg developed motivation-hygiene theory on the basis of studies to
understand the factors affecting satisfaction or dissatisfaction in a work environment.
These factors have been classified as motivators and hygiene factors respectively.Hygiene Factors: These are the basic factors in a job and also known as extrinsic
factors. Although, they may not provide positive satisfaction but absence of these
factors lead to dissatisfaction. Examples of hygiene factors include status, job
security, salary and fringe benefits.Motivators: These are internal elements that contribute to job happiness. Intrinsic
factors are what they’re termed. The absence of these elements may not lead to
discontent, but their presence in the workplace does. Job challenge, advancement,
autonomy, and responsibility are examples of motivators.b. Process Theories
Process theories concentrate on “how” part of motivation. They describe and
analyze how behavior is energized, directed and sustained. The theories under
process theories are discussed as follows:i. Expectancy Theory
Vroom’s theory of motivation suggests that individuals are motivated towards
objectives if they think that their performance will be rewarded for the efforts they
put in. Vroom suggested three variables in this study Expectancy, Instrumentality
and Valence.
Expectancy: Effort lead to performance
Instrumentality: Performance lead to outcome
Valence is the importance associated by an individual with respect to the
expected outcome. It is an expected and not the actual satisfaction that an
employee expects to receive after achieving the goals. This is dependent
on individuals’ needs, values, goals, preferences and source of motivation.ii. Equity Theory
The equity concept was suggested by J.S. Adams. According to this theory,
employees have high expectations of justice, balance, and fairness in their treatment
by their employers. In this viewpoint, people are motivated by a desire to be treated
equally at work.Inputs: These are the quality and quantity of an employee’s contributions to the
workplace like: time, effort, loyalty, hard work, commitment, ability, adaptability,
flexibility, tolerance, determination, excitement, management trust, coworker
support, and skills are among them.Outputs: The positive and negative outcomes that an individual obtains after putting
inputs into an activity are referred to as outputs. They can exist in both tangible and
immaterial forms. Job security, esteem, remuneration, employee benefits, acclaim,
and recognition are examples of outputs.c. Reinforcement Theory
Reinforcement theory is based upon “law of effect” Individuals tend to repeat
behavior which is rewarded while the behaviour which gives punishment is not
repeated. Today managers focus on positive rewards to elicit desirable behaviour.d. Behavioral Theories
Behavioral is described as the way a person conducts themselves towards others.
When workers are treated as humans rather than machines, they take action to their
particular work situation in a constructive way by increasing individual productivity.
Thus, in lines of understanding and improving the human behavior, McGregor and
William Ouchi suggested Theory X and Y and Theory Z respectively.i. McGregor’s Theory X and Theory Y
McGregor has suggested two contrasting theories on motivation based on certain
assumptions1. Theory X
Theory X revolves around the traditional approach to motivation and control.
It represents traditional stereotyped and authoritarian management style. It has
following assumptions:
An average human being is lazy and doesn’t like to work. He will avoid work
if he can
Most human beings lack ambition and thus don’t want responsibility. They
prefer to be directed rather than to lead.
Most human beings are self-centred and indifferent to the organizational
goals.
Most people are not creative to solve organizational problems.
Most human beings are motivated with physiological and safety needsThese assumptions suggest that the human beings can be motivated by money
and the benefits required for satisfying the physical and safety needs. According
to the theory, the employees are managed by punishments and strict control. This
type of motivational process can only work in the environment whereby the work is
repetitive in nature and promotions are not frequent. McGregor advocated Theory
Y refuting the assumptions of Theory X as nowadays the employees don’t just get
motivated with money and related benefits2. Theory Y
Theory Y assumes that people are not unreliable and lazy by nature. It has a positive
view on employee motivation and their behavior. The management undertakes the
responsibility of helping the employees to develop and express their creative skills.
The assumptions of McGregor’s Theory Y are as follows:
Fundamental of Nursing | Associate Nursing Program | Senior 4410
An average person doesn’t dislike work rather work is natural as play.
An average human being will exert self-control and direct himself for his
objectives.
An average individual knows that he will be rewarded if he is committed for
the objectives. And generally these rewards are higher order needs namely
ego satisfaction and self-actualization.
An average person tends to seek responsibility and is ambitious.
Imagination, creativity, and ingenuity can be used to solve work problems
most of the people.
Considering the present scenario of present industrial life, the intellectual
potential of an average man is only partly utilized. Theory Y is more real
and generally used in the organizations. In support of this theory, McGregor
suggested motivational practices like decentralization, delegation, job
enlargement, participation and consultative managementSelf-assessment 9.7.
1) Maslow’s hierarchy of needs includes all of the following except:
a) Physiological
b) Safety
c) cognition
d) Esteem2) In Maslow’s hierarchy of needs, food, water and sleep are considered
______________________motives.
a) Safety
b) Self-actualization
c) Physiological
d) Esteem3) In Maslow’s theory of motivation, social needs are satisfied by ….
a) Job security
b) Food and water
c) Love and friendliness
d) Job responsibility4) Explain the factors affecting satisfaction or dissatisfaction in a work
environment developed by Herzberg5) List the motivation models proposed by David McClelland
6) Describe the needs developed by Alderfer’s ERG
End unit assessment 9.
Question one and two are True and false questions
1) An optimist believes that the best possible outcome will occur and hopes
for it even if it is unlikely.2) The qualities of pessimistic people are self-motivated, they surround
themselves with other people with the same qualities.
Multiple choice questions3) According to Freud, which part of our personality is the moral part that
develops due to the moral and ethical restraints placed on us by our
caregivers?
a) Id
b) Ego
c) Superego
d) No answer4) Which of the following is not one of the big personality traits?
a) Open to new experiences
b) Agreeableness
c) Locus of control
d) Neuroticism5) Which of the following are considered tenants of personality according
to trait theorists?
a) There are only 5 personality trait, people are born with and retain
the same traits throughout their life and they are entirely based on
nature
b) Traits are relatively stable over time, traits influence behavior
c) Traits change based on situation and exposure, trait are affected by
behavior and they do not affect each other (friendly and unfriendly
at once)
d) Traits can be used to predict a person’s behavior and all people
have the same definable traits6) According to Freud, displacement, sublimation and projection are all
types of what?
a) Behavior need
b) Defense mechanism
c) Behavior change
d) Psychosocial stage7) In Freud’s topographic model, the ‘çensor’ guards the border between
…
a) The Conscious and the Preconscious
b) The Preconscious and the Unconscious
c) The Conscious and the Unconscious
d) The Ego and the Id8) Considering six stages of behavior change. A person who does not
regularly exercise makes a plan to exercise in the upcoming month. He
schedules an appointment to speak with his healthcare provider. Which
stage of stages of behavior change does this best describe?
a) Pre contemplation
b) Contemplation
c) Preparation
d) Action9) Maslow’s hierarchy of needs includes all of the following except:
a) Physiological
b) Safety
c) cognition
d) Esteem10) M. is friendly, always willing to help others and compassionate. We
would expect Lana to score highly on:
a) Extraversion
b) Agreeableness
c) Neuroticism
d) Openness to experience11) John is self-disciplined, focused on achievement and keen to do his
duty. He would be expected to score highly on:
a) Neuroticism
b) Agreeableness
c) Extraversion
d) Conscientiousness12) Which of the following is not an overt behaviour?
a) Dreaming
b) Walking
c) Laughing
d) FightingOpen questions
13) State 4 determinants of human behavior
14) List the types of defence mechanism
15) Explain what good personality meant?UNIT 10: SOCIOLOGY OF HEALTH AND ILLNESS
Key unit competence:
Explain the concepts of sociology in health promotion and wellbeing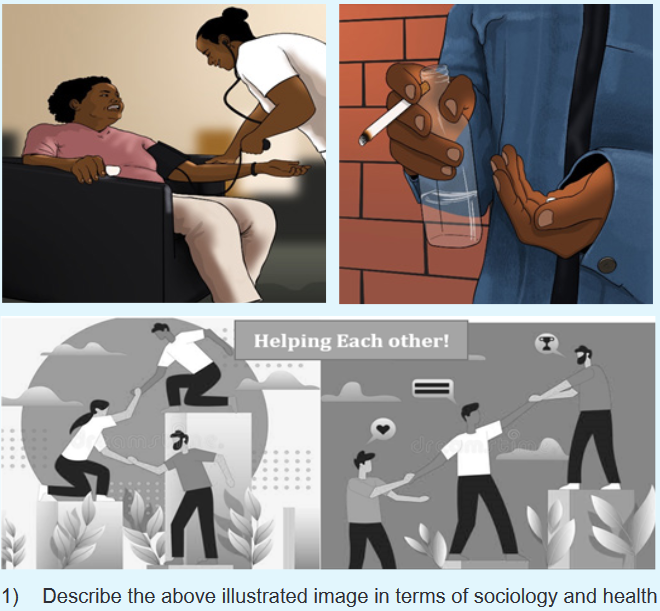
10.1. Definition and characteristics of sociology
Learning activity 10.1.
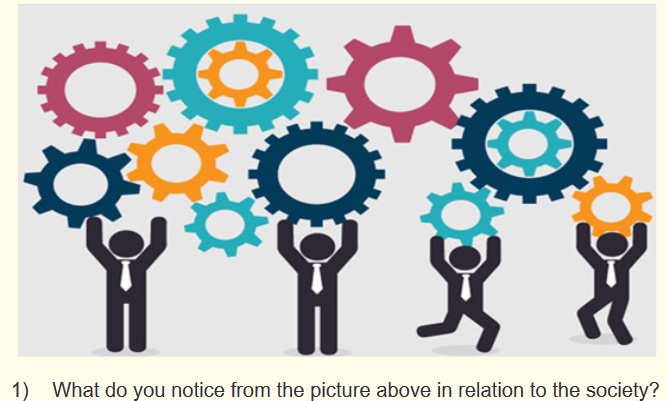
Sociology is a study of social facts, which are ways of acting, feeling and thinking
common to a society which coerce individuals in that society to conform. Sociological
knowledge enables us to look at society and human relationships in a certain way
and to understand, explain and make predictions about members of that society.
The broad statement that sociology is the study of society can be refined by more
specific definitions such as ‘the scientific study of human society through the
investigation of the social behavior of man.Sociology is the youngest among the Social Sciences. The term “Sociology” is
derived from Latin word “Socius” means ‘Companion’ or ‘Associate’ and Greek word
“LOGOS” means ‘Science’ or ‘Study of Society’. Thus the etymological meaning of
the term Sociology is “Study of Society”. The nature and characteristics of sociology
can be summarized in the following way:1. Sociology is an independent science
Sociology is not treated and studied as a branch of any other science like philosophy
or political philosophy. As an independent science, it has its own field of study,
boundary and method of approach.2. Sociology is a Social Science and not a physical Science
Sociology belongs to the Social Science and not to Physical Science. As a social
science, it concentrates its attention on man, his Social behavior, Social Activities,
and Social life. It is intimately related to other social Sciences like Anthropology,
Political Science, Economics, Psychology, etc.3. Sociology is a categorical and not a Normative Discipline
Sociology Studies things “as it is” and not “as they ought to be”. As a Science,
Sociology is necessarily silent about the questions of value. It does not make any
kind of value-judgements. Its approaches neither moral nor immoral but amoral. It
is ethically neutral. It cannot decide the directions in which Sociology ought to go.4. Sociology is a pure science and not an Applied science
Sociology is a pure Science because the immediate aim of Sociology is the
acquisition of knowledge. On the contrary an applied science is interested in the
application or utilization of that knowledge. Sociologists never determine questions
of public policy and do not recommend legislators what laws should be passed
or repealed. But the knowledge acquired by a Sociologist is of great help to the
administrator, legislators, diplomats, teachers, social workers, and citizens.5. Sociology is relatively an abstract science and not a concrete science
Sociology does not confine itself to the study of particular or concrete instances of
human events. But it studies the abstract forms of human events and their patterns.
For example, it does not limit itself to the study of any particular war or revolution.
On the contrary, it deals with them in a general or abstract manner, as social
phenomena, i.e., as types of Social conflict. In a similar manner, it makes such
generalized Studies of marriage, religion, family, group, etc.6. Sociology is a Generalizing and not a particularizing science
Sociology tries to make generalizations on the basis of the study of some selected
events. For example, a sociologist makes generalizations on the following:
Joint families are more stable than the nuclear families.
Social changes tale place with greater rapidity in urban communities than in
tribal or rural communities.7. Sociology is a General Social science and not a Special Social Science
The area of inquiry of Sociology is general and not specialized. It is concerned with
human activities whether they are political, economic, religious, social, etc., in a
general way.8. Sociology is both an Empirical and a Rational Science
Sociology is an empirical science because, it emphasizes the facts that result from
observation and experimentation, it rests on trial, or experiment or experience. It is
a rational Science because it stresses that role of reasoning and logical inferences.
An empiricist collects facts where as a rationalist co-ordinates and arranges them.
All modern science including Sociology avail themselves of both empirical and
rational resources.Self-assessment 10.1.
1) Define sociology.
2) Describe the characteristics of sociology10.2. Definition of health and illness in social context
Learning activity 10.2.
Case: A father went in a vacation with his family; in their way, they meet with a
disabled person who was begging for money. In their discussion, the disabled
person tells them that he lost his arm in a car accident which happened when he
was still young. He said that he was very hungry and that his survival depends
on humanitarians who have him something. The father gave him money and
left. In their car the child asks his parent this question “why does that man
survival depend on begging? Losing one arms means that he is ineligible to do
anything? In your groups debate on these two questionHealth is a physiological and a psychological state but it is also, fundamentally, a
social state. The human being make sense of health and illness by drawing on a
stock of current social belief, ideas and practices. In the process of social learning;
humans start to interpret and discuss the social world since infancy. The educational
institution helps people to understand ‘what health is’ and is not, and what are
appropriate responses to disease and illness. In encounters with the structures of
power in society, people learn what it means to be ‘sick’, ‘dependent’ or ‘disabled’.
As they come into contact with organisations which provide health services they
develop their understanding of how to be a ‘patient’ or a ‘career’.Medical sociologists use social constructionist theory to explain health and illness.
In medical profession, disease is a biological condition. Referring to the social
constructionist theory, illness is the social meaning of that condition. In social constructionist theory, impairment refers to a physical illness or
injury; disability is the social experience of impairment.
Illness can reshape an individual’s identity. For example, deafness can be a
cultural identity that replaces individual identity.
Medicalization—the act of reducing illness to strictly a medical definition
ignores the social context of disease.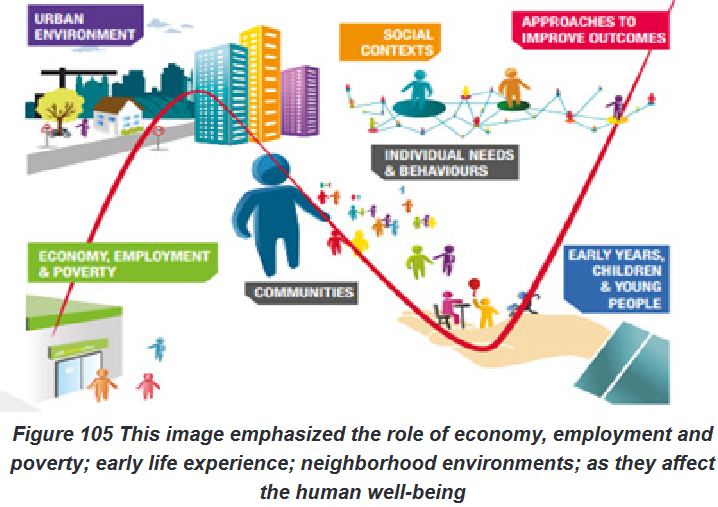
Self-assessment 10.2.
1) Match the terms in column A with their specific definition or examples
in column B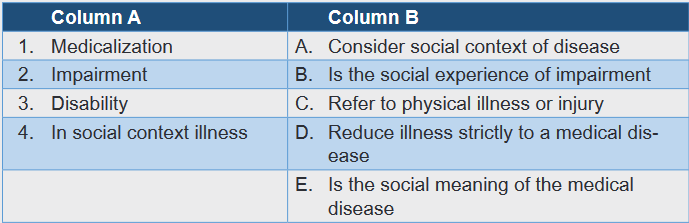
10.3. Biomedical model and holistic approach toward
healthLearning activity 10.3.
Search online books about model of health and with example explain the
following terms
1) Bio-chemical model of health
2) Holistic approach of health10.3.1. Introduction
A positive view of health is maintaining and achieving a balanced diet and a healthy
lifestyle. the individual may regard running and walking in a positive view or taking
supplements for mental and physical well-being. Generally feeling good within is a
good indicator of good health. However, obsession toward having positive view of
health can have its consequences physically and mentally. For example, physical
activity can become unhealthy when it’s taken to extreme measures. People
normally start off at a moderate pace to stay healthy but slowly become obsessed
with fitness and health. This compulsive behaviour could lead to heart and arteries
been damage due to excessive training and consequently to heart attack.A negative view on health is believing you don’t have to go to the local General
practitioner because you feel ok within yourself. Due to not seeing any physical
evidence or symptoms of illness such as blood and vomiting, they automatically
assume they are healthy. Individuals like this regard good health as normal and
they do the minimum to maintain their health. The problem with the negative attitude
towards health is it puts the individual at a huge disadvantage regarding their own
health as certain diseases may only show physical symptoms when the disease
may become untreatable, such as pancreatic cancer and heart disease. These
individuals tend to live a shorter life than the general population, as they don’t act
upon changes in their health or physical well –being.10.3.2. The Biomedical Model of health
The Biomedical model is a scientific method used by clinicians and other health
professionals. It treats the human body as a very complex device and advocates the
treatment of symptoms through the use of medical intervention. The main objective
of the biomedical model is to focus on the human body solely and treat the illness
and diseases separate from the mind.a. Advantage of biomedical model of health
It has a high success rate regarding research and diagnosis of humans.
Depending on the illness, the model can be used to learn about the disease
and avoid it recurring.
The model states health can be restored through treatment and a variety of
techniques including nuclear medication and drugs.Example, if you fracture your leg you can have surgery which will allow you to walk
again. Many illnesses can be treated through medical intervention and advance
research. At the beginning of the 20th century, the leading causes of death were
tuberculosis, pneumonia, influenza and diarrhea. The biomedical model was used
to rule out the cause and influence treatment.b. Disadvantage of Biomedical model of health
The biomedical model fails to include other factors like psychosocial that
are sometimes found to be the main influences of illness.
The model fails to address any illness or disease which doesn’t display any
physical signs and symptoms.Criticizing the model, Foucault (1973) states that Doctors who use this model see
their patients like robots in need of repair. He then suggested that due to medicine
and science, doctors are solely focused on the function and structure of the human
body and they don’t consider any other factors which may contribute to illnesses
such as poverty, stress and poor housing.10.3.3. The Holistic approach of health
The Holistic Model of health focuses on the whole person instead of specific parts
of the body like the biomedical model. Many Holistic Doctors believe all parts of the
human body work in sync with one another. Meaning that if one part of the body,
isn’t working properly then the rest of the body doesn’t work. The main objective
of the holistic Doctor is not to solely examine the body but to understand why it is
happening.c. Advantage of holistic approach of health
The Holistic approach takes into consideration the whole person including
their psychological and emotional health.
The holistic approach allows alternative. Alternative medication is a
treatment which is alternative to mainstream medication. Example herbal
medicine which uses herbs and plants as an alternative.
Yoga and massage are aspects of holistic model and these have proven to
reduce stressd. Disadvantage of holistic approach of health
For people who has serious medical illness like cancer, time spent looking for other
treatments can cause the disease to spread which could lead to the disease to
become untreatable. Holistic drugs don’t always reveal the true ingredients on the
packaging, so you could take a holistic medication which may have a contraindication
when taking conventional medication.Self-assessment 10.3.
1) Differentiate biomedical model of health from holistic approach of health
10.4. Sociology and nursing practices
Learning activity 10.4.

1) Discuss the concepts of sociology and effect on nursing practice
The relevance of sociology to nursing
In 1991, the World Health Organization (WHO) proposed that nurses should
be required to develop and perform functions related to the promotion and
maintenance of health as well as disease prevention and rehabilitation. Nurses
need to be aware of the physical, psychological, social and spiritual aspects of
health, illness, disability and dying. Nursing models developed in nursing havebeen influenced by the social and biological sciences and are intended to help
raise standards of nursing care. Sociology may help nurses to achieve their primary
objective of caring for patients in four ways: (i) implications of changing patterns of
disease, dependency and death; (ii) social and cultural variations in perceptions of,
and responses to, pain and diseases; (iii) organizational analyses, with particular
reference to the importance of nurse-patient communication and; (iv) sociological
studies on interpersonal relationshipsSelf-assessment 10.4.
1) Explain the ways by which sociology may help nurses to achieve their
objective10.5. Determinants of health
Learning activity 10.5.
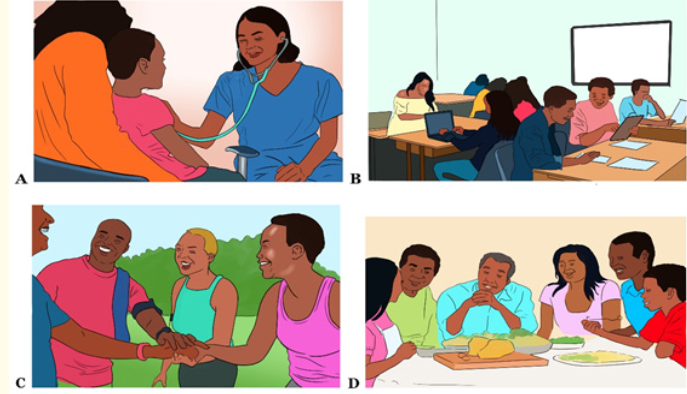
Observe the pictures above and answer the following questions:
1) What do you see on pictures A, B, C, and D?
2) According to your point of view, what might be the relation between: (a).
people’s access to health services and their own health; (b). education
access and health status; (c). Social circumstance and health status;
(d). Income status and health status?10.5.1. Introduction to determinants of health
Many factors combine together to affect the health of individuals and communities.
Whether people are healthy or not, is determined by their circumstances and
environment. To a large extent, factors such as where we live, the state of our
environment, genetics, our income and education level, and our relationships with
friends and family all have considerable impacts on health, whereas the more
commonly considered factors such as access and use of health care services often
have less of an impact.The determinants of health include:
The social and economic environment,
The physical environment, and
The person’s individual characteristics and behaviours.The context of people’s lives determines their health, and so blaming individuals
for having poor health or crediting them for good health is inappropriate. Individuals
are unlikely to be able to directly control many of the determinants of health. These
determinants—or things that make people healthy or not—include the above
factors, and many others:
Income and social status - higher income and social status are linked to
better health. The greater the gap between the richest and poorest people,
the greater the differences in health.
Education – low education levels are linked with poor health, more stress
and lower self-confidence.
Physical environment – safe water and clean air, healthy workplaces, safe
houses, communities and roads all contribute to good health.
Employment and working conditions – people in employment are healthier,
particularly those who have more control over their working conditions
Social support networks – greater support from families, friends and
communities is linked to better health. Culture - customs and traditions, and
the beliefs of the family and community all affect health.
Genetics - inheritance plays a part in determining lifespan, healthiness and
the likelihood of developing certain illnesses.
Personal behaviour and coping skills – balanced eating, keeping active,
smoking, drinking, and how we deal with life’s stresses and challenges all
affect health.
Health services - access and use of services that prevent and treat disease
influences health Gender - Men and women suffer from different types of diseases at different
ages.10.5.2. Social determinants of health
Social determinants of health (SDOH) are conditions in the places where people
live, learn, work, and play that affect a wide range of health risks and outcomes.
The World Health Organization also provides a definition of social determinants of
health. Social determinants of health as the conditions in which people are born,
grow, live, work and age. These circumstances are shaped by the distribution
of money, power, and resources at global, national, and local levels. The social
determinants of health are mostly responsible for health inequities – the unfair and
avoidable differences in health status seen within and between countries. Healthy
People 2030 use a place-based framework that outlines five key areas of SDOH:a. Health care access and quality
There is connection between people’s access to and understanding of health
services and their own health. This domain includes key issues such as access to
healthcare, access to primary care, health insurance coverage, and health literacy.b. Education access and quality
There is connection of education to health and wellbeing. This domain includes
key issues such as graduating from high school, enrolment in higher education,
educational attainment in general, language and literacy, and early childhood
education and development.c. Social and community context:
There is connection between characteristics of the contexts within which people
live, learn, work, and play, and their health and wellbeing. This includes topics like
cohesion within a community, civic participation, discrimination, conditions in the
workplace, and incarceration.d. Economic stability
There is connection between the financial resources people have – income, cost of
living, and socioeconomic status – and their health. This area includes key issues
such as poverty, employment, food security, and housing stability.e. Neighborhood and built environment
There is connection between where a person lives – housing, neighborhood, and
environment – and their health and wellbeing. This includes topics like quality of
housing, access to transportation, availability of healthy foods, air and water quality,
and neighbourhood crime and violence.10.5.3. Addressing social determinants of health
Resources that enhance quality of life can have a significant influence on population
health outcomes. Examples of these resources include safe and affordable housing,
access to education, public safety, availability of healthy foods, local emergency/
health services, and environments free of life-threatening toxins. We also know
that poverty limits access to healthy foods and safe neighbourhoods and that
more education is a predictor of better health. Differences in health are striking
in communities with poor SDOH such as unstable housing, low income, unsafe
neighbourhoods, or substandard education. By applying what we know about
SDOH, we can not only improve individual and population health but also advance
health equity.Self-assessment 10.5.
1) Outline any 4 determinants of health
2) 2.Explain how the following factors can have an influence on population
health
a) Income and social status
b) Physical environment
c) Employment and working conditions
d) Social support networks
e) Genetics
f) Personal behavior
g) Gender10.6. Religion, culture, social norms, beliefs, values,
customs, practice and implications to healthLearning activity

1) Discuss about the following topics
a) Religion and its importance in mental health
b) Culture and cultural perception
c) Types of norms
d) Importance of values10.6.1. Religion and implications to health
Religious practice substantially contributes to physical and mental health. Regular
religious practice lessens depression, promotes self-esteem, and builds familial
and marital happiness. Religious worship also increases longevity, improves an
individual’s chances of recovering from illness, and lessens the incidence of many
diseases.Theory and literature suggests that the reasons religiously involved people tend to
have good health outcomes are because they have healthy lifestyles and behaviors
in accord with religious beliefs. Other literature suggests that religious involvement
may play a negative role in health outcomes due to beliefs about illness originating
as punishment for sins.Good mental health is highly correlated to religious participation. An increase in
religious practice was associated with having greater hope and a greater sense of
purpose in life. Religious affiliation and regular church attendance were among the
most common reasons people gave to explain their own happiness. Happiness was
greater and psychological health was better among those who attended religious
services regularly.More frequent attendance at religious services predicted less distress among
adults. Membership in a religious community can enhance coping skills. One study
found that people were much more inclined to use positive coping responses when
they received spiritual support from fellow church members.10.6.2. Culture and implications to health
a. Definition
Culture refers to a set of the ideas, customs, and social behavior of a particular
people or society. Culture involves how a person lives, speaks, interacts with others
and what individuals create, but perception considers how that individual sees the
world, or what happens when these two concepts are combined into a single phrase.
Cultural perception is how people gather information, learned within their specific
culture, to inform themselves about their world. This takes into account all aspects
of the individual’s life. How a person sees art, language, religion, etc. is all informed
by how those elements of the world are seen within the context of their cultureb. Elements of culture
i. Values
Values are a culture’s standard for discerning what is good and just in society.
Values are deeply embedded and critical for transmitting and teaching a culture’s
beliefs. Values help shape a society by suggesting what is good and bad, beautiful
and ugly, sought or avoided.ii. Beliefs
Beliefs are the tenets or convictions that people hold to be true. Individuals in a
society have specific beliefs, but they also share collective values.iii. Norms
Norms define how to behave in accordance with what a society has defined as
good, right, and important, and most members of the society adhere to them.
Formal norms are established, written rules. They are behaviors worked out andagreed upon in order to suit and serve the most people. Informal norms are casual
behaviors to which an individual generally conforms.iv. Symbols
Symbols are gestures, signs, objects, signals, and words that help people
understand their surrounding world.v. Language
Language is the principal method of human communication, consisting of words
used in a structured and conventional way and conveyed by speech, writing, or
gesture. Language is considered as a system of communication used by a particular
country or community.c. Culture influence to health
Culture influences healthcare at all levels, including communications and
interactions with doctors and nurses, health disparities, health care outcomes, and
even the illness experience itself. People in some cultures believe illness is the will
of a higher power, and may be more reluctant to receive health care.A culture of Health is broadly defined as one in which good health and well-being
flourish across geographic, demographic, and social sectors; fostering healthy
equitable communities guides public and private decision making; and everyone
has the opportunity to make choices that lead to healthy lifestylesSelf-assessment 10.6
1) Discuss about the following 4 topics
a) Religion and positive implication to health
b) Culture and negative implication to health
c) Social norms and positive implication to health
d) Values and negative implication to health10.7. Health beliefs and practices and their influence on
health, health promotion and illness preventionLearning activity 10.7.

In groups, discuss about the followings:
1) Health beliefs
2) Health practices
3) Health promotion10.7.1. Health in social context
Health is determined by the conditions in which we live our everyday lives. Those
conditions include the social, cultural, economic, educational, and occupational as
well as the physical and mental environment, which influence health behavior and
lifestyle and so the health status. Health beliefs are the tenets or convictions that
people hold to be true regarding health promotion.10.7.2. Illness
Illness is defined as the ill health the person identifies themselves with, often based
on self -reported mental or physical symptoms. In some cases, this may mean only
minor or temporary problems, but in other cases self - reported illness might include
severe health problems or acute suffering.10.7.3. Health promotion
Health promotion is the process of enabling people to exert control over the
determinants of health and thereby improve their health. It moves beyond a focus on
individual behavior towards a wide range of social and environmental interventions.Health beliefs and practices and influence on health promotion and illness prevention
Health beliefs are what people believe about their health, what they think constitutes
their health, they are also what they consider the cause of their illness, and ways
to overcome an illness. Healthy practices mean the actions intending for “first do
not harm”. Healthy practices mean to teach or advise patients to use their own non-
specific mechanisms of defense to promote health and prevent illness in order to
live a healthy life.People will not change their health behaviors unless they believe that they are
at risk. Example: Individuals who do not think they will get the sexual transmitted
disease are less likely to use condom during sex intercourse. People who think they
are unlikely to get malaria are less likely to sleep under mosquito netSelf-assessment 10.7.
1) “Health is determined by the conditions in which we live our everyday
lives” basing on this statement list four conditions in which we live that
determine our health?
2) Explain how health beliefs influence health promotion?10.8. Health enhancing versus risk-taking behaviors;
smoking, alcohol abuse, drugs and other
substance abuseLearning activity 10.8.

In groups, Discuss about the following topics
1) Smoking and health
2) Alcohol abuse and health
3) Drugs/substances abuse and healthWhile adults almost always view risk-taking in negative terms, not all risk-taking is
dangerous or detrimental to a young person’s health. In fact, a degree of risk-taking
is essential for personal growth and development: it allows a young person to test
their limits, learn new skills, develop competence and self-worth, and assume
greater responsibility for their lifeFor some young people, risk-taking is a way of resolving developmental challenges
(for example, a young male who drinks heavily to prove that he is as grown-up
as his peers). For others, risk-taking may be a way of dealing with problems or
escaping unhappy situations or feelings (such as a young woman who engages in
sexual activity in response to her low self-esteem and feelings of worthlessness, or
her experience of sexual assault). While risk-taking behavior can constitute a major
health problem in itself, it may also be an indicator of an underlying problem in the
young person’s life. Angry, acting-out behaviour can mask depression, or it may
reflect the young person’s experience of violence. Risk-taking behaviours which
can have serious negative implications for young people’s health include: Early and/or high risk sexual activity
Drink driving
Substance or alcohol abuse
Running away from home
Dropping out of school
Criminal activity
Severe dieting
Dissociation
Suicidal thoughts and talk
Self-harm
Assaulting others10.8.1. Smoking
Nicotine is a highly addictive chemical found in the tobacco plant. The addiction
is physical, meaning habitual users come to crave the chemical, and also mental,
meaning users consciously desire nicotine’s effects. Nicotine addiction is also
behavioural. People become dependent on actions involved with using tobacco.10.8.2. Alcohol abuse
Alcohol abuse or alcohol use disorder is a condition in which a person continues to
consume alcohol despite the adverse consequences.10.8.3. Drug abuse
Drug abuse is the use of illegal drugs or the use of prescription or over-the-
counter medications in ways other than recommended or intended. It also includes
intentional inhalation of household or industrial chemicals for their mind altering
effects.10.8.4. Health enhancement versus risk taking behaviours
Drug addiction and other risk taking behaviour have been termed as a disease
because their effects cause permanent changes in the dopamine reward pathway
of the brain leading to compulsive use even after the initial pleasurable effect of the
drug has warm off. Therefore, the repetitive use of the drug leads to craving and
withdrawal symptoms which lead to continuation and maintenance of drug abuseSelf-assessment 10.8.
1) What is nicotine and its effects in human body
2) Explain drug abuse in few words?
3) Why is drug addiction considered as disease?End unit assessment 10.
From question 1 to 5; select the best answer
1) The term socious derived from which language?
a) German
b) Greek
c) Latin
d) Roman2) Which are the words composing the term sociology
a) Society and community
b) Socious and Logos
c) Society and Science
d) Socious and science3) Which among the following is a youngest science?
a) History
b) Sociology
c) Geography
d) Philosophy4) In biomedical model of health a ‘sick’ organ is best described as being:
a) Depressed
b) Unwell
c) Ill
d) Diseased5) Which of these is an assumption of the biomedical model?
i. All illness has one underlying cause.
ii. Disease is always that single cause.
iii. Stopping, removing, or minimizing the disease will return a person
to good health.
a) II only
b) I only
c) I, II
d) I, II, III1) Match terms in column A with their specific definition or example in column
B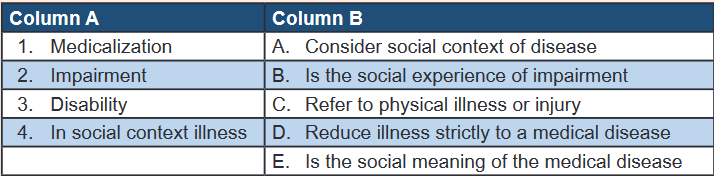
Differentiate the biomedical model of health and the holistic approach of health?
2) How can sociology impact nurses to achieve their primary objective of
caring?
3) Describe the implication of Religion to health
4) With example describe how negative health believes can negatively
influence health promotion and illness preventionREFERENCES
• Burton, M. A., & Ludwig, L. J. M. (2015). Fundamentals of Nursing Care:
Concepts, Connections & Skills (2nd Editio). F. A. Davis Company. Philadelphia.
• Erb, K., Snyder, B., Buck, F., & Yiu, F. (2018). Fundamentals of Canadian
Nursing: Concepts, Process, and Practice (Fourth Can). Pearson Canada Inc.
• Kozier & Erb’s. (2018). Fundamentals of Nursing: Concepts, Process and
Practice (Fourth Edi). Pearson Australia.
• Lynn, P. (2011). Taylor’s Clinical Nursing Skills: A Nursing Process Approach
(Third Edit). Wolters Kluwer Health| Lippincott Williams & Wilkins.
• Perry. A.G, Potter. P.A, O. W. . (2014). Clinical Nursing Skills & Techniques (8th
Editio). Elsevier.
• Potter, P.A, Perry,A.G, Stockert, P.A, & Hall, A. . (2019). Essentials for Nursing
Practice (Ninth Edit). Elsevier Inc.
• Wilkinson, J.M, Treas, L.S, Barnett, K.L, Smith, M. . (2016). Fundamentals
of Nursing: Theory, Concepts, and Applications. F. A. Davis Company.
Philadelphia.
• Craven et al., 2013; McKenna et al., 2014; Nair & Peate, 2013; Narwal &
Gangadharan, 2017; Potter et al., 2020; Snyder et al., 2018; Wilkinson et al.,
2016)(Chilton & Bain, 2018)
• Chilton, S., & Bain, H. (Eds.). (2018). A Textbook of Community Nursing (2nd
Ed). Routledge.
• Craven, R. F., Hirnle, C. J., & Jensen, S. (2013). Procedure checklists for
Fundamentals of Nursing Human Health and Function (7th Ed). Lippincott
Williams & Wilkins.
• McKenna, H. P., Pajnkihar, M., & Murphy, F. A. (2014). Fundamentals of
Nursing Models, Theories and Practice. In Wiley E-Text (2nd Ed, Vol. 8, Issue
3). John Wiley and Sons Ltd.
• Nair, M., & Peate, I. (Eds.). (2013). Fundamentals of Applied Pathophysiology
An Essential guide for Nursing and Healthcare Students (2nd Ed). John Wiley
and Sons Ltd.
• Narwal, A., & Gangadharan, H. (2017). Fundamentals of Nursing. In Key to
Success Staff Nurses Recruitment Exam (10th Ed, pp. 49–49). Elsevier.
• Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2020). Fundamentals
of Nursing (10th Ed). Elsevier.• Snyder, B., Dwyer, L.-J., Harvey, H., Moxham, L., Parker, L., & Stanley, R.-
S. (2018). Kozier and Erb’s Fundamental of Nursing Concept, Process and
Practice (4th Ed, Vols. 1–3). Pearson Australia Pty Ltd.
• Wilkinson, J. M., Treas, L. S., Barnett, K. L., & Smith, M. H. (2016). Fundamentals
of Nursing: Theory, Concepts, and Applications (3rd Ed). F. A. Davis Company.
• Klainberg, M. (2009). An historical overview of nursing. Today’s nursing leader:
Managing, succeeding, excelling, 21-40. Jones and Bartlett publisher.
• Berman, A., Snyder, S. J., Kozier, B., Erb, G., Levett-Jones, T., Dwyer, T., &
Stanley, D. (2010). Kozier and Erb’s fundamentals of nursing, Fourth Australian
edition (Vol. 1). Pearson Australia.
• Ahtisham, Y., & Jacoline, S. (2015). Integrating Nursing Theory and Process
into Practice; Virginia’s Henderson Need Theory. International Journal of
Caring Sciences, 8(2).
• Berman, A., Snyder, S. J. (2012). Kozier & Erb’s fundamentals of nursing:
concepts, process, and practice, 9th edition.
• Alligood, M.R. (2018). Nursing theorists and their work, 9th edition, Elsevier
Health Sciences.
• C Smith, M., & E Parker, M. (2015). Nursing theories and nursing practice, 3rd edition.
• Talor, C., Lillis, C., & Lemone, P. (2011). Fundamentals of nursing: the art and
science of nursing care, 7th edition, Lippincott Williams & Wilkins.
• Burton, M. A., & Ludwig, L. J. M. (2015). Fundamentals of Nursing Care
Concepts, Connections &Skills.
• Basavanthappa (2009) Fundamentals of Nursing 2nd Edition
• Kasinathan, V (2017) Introduction on route of drug administration. http://www.
medindia.net/patientinfo/routes-of-drug-administration
• Berman, Audrey T.; Snyder, Shirlee; Frandsen, Geralyn (2018). Kozier and
Erb’s Fundamentals of Nursing. Concepts, Process and Practice, fourth
edition, Pearson austrarian group.
• Karch, A. M. (2013). Focus on nursing pharmacology. Philadelphia: Lippincott
Williams & Wilkins.
• Sahoo,c,k. Nayak,P,K. Sarangi,D,K, Tanmaya (2013) Intra Vaginal Drug
Delivery System: An Overview , American Journal of Advanced Drug Delivery.
Osmania University College of Technology, Osmania University Hyderabad,
https://www.imedpub.com/articles/intra-vaginal-drug-delivery-systeman-
overview.pdf retrieved on 11th September 2021.• Haddad, D.(2020)Biological Factors That Influence Child Development
• Barbara M. Newman, Philip R. Newman (2020) Theories of Adolescent
Development
• Cherry,k (2019) Sociocultural Theory of Cognitive Development
• Haddad, D.(2020) Biological Factors That Influence Child Development
• pinikahana, J. (2003). Role of sociology within the nursing enterprise. Nursing
& Health sciences, 175-180.
• Surajkmar. (2020). Define Sociology, describe its characteristics. Sarthaks
eConnect, 1-2.
• World Health Organization (2021). Demographics and Social
Determinants of Health, retrieved on 22 December 2021
from chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/
viewer.html?pdfurl=https%3A%2F%2Fhealth.hamiltontn.
org%2FPortals%2F14%2FDataPublications%2FDocs%2FDemographics.
pdf&clen=1177564&chunk=true
• Center for Diseases control and prevention (2021). Social determinants of
health: Know what affect health, retrieved on 22 December 2021 from https://
www.cdc.gov/socialdeterminants/about.html on 22 December 2021.
• World Health Organization (2017). Determinants of health, retrieved on 22
December 2021 from https://www.who.int/news-room/questions-and-answers/
item/determinants-ofhealth
