UNIT 2: HUMAN REPRODUCTION AND FAMILY PLANNING
Key Unit Competence:
Explain the role of human reproductive hormones,
stages of pregnancy and family planning methods.
Introductory activity 2
Observe the photo below and answer the questions that follow: a) The woman in A is pregnant. What do you think about the origin of the
a) The woman in A is pregnant. What do you think about the origin of the
fetus in the womb of the pregnant woman?
b) Use the photo B to imagine the embryonic development in mother’s
uterus.
c) Use the photo in B and identify the observable parts of the female
reproductive system. Are you satisfy with that description? Justify your
response.
d) The child on the photo is a boy. Can you identify the parts of the male
reproductive system? What represent the gesture of that boy? Are
challenging!!!!e) What do you think about foetus position observed in mother’s uterusAnimals reproduce sexually, but some, on occasion, can reproduce asexually.
on the photo B?
f) The child boy on picture A is the first borne of her mother and the
fetus in the womb will be the second and last borne of this mother.Can you advocate for such a family planning? Give reasons
Sexually reproducing animals have gonads for the production of gametes,
and many have accessory organs for the storage and passage of gametes
into or out of the body. Animals have various means of ensuring fertilization of
gametes and protecting immature stages. Human reproduction is any form of
sexual reproduction resulting in human fertilization. It typically involves sexualintercourse between a man and a woman.
2.1. Human reproductive systems
The diagrams below represent male and female reproductive system.Observe and use them to answer questions that follow.
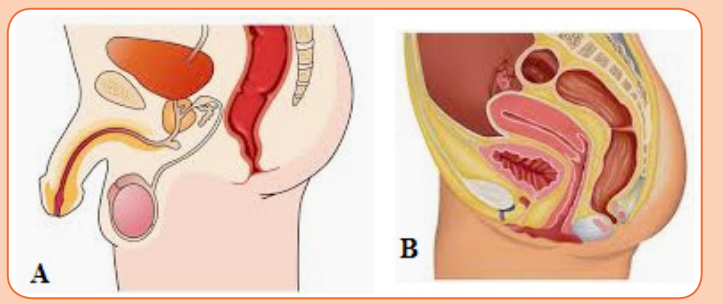 a) Identify the structures representing a male and female human
a) Identify the structures representing a male and female human
reproductive system.
b) Use the choice in (a) to locate and suggest the function of the following
male human reproductive organs on the diagram: testis, epididymis,
vas deferens, seminal vesicles and prostate gland.
c) Use the choice indicating the female human reproductive system
to locate and suggest the function of the following female human
reproductive organs on the diagram: urethra, vagina, uterus, ovariesand oviducts.
Human beings reproduce by sexual means where the male and female involve2.1.1. Structure of male reproductive system
in sexual intercourse, resulting in fertilization. During sexual intercourse, the
interaction between the male and female reproductive systems results in
fertilization of the woman’s ovum by the man’s sperm. The ovum and sperm are
specialized reproductive cells called gametes, generated by a process calledgametogenesis (i.e., spermatogenesis in males and oogenesis in females).
The main visible differences between boys and girls at birth are their reproductive
organs. The sex of a child is determined at the time of fertilization of the ovum by
the spermatozoon. The differences between a male and a female are geneticallydetermined by the chromosomes that each possesses in the nuclei of the cells.
The male gonads are paired testes, which are suspended within the sacs of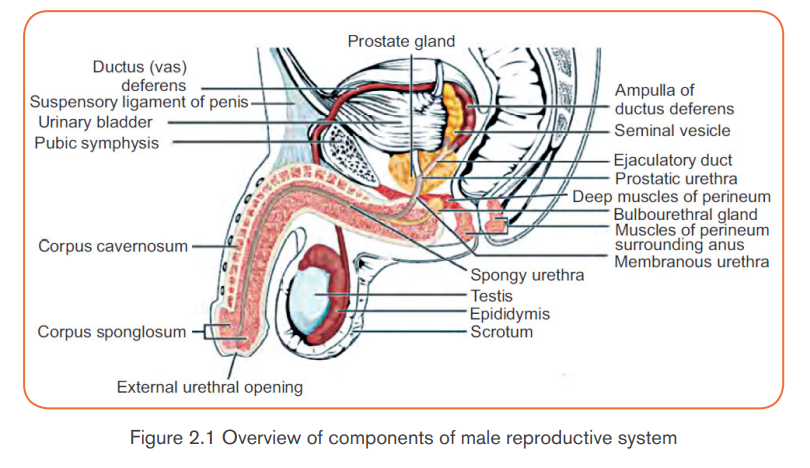
the scrotum. The testes begin their development inside the abdominal cavity,
but they descend into the scrotal sacs as development proceeds. If the testes
do not descend and the male does not receive hormone therapy or undergo
surgery to place the testes in the scrotum results in sterility (the inability to
produce offspring). Sterility occurs because undescended testes developing
in the body cavity are subject to higher body temperatures than those in the
scrotum. A cooler temperature is critical for the normal development of sperm.
Sperm produced in the seminiferous tubules of the testes mature within the
epididymides (sing., epididymis), which are tightly coiled tubules lying just
outside the testes. Maturation seems to be required for the sperm to swim tothe egg.
Once the sperm have matured, they are propelled into the vasa deferentia
(sing., vas deferens) by muscularcontractions. Sperm are stored in both the
epididymides and the vasa deferentia. When a male becomes sexually aroused,
sperm enter the ejaculatory ducts and then the urethra, part of which is locatedwithin the penis.
The penis is the male organ of sexual intercourse. The penis has a long shaft
and an enlarged tip called the glans penis. The glans penis is normally covered
by a layer of skin called the foreskin. Circumcision, the surgical removal of theforeskin, is often done soon after birth.
In addition to these organs, the male reproductive system consists of a series of
ducts and glands. Ducts include the vas deferens and ejaculatory ducts. They
transport sperm from the epididymis to the urethra in the penis.
Glands include the seminal vesicles, prostate gland, and bulbourethral glands
(also called Cowper’s glands). They secrete substances that become part ofsemen.
- Two seminal vesicles contribute about 60% of the volume of semen.
The fluid from the seminal vesicles is thick, yellowish, and alkaline. It
contains mucus, the sugar fructose (which provides most of the sperm’s
energy), a coagulating enzyme, ascorbic acid, and local regulators called
prostaglandins.
- The prostate gland secretes its products directly into the urethra through
several small ducts. This fluid is thin and milky; it contains anticoagulant
enzymes and citrate (a sperm nutrient).
- The bulbourethral glands are a pair of small glands along the urethra below
the prostate. Before ejaculation, they secrete clear mucus that neutralizes
any acidic urine remaining in the urethra. Bulbourethral fluid also carries
some sperm released before ejaculation, which is one reason for the highfailure rate of the withdrawal method of birth control (coitus interruptus).
Semen is the fluid that is ejaculated from the urethra. Semen contains secretions
from the glands as well as sperm. The secretions control pH and provide thesperm with nutrients for energy.
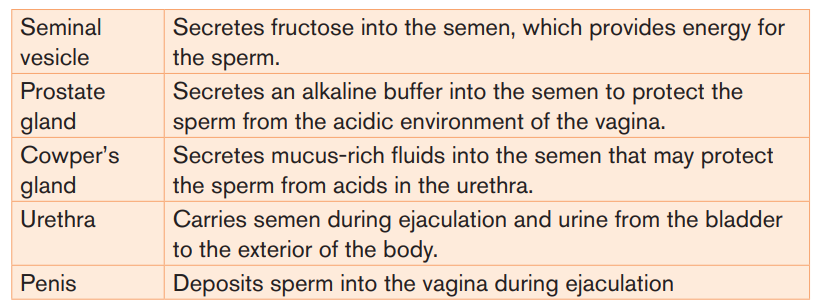
Table 2.1: Parts of the male reproductive system and their functions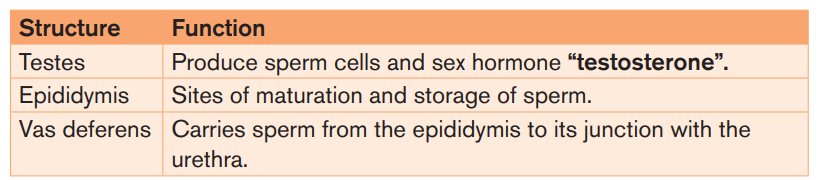
Note: Male infertility refers to a male’s inability to cause pregnancy in a fertile
female. In humans it accounts for 40-50% of infertility. It affects approximately
7% of all man. Male infertility may be due to:- Absence of sperms in the semen (Azoospermia).
- Low sperm count e.g. when ones ejaculate less than 1cm3 of semen.
- Abnormal sperm e.g. sperms with 2 tails, or without tail, or without
acrosomes,
- Auto-immunity e.g. antibodies attack one’s sperms
- Premature ejaculation: the man has orgasm before copulation
- Impotence i.e. inability to achieve or maintain an erection of the penis.2.1.2. Structure of female reproductive system
The female reproductive system is a collection of organs and other structures
located primarily in the pelvic region. Most of the structures are inside the body.
It includes the ovaries, the oviducts, the uterus, and the vagina. The female
reproductive system has several functions:- Producing eggs, which are female gametesDuring puberty, a girl develops into a sexually mature woman, capable of
- Secreting female sex hormones
- Receiving sperm during sexual intercourse
- Supporting the development of a fetus
- Delivering a baby during birthproducing eggs and reproducing.
The external genital organs of a female are known collectively as the vulva. The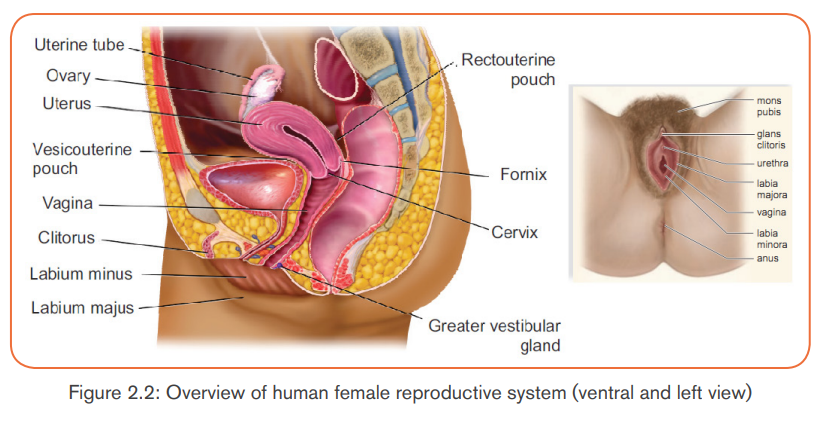
pubic hairs and two folds of skin called labia minora and labia majora are
on either side of the urethral and vaginal openings. Beneath the labia majora,
pea-sized greater vestibular glands (Bartholin glands) open on either side of thevagina. They keep the vulva moist and lubricated during intercourse.
At the juncture of the labia minora is the clitoris, which is homologous to the
penis in males. The clitoris has a shaft of erectile tissue and is capped by a peashaped glans. The many sensory receptors of the clitoris allow it to function
as a sexually sensitive organ. The clitoris has twice as many nerve endings as
the penis. Orgasm in the female is a release of neuromuscular tension in the
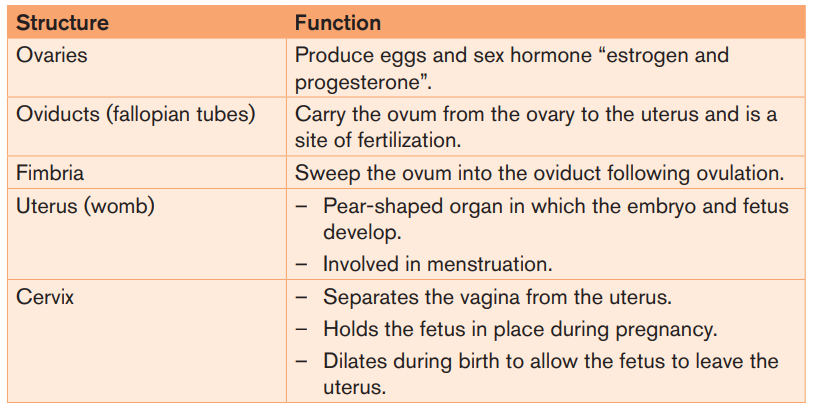
muscles of the genital area, vagina, and uterus.Table 2.2: Parts of the female reproductive system and their functions
Note: Female infertility is defined as the inability to conceive or carry a pregnancy
to term after 12 months of unprotected intercourse, or 6 months of unprotected
intercourse if the female is over 35 years old. In females, infertility may be due
to:- Failure to ovulate due to the lack of some hormones.Application activity 2.1
- Damage of the Fallopian tubes / oviducts, for example the tubes may be
completely blocked by nature or after an infection.
- Damage on the uterus; for example, the endometrium can be destroyed.
- Damage on the cervix, for example the cervix may be narrow or too wide or
may stop producing cervical mucus needed for the sperm to reach uterus.
- Antibodies against sperms, for example, the cervix, the uterus or the oviductof a woman can produce antibodies against her husband’s sperms.
The figure below represents the male reproductive system.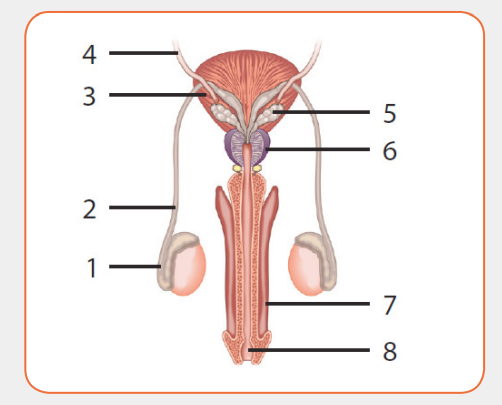
a) Justify why it is representing a male reproductive system.
b) Refer to the figure and identify the parts represented by the numbers
1 to 8.
c) How can you justify the function of organ 2, 5 and 7 according to thestructure of male reproductive system?
2.1.3. Gametogenesis
Activity 2.2
Gametes are haploid cells that are formed from diploid germ cells through
the process of gametogenesis. The significance of developing haploid
gametes lies in the fact that after fertilization, the developing zygote attains
the diploid status back. In this way, the developing embryo gets the single
copy of all the chromosomes from each parent.
Based on the chart diagrams of spermatogenesis and oogenesis shown
below.
i) Compute the number of chromosomes at each stage, assuming 2n= 46.
ii) Which diagram does it represent spermatogenesis and oogenesis?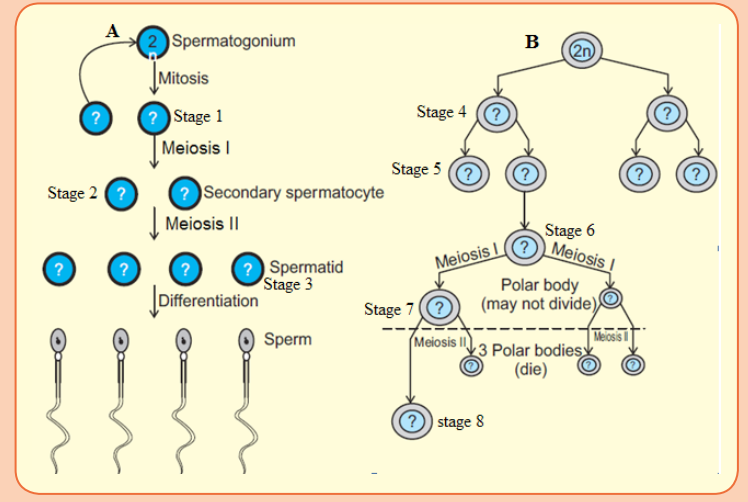
Explain why?
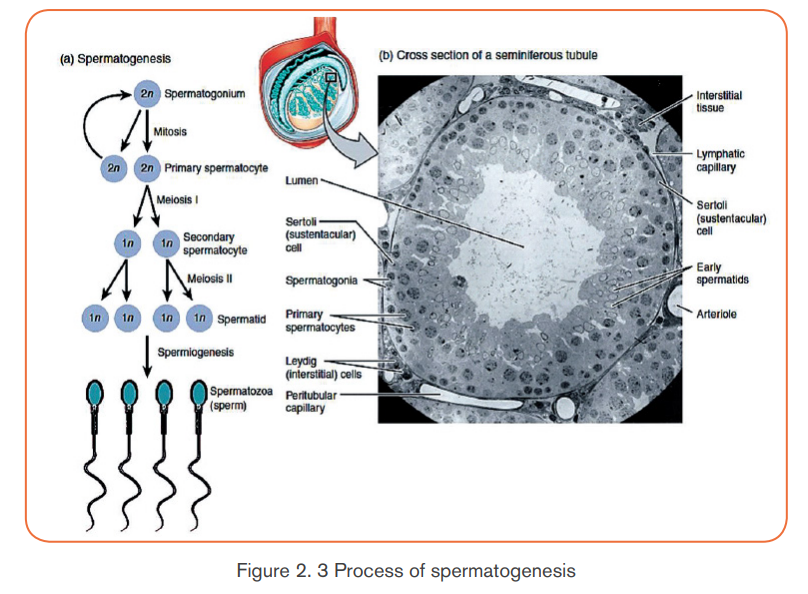
A) Spermatogenesis
The process of formation of haploid male gametes or spermatozoa from diploid
reproductive cells in males is called spermatogenesis. The complete process is
broadly divided into two parts, formation of spermatids and spermatogenesisor spermatoleosis.
Formation of Spermatids
The process of formation of spermatids is further divided into three stages as:
a) Multiplication phase: The primordial germ cells or sperm mother cells
differentiate from germinal epithelium of testis and increase in size with
prominent nuclei. These cells divide repeatedly by mitosis (i.e., equational
division) and produce a number of diploid daughter cells, known as
spermatogonia. Thus, in this stage, multiplication of germ cells takes place
mitotically.
b) Growth phase: In this phase, spermatogonia increase in size by
accumulating food reserves and are now called primary spermatocytes.
c) Maturation phase: The primary spermatocytes (which are diploid)
undergo first maturation division which is meiotic division (or
reductional division) to produce two haploid secondary spermatocytes.
These haploid secondary spermatocytes divide further by mitosis to give
rise to four haploid spermatids. This mitotic division is called secondmaturation division.
The spermatids so produced are non-motile rounded structures that
metamorphose into functional and motile spermatozoa through a process
known as spermiogenesis or spermatoleosis. The spermatozoa from testis
are incapable of fertilizing an ovum. They undergo several morphological,
physiological and biochemical changes as they move through the epididymis
to attain this structural and physiological maturity. The epididymis i) provides a
favorable environment to spermatozoa in acquiring fertilizing ability and ii) stores
them until they are ejaculated or move down to the vas deferens.
The morphological changes include structural remodeling of acrosome and
formation of disulfide linkages. The physiological and biochemical changes
include increase in net negative charge on spermatozoa, change in pattern of
motility, change in content of sialic acid, increase in specific activity and reflectionpower, resistance to pH and temperature and changes in metabolic patterns.
– Spermiogenesis
A series of changes in spermiogenesis that transform a non-motile spermatid
into motile, functional spermatozoa are listed below:- The nucleus shrinks and flattens by losing water. Only DNA is left in the
nucleus, making cells very light that aids to its motility.
- The two centrioles of a centrosome form proximal and distal centrioles
that lie at the posterior end of nucleus and give rise to axial filament of the
flagellum and acts as a basal granule respectively.- The mitochondria gather around axial filament and gradually unite toDuring all these steps, head of the developing sperm remains embedded in
form spiral sheath or nebenkern. It acts as power house of the sperm and
provides energy.
- The golgi bodies form the covering over nucleus called acrosome. During
acrosome formation, one or more vacuoles start enlarging with a small,
dense body called pro-acrosomal granule which further enlarges to
form acrosomal granule. The vacuole loses its liquid content and forms the
cap of spermatozoan. The remaining part of golgi apparatus is reduced
and discarded from sperm.
sertoli cells for nourishment. At the end, fully formed spermatozoan showsdistinct head, middle piece and tail region.
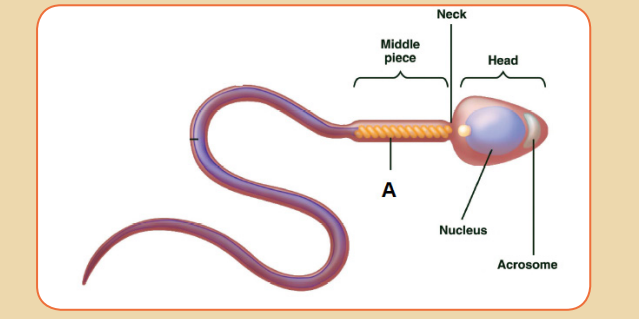
Structure of Spermatozoa
The sperms are microscopic and motile cell. Each sperm is composed of four
parts a head, a neck, a middle piece and a tail. A plasma membrane covers the
whole body of sperm.
i) Head is the enlarged end of the sperm, containing an elongated haploid
nucleus. The anterior of the nucleus is covered by a cap-like structure called
acrosome. The acrosome contains enzymes sperm or hyaluronidases,
which are used to contact and penetrate the ovum at the time offertilization.
ii) Neck is very short and is present between the head and middle piece. It
contains the proximal centriole towards the nucleus which plays a role in
the first cleavage of the zygote and the distal centriole which gives rise tothe axial filament of the sperm.
iii) Middle piece possesses numerous mitochondria which produce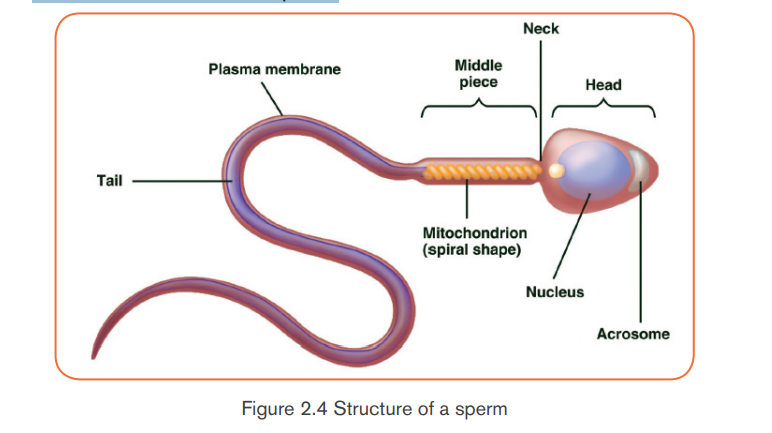
energy for the movement of the sperm. At the end of the middle
piece, there is a ring centriole (annulus) with unknown function.
iv) Tail is several times longer than the head. It consists of an axial filament
surrounded by a thin layer of cytoplasm. The tail provides motility tothe sperm, which is essential for fertilization.
b) Growth and differentiation phase: During this long phase, which may
last upto years, one cell in a follicle prepares for the formation of ovum. It
starts meiotic division but gets arrested at prophase-I stage and is called
primary oocyte. The remaining cells of the follicle lose the potential to
become primary oocyte and are known as the follicular cells or granulosa
cells. These follicular cells serve to protect and nourish the primary oocyte.
The complete follicle with a primary oocyte surrounded by a layer of
follicular cells is called the primary or the ovarian follicle.
c) Maturation phase: At puberty, only one of the primary oocytes resumes
division per menstrual cycle, alternately in each ovary. The tertiary follicle
matures into a Graafian follicle, within which the primary oocyte makes two
successive to form secondary oocyte. However, the secondary oocyte
again gets arrested at metaphase stage of meiosis-II and is released
from the ovary during ovulation. It waits in the oviduct for the sperm to
arrive. If fertilization occurs, sperm entry into the secondary oocyte marks
the resumption of meiosis. The 2nd maturation division (meiosis-II) again
divides the secondary oocyte into two unequal daughter cells: a large
ootid and a very small 2nd polar body. The ootid undergoes maturation into
a functional haploid ovum. A thin vitelline membrane develops outside theplasma membrane of the ovum that protects and nourishes the latter.
– Structure of Ovum
An ovum is a spherical, non-motile cell, in the secondary oocyte stage of
oogenesis. Human ovum is microlecithal with large amount of cytoplasm.
Cytoplasm is differentiated into outer, smaller and transparent exoplasm or egg
cortex and inner, larger and opaque endoplasm or ooplasm. Egg cortex is with
some cytoskeletal structures like microtubules and microfilaments, pigment
granules and cortical granules of mucopolysaccharides. Endoplasm is with cellorganelles,
informosomes, tRNAs, histones, enzymes etc.
The ovum is covered over by a thin, transparent vitelline membrane which is
further covered over by zona pellucida. There is a narrow space between these
two membranes known as perivitelline space. During discharge of ovum from
the Graafian follicle, several layers of follicular cells adhere to the outer surfaceof zona pellucida and are arranged radially forming corona radiata.
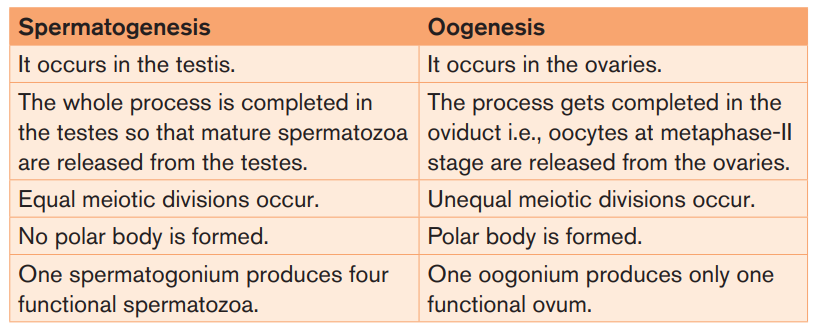
Table 2.3: Differences between spermatogenesis and oogenesis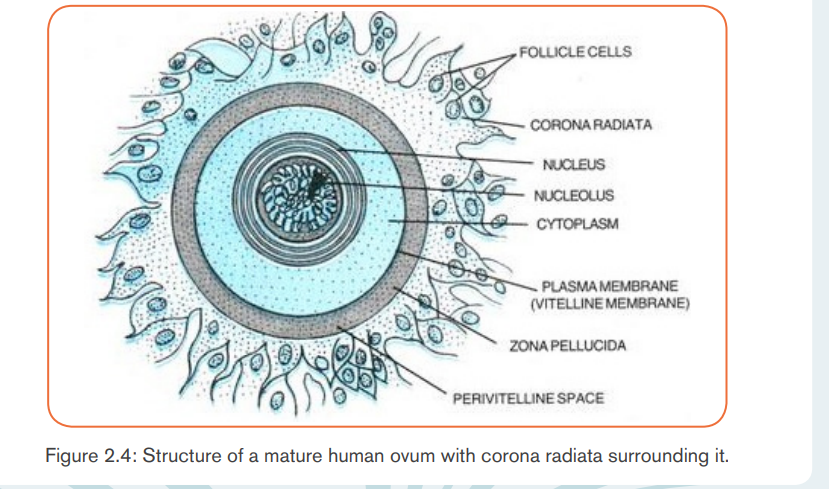
Application activity 2.2
1. Suppose that four hundred sperm mother cells have undergone a process
of spermatogenesis in a testis of human. How many chromosomes are
produced at the end of spermatogenesis? How many chromosomes
does each sperm have?
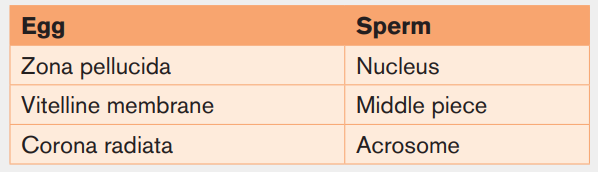
2. On the basis of your observations, use the drawn structure of a human
spermatozoan and an ovum and label their respective parts along with
the functions of each: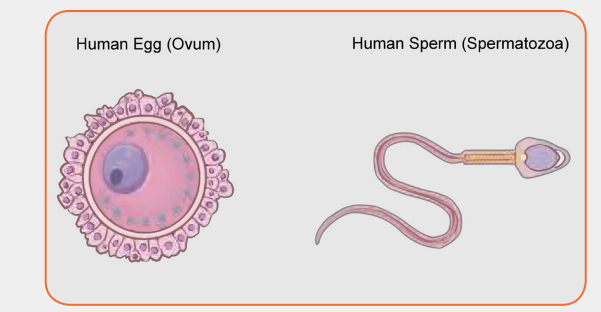
2.1.4. Cycle in humans
Activity 2.3
Human beings grow and develop from childhood to adulthood, during such
period of growth and development; there are changes in some parts of body
which may occur physiologically, physically and even psychologically. These
changes prepare individual adulthood to reproduce. Different researchers
indicated these changes to be coordinated by different types of hormones.1. Suggest the hormones involved during such period of changes in body
parts?
2. Discuss the significance of these hormones you have mentioned above
during such period of changes.
3. Describe the role of hormones involved during pregnancy and birth.4. Which day of the cycle will ovulation take place?
The menstrual cycle refers to the periodical changes in the reproductive behaviour
of a female which tend to occur in a sequence of events one after the other
in the periodical circle. At the onset of puberty, the cycle begins and repeats
after 28 days unless interrupted by pregnancy. The changes are stimulated
by the gonadotrophic hormone such as; follicle stimulating hormone (FSH)
and luteinizing hormone (LH). These hormones stimulate ovaries to secrete;
oestrogen (steroid) and progesterone hormones. These four hormones are
involved in menstrual cycle. Two of them including; FSH and LH are produced
by pituitary gland and the other two are released by ovaries respectively. The
most obvious sign of the cycle is the monthly discharge of blood a process
called menstruation. The first day of menstruation is regarded as the first dayof the cycle.
The three phases of the menstrual cycle are the follicular phase,ovulation and the luteal phase.
a. Follicular phase
Menstrual cycle usually begins when blood is first discharged from the uterus
during the first to fifth day (1-5 days). Following the reduction of progesterone,
the hypothalamus releases gonadotropin releasing hormone (GnRH) which
stimulates anterior pituitary gland to secrete follicle stimulating hormone (FSH).
FSH brings about the following effects:- Stimulates the development of a primary follicleCauses production of oestrogen by uterine cells. The oestrogen produced- Contributes to the shedding of uterine wall
promotes healing, repair and growth of uterine lining, inhibits further
secretion of FSH. Oestrogen levels keep on raising until day 13 where
they stimulate secretion of luteinizing hormone (LH) by anterior pituitarygland.
b. Ovulatory phase
Around the 14th day, the high levels of oestrogen causes release of luteinizing
hormone (LH).The release of LH brings about ovulation (release of mature egg
from the ovary). Immediately after and slightly before ovulation, a woman is fertile
and can conceive a baby if she has sexual intercourse or if sperm is present inher oviduct.
c. Luteal phase
After ovulation, the remains of ovarian follicle form corpus luteum also known
as Yellow body, which secrete large amounts of progesterone hormone
and smaller oestrogen. These two hormones; stimulate further development
of mammary glands, inhibit release of FSH and thickening wall of uterus in
anticipation of pregnancy. If oocyte (ovum) is not fertilized with in about 36
hours of being shed into oviduct, it dies and corpus luteum gets smaller. Thus
levels of progesterone and oestrogen keep on reducing until day 28 days i.e. 14
days after ovulation. Low levels of progesterone remove the inhibitory effect onFSH, causing its release thus menstruation and the cycle starts again.
The menstrual cycle is the regular natural changes that occurs in the female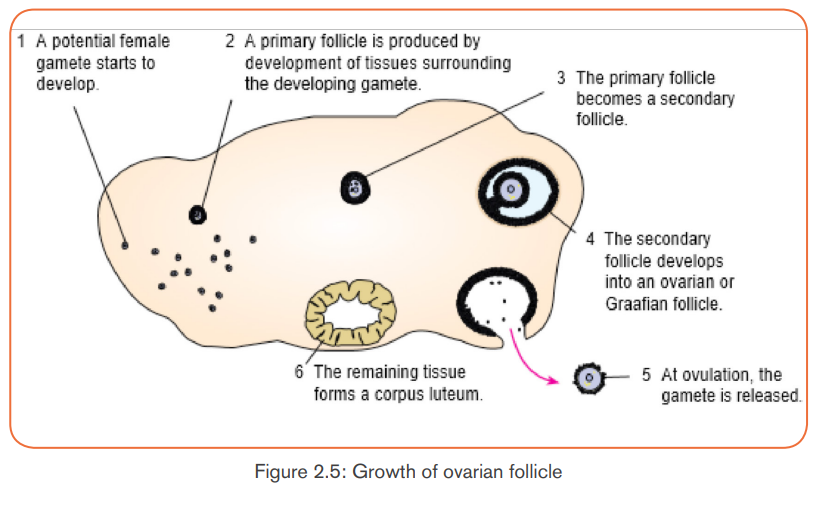
reproductive system (specifically the uterus and ovaries) that makes pregnancy
possible. The cycle is required for the production of oocytes, and for the
preparation of the uterus for pregnancy. The uterine events during menstrualcycle can also be divided into three phases:
Menstrual phase: when endometrium tissue is discharged and vaginal bleeding
occurs at the end of ovulatory cycle if pregnancy has not occurred. It is called
menstruation. It describes the shedding of endometrium when implantation
does not occur. When pregnancy does not occur, the level of progesterone
falls and this leads to the shedding of endometrium. Menstrual bleeding lasts
between 3 and 5 days. The first day of the period is the first day of the cycle.
Proliferative phase: It stimulates the thickening of endometrium of the uterus.
This thickness of endometrium is stimulated by estrogen from follicles before
ovulation which occurs when the ovarian follicles rupture and release the
secondary oocyte ovarian cells. This results to the development of ovary. It acts
like follicular phase.
Secretory phase: it occurs after ovulation for describes further thickening of
endometrium (endometrium tissue become more complex) in preparation for
implantation. This is stimulated by progesterone which is secreted by corpus
luteum and this occurs when corpus luteum is functioning. It acts like lactealphase.
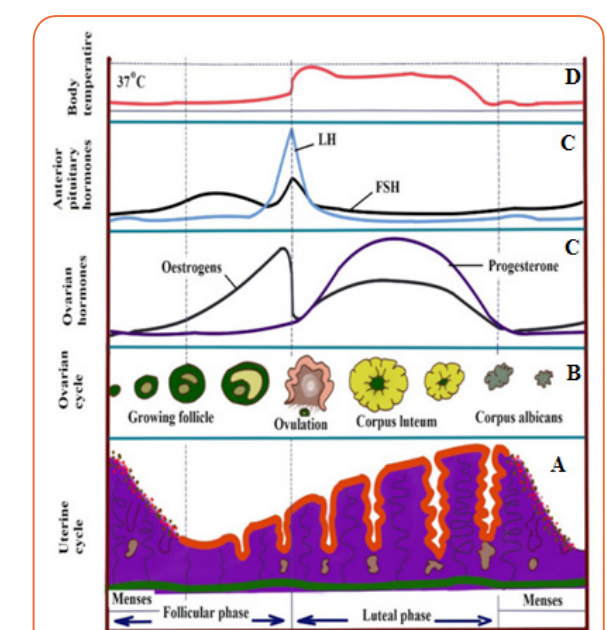
Figure 2.6: Menstrual cycle of human female
Application activity 2.3
1. The diagram below represents a section through a human ovary inovulation.
1. Use the diagram to locate the step at which ovulation take place. Explain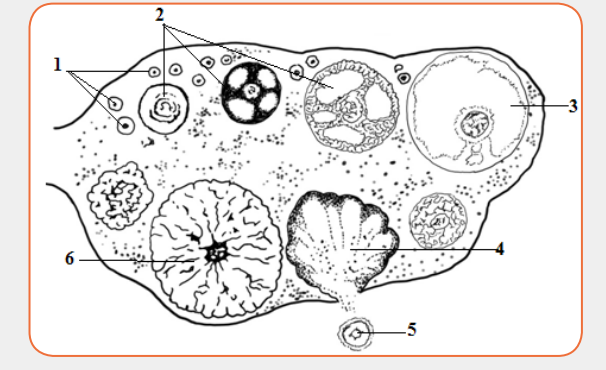
your answer.
2. State what will happen to this structure next if pregnancy has not
occurred.
3. State which hormone is needed to cause the changes seen in thediagram and indicated by the sequence (1), (2) and (3).
2.1.5. Fertilization and fatal developmentActivity 2.4
The following diagram represents different stages that happen before fetal
development. Use it to answer related questions.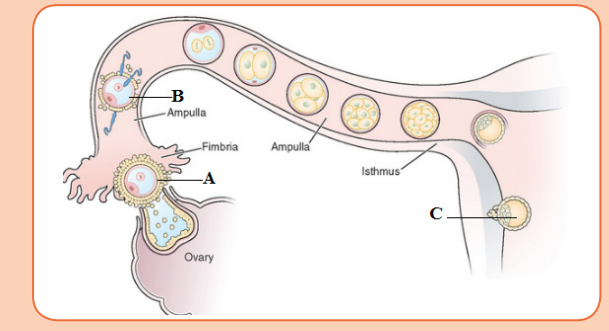 i) Suggest the name of the cell labeled A.a. Copulation
i) Suggest the name of the cell labeled A.a. Copulation
ii) Name the process which is happening on the cell labeled B. What
are the conditions required for the process to happen? Justify your
answer.
iii) Describe the process which is happening in C and what happensafter?
It is act of mating where sperms from male are transferred into the female tract.
Male mammals have an intromittent organ called penis which becomes erect
at a moment of mating for insertion into female’s vagina. The erection of penis is
brought by hydraulic action (penis becomes gorged with blood). This occurs as
a result of sexual arousal which brings about by ejaculation (release of sperm).
The semen’s are secreted from accessory glands into vas deferens and bladder
sphincter closes preventing urine from entering urethra. Sperms are expelled
from epididymis into vas deferens and out of the body by a series of muscle
contraction of penis. In a female, sexual arousal results in the swelling of clitoris
and stimulates the secretion of mucus which lubricates vagina during sexualintercourse.
b. Fertilization
Fertilization is the fusion of male and female nuclei to form zygote. Copulation
results in the ejection of spermatozoa into vagina. The spermatozoa swim in the
watery mucus of vagina and uterus up into the oviduct where the fertilization
takes place in the upper part of the oviduct. From the vagina or uterus
spermatozoa propel using energy from mitochondria. If ovulation has already
taken place, the egg and sperm meet in the upper part of oviduct and once they
come into contact, acrosome raptures and release lytic enzyme which dissolve
corona radiata of the egg and soften zona pellucida and vitelline membrane. The
following processes take place:
– Capacitation
This is a stage where by sperm undergoes essential changes while passing
through female genital track and this takes about 7 hours. These changes
include the removal of a layer of glycoprotein from outer surface of sperm, by
enzyme in uterus. Cholesterol also is removed to weaken the membrane.
– Acrosome reaction
This involves the releasing of enzyme found in acrosome such as hyaluronidases
and protease. These enzymes digest corona radiata (narrow path in the follicle
cells) and the zona pellucida (a protective glycoprotein surrounding the plasmamembrane of the egg).
Fusion
In this stage the head of sperm will fuse with the microvilli surrounding thesecondary oocyte and penetrate its cytoplasm.
– Cortical reaction
This stage involves the releasing of enzymes by lysosomes in cortical granules
(outer region of the secondary oocytes); the enzymes cause the zona pellucida
to thicken and harden forming a fertilization membrane. This cortical reaction
prevents the entry of other sperm inside ovum (polyspermy).
– Zygote formation
The secondary oocyte is stimulated to complete meiosis II, during this time of
stimulation the nucleus of sperm and secondary oocyte are called pro-nucleiand then the two nuclei fuse to form the zygote (2n).
2.1.6. Embryonic development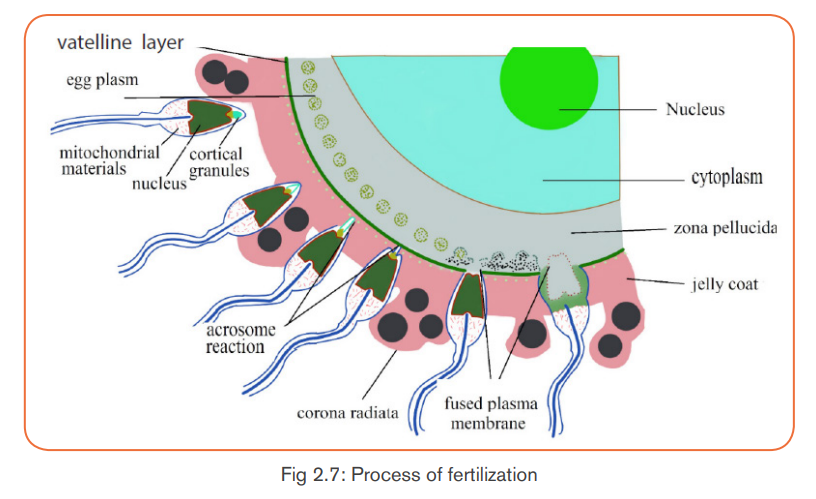
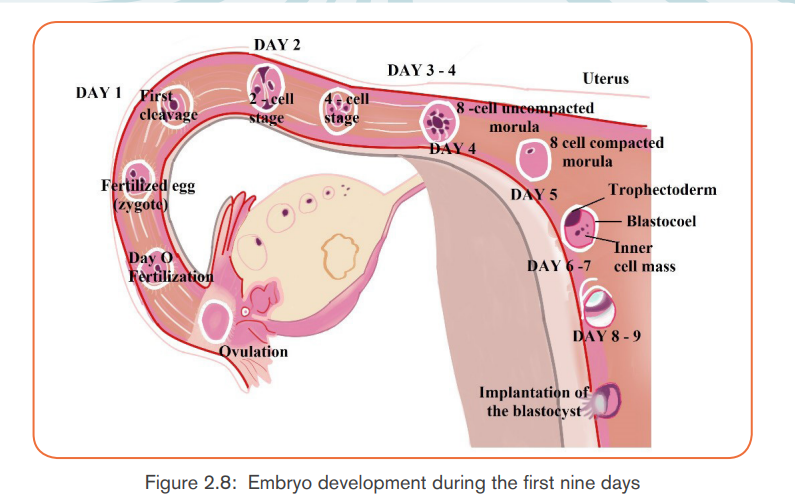
The zygote spends the next few days travelling down the oviduct (Fallopian
tube) by peristaltic contraction and by beatings of the cilia in wall of the oviduct
toward the uterus. As it travels, it divides by mitosis several times to form a ball
of cells called a morula. The cell divisions, which are called cleavage, increase
the number of cells but not their overall size. More cell divisions occur, and soon
a fluid-filled cavity forms inside the ball of cells. At this stage, the ball of cells iscalled a blastocyst.
The blastocyst reaches the uterus and becomes embedded in the endometriumat roughly the 5th – 10th day. Once in the uterus, the blastocyst burrows into theuterine wall a process called implantation. After implantation, the blastocyst
becomes embryo. It grows through multiplication and differentiation of its cells
forming tissues and organs. The heart and blood vessels are the first organsformed and embryo now called foetus.
During embryonic development, cells of the embryo migrate to form three distinct
cell layers: the ectoderm, mesoderm, and endoderm. Each layer will eventually
develop into certain types of tissues and cells in the body of vertebrates.- Ectoderm: forms tissues that cover the outer body; develops into cells
such as nerves skin, hair, and nails.
- Mesoderm: forms tissues that provide movement and support; develops
into cells such as muscles, bones, teeth, and blood.
- Endoderm: forms tissues involved in digestion and breathing; developinto organs such as lungs, liver, pancreas, and gall bladder.
Application activity 2.4
The diagram below shows some of the events which take place in the ovaryand oviduct (Fallopian tube) around the time of fertilization.
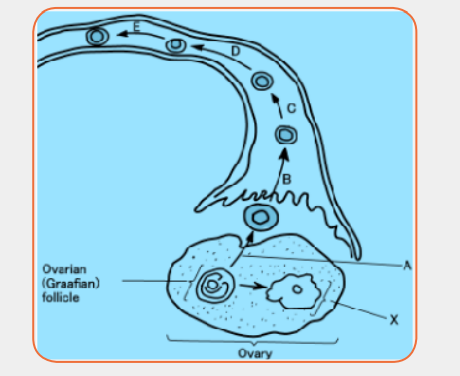
a) Name the following:
i) The process labeled A.b) On the diagram, use the letter F to label the region where fertilization
ii) The type of nuclear division taking place at D and E.
iii) The structure labeled X.
iv) One hormone produced by structure X.took place
2.1.7. Role of placenta in the development of an embryoActivity 2.5
The drawing below shows a developing human fetus inside the uterus.Observe the diagram and attempt the related questions.
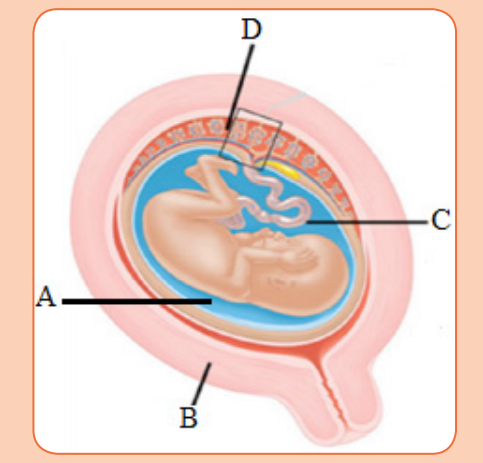 a) Suggest the name of the parts marked A to D.The placenta is a temporary organ in which nutrients and wastes are exchanged
a) Suggest the name of the parts marked A to D.The placenta is a temporary organ in which nutrients and wastes are exchanged
b) Which part is involved in transport of substance from mother to fetus
on the diagram and why?
c) Suggest four substances which pass from the mother to the embryo.
d) Name one substance which passes from the embryo to the mother.e) What is the importance of the placenta?
between the mother and the embryo or foetus.
The foetal part of the placenta consists of the allantoids and chorion. The
chorion forms many large projections called chorionic villi which contain a
dense network of foetal capillaries which in turn are connected to two umbilical
arteries and umbilical vein in the umbilical cord. The umbilical arteries carry
blood from the foetus to the placenta, while the umbilical vein carries blood
in the opposite direction. Although maternal blood in the endometrium is in
close proximity with the foetal blood in the umbilical capillaries, they do not mixbecause they separated by membranes of the villi and capillary.
The placenta is an organ that develops in your uterus during pregnancy with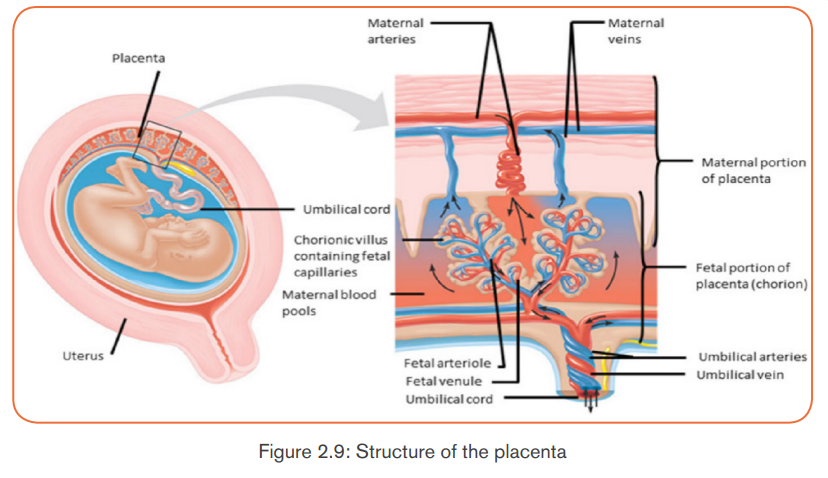
specifically the following functions:- It allows diffusion of nutrients such as water, glucose, amino acids, simpleNote: The action of HCG is similar to that of LH. HCG stimulates the corpus
proteins and mineral salts from maternal blood.
- It is a site of gaseous exchange: haemoglobin of the foetus has high affinity
to oxygen compared to adult haemoglobin.
- It offers passive natural immunity on the foetus. Certain maternal antibodies
can cross the placental barrier.
- It protects foetal circulation from the high pressure in the maternal
circulation
- Prevents mixing of maternal and foetal blood which would cause
agglutination (clotting) if the two blood types are incompatible.
- It produces and secretes hormones such as the HCG (human chorionicgonadotrophin), progesterone, oestrogen, and relaxin.
luteum to secrete progesterone and oestrogen throughout the first trimester.
HCG is produced in such large quantities that some of it is excreted in the urine
of a pregnant woman (positive test of pregnancy). Secretion of HCG declinesaround tenth week and the corpus luteum reduces.
The placenta does not give complete protection to the foetus. Certain pathogens,
toxins, and drugs can enter the foetal circulation and cause damage. Examplesare; HIV, rubella toxins, alcohol, nicotine and heroin.
Application activity 2.5
The diagram shows the structure of the placenta and parts of the fetal andmaternal circulatory systems.
a) Complete the table by listing the blood vessels that carry oxygenated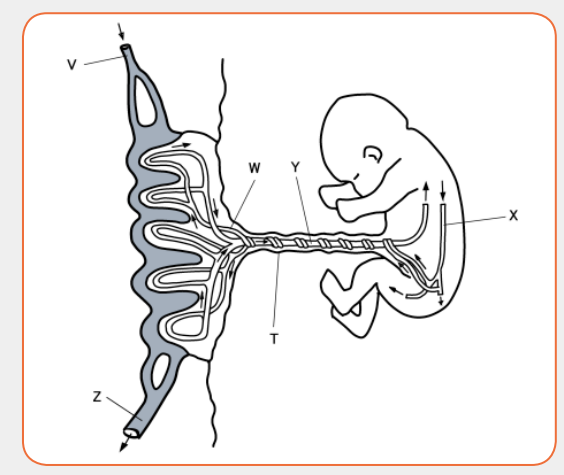
blood. Use the letters in the diagram to identify the blood vessels.
b) What happens on the structure T after birth?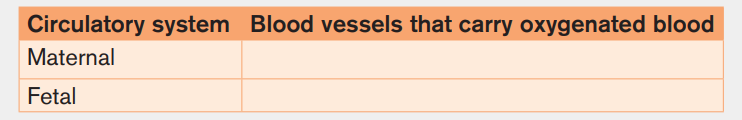
c) The placenta is adapted for the exchange of substances between the
maternal blood and the fetal blood. Describe the exchanges that occuracross the placenta to keep the fetus alive and well.
2.1.8. Physiological changes in females during pregnancy
and Parental care
Activity 2.6Observe the following images that show pregnant women.
Use your personal observation or conduct research from medical personnel,
internet or library to answer the following questions:a) Suggest the physical changes that can be observed to the pregnantPregnancy refers to the development that take place between fertilization of the
women.
b) What physiological and behavioral changes that can happen when
women get pregnant.
c) It is necessary to practice a special parental care to pregnant women.Provide reasons that justify this statement.
ovum to birth of the foetus. When fertilized egg becomes implanted in uterine
wall, pregnancy starts. And a number of important events take place during
this period. The period from fertilization to birth is called gestation period. Inhuman it is about nine months.
A. Changes during pregnancy
A pregnant woman’s body undergoes various; physiological, physical and
behavioural changes.
a) Physiological changes during pregnancy- Respiration rate rises for increased maternal oxygen consumption which is
needed for demand of placenta, uterus and foetus.
- More blood vessels grow and pressure of expanding uterus on large veins
causes blood to slow in its return to the heart.
- Rise up and out of pelvic cavity this action displaces the stomach and
intestine.
- Blood volume increase greatly.- Placenta produces large amount of progesterone and oestrogen by 10 to12 week of pregnancy to control uterine activity.
- Increased requirement of calcium due to increase of parathyroid gland.b) Physical changes during pregnancy
- Experiences warm (hot flashes) caused by basal metabolic rate and
increased hormonal level.
- Stretching of abdomen wall and ligaments that support uterus.
- Kidney work extra hard to excrete waste products of both mother andfoetus.
- Breast may become large and more tender because of increased level ofc) Behavioural changes during pregnancy
oestrogen hormone progesterone thus breast gets even bigger to prepare
for breast feeding.
- Nipples may stick out more.
- By the end of third trimester, a yellow, watery, pre-milk may leak from
nipples.
- Changes in hair and nail growth and texture due to hormone changes.
- Leg cramp caused by fatigue from carrying pregnant weight.
- Feet and ankles may swell because of extra fluid in the body duringpregnancy.
- Physical discomfort such as urinary frequency can be frustrating.B. Delivery process
- Fear and anxiety lessen especially when foetal movements are felt.
- Self-introspection
- Nesting behaviour begins. Some woman exhibits mood swings andemotional liability.
By the end of pregnancy, near the time of birth, the amniotic sac raptures
(breaks) and amniotic fluid drains through birth canal and labour usually begins
which involves the contractions of muscular walls of the uterus.
Initiation of birth: Uterine contractions start when the foetal pituitary gland
secretes adrenocorticotrophic hormone (ACTH) which stimulates foetal adrenal
gland to secrete corticosteroids. These hormones pass into blood sinuses in
placenta to cause maternal cells to secrete prostaglandins (local hormone) and
cause uterine wall to contract. This contraction pushes the foetal head against
the cervix to stimulating stretcher receptor to send information to mother’s
brain and causes release of oxytocin hormone. The prostaglandin and oxytocin
hormone together result intense contraction of uterine walls called labour
which stimulates more release of oxytocin hormone and as positive feedbackmechanism.
The delivery process can be summarized into three main stages:- Dilation stage: During this stage, water sac filled with amniotic fluid forms
and precedes the head, widening soft tissue of birth canal, cervix, and
vagina for canal of constant diameter. The amnion raptures and amniotic
fluid drains through vagina.
- The expulsion stage: During this stage, cervix is fully dilated while
abdominal muscle bear down in supporting rhythmic contraction of uterus
shorten the uterine wall and baby is pushed into and through the birth
canal. The head and shoulder align themselves first.
- Placenta stage: This stage begins with complete expulsion of baby and
ends with expulsion of foetal membrane. The cord is clamped and cut
when delivery of baby is complete. This leads carbon dioxide enrichment
into baby’s blood which activates respiratory centre and baby begins to
breath with the first cry at the same time foetal circulation changes tobaby’s own systemic and pulmonary circulation.

Antenatal care is the care you get from health professionals during your
pregnancy. It is sometimes called pregnancy care or maternity care. Prenatal
care, also known as antenatal care, is a type of preventive healthcare. Its goal
is to provide regular check-ups that allow doctors or midwives to treat and
prevent potential health problems throughout the course of the pregnancy andto promote healthy lifestyles that benefit both mother and child.
a) Health needs of the pregnant mother
The pregnant mother needs to maintain good health status so that she has a
healthy baby. To remain healthy she needs:- To avoid contractions diseases such as malaria, STIs and HIV and AIDS
as these may harm the foetus.- To avoid smoking and drinking alcohol as these interfere with growth anddevelopment of the foetus, especially brain development.
- To eat an adequate balanced diet so that she maintains her good health
and is able to give birth to a healthy baby. Malnourished mothers usually
give birth to babies who are underweight. Such babies often have growth
and development problems because they do not eat well and tend to get
sick often.During the antenatal period, the promotion of the women healthy is the care
- To attend the ante-natal clinic once a moth so that her health and nutritional
needs and those of the foetus are monitored. In the ante-natal clinic the
mother has her weight monitored, blood pressure checked and urinechecked to establish the level of sugar.
and health of their babies before and after birth. Educating mothers about the
benefits of good nutrition, adequate rest, good hygiene, family planning and
exclusive breastfeeding, immunization and other disease prevention measures
aims to develop women’s knowledge of these issues so they can make better
decisions affecting their pregnancy outcome and never forget the difficultiessome women will face in being able to improve their lifestyles.
b) Nutritional needs of the pregnant mother
The pregnant mother needs additional nutritional requirements to meet the needs
of the growing foetus and those of her body. The pregnant mother therefore
needs to eat additional balanced diet to cater for these additional nutritional
requirements in her own body and for that of the growing foetus. The mother
needs the increased nutrients because of:- The increase in the rate at which her body burns energy. More carbohydrates
and fats are required. Adequate amounts of carbohydrates and fats are
required for the additional weight the mother puts on. The mother puts on
additional weight of about 10 to 12.5kg during pregnancy. More energy
giving foods are required to make up this additional weight.
- The increase in her blood volume of her additional weight. More iron is
required to form additional blood required by the body.
- The development of the placenta which requires nutrients to form and
making the amniotic fluid within which the foetus grows require more
nutrients.
- Increased muscles for both the mother and the growing foetus. The
mother’s body requires additional muscles, especially the breast and
uterine tissues. More proteins are required to develop these muscles.
- The need to store more fat. This fat is stored during the first four months
of pregnancy. From 5-9 months the stored nutrients are used by the fast
growing foetus. The mother starts to appear thinner.The breast milk contains antibodies that help your baby fight of viruses and- Preparation of breast-feeding. Nutrients are required to prepare milk to be
used to breast-feed the baby.
bacteria. Breastfeeding lowers your baby’s risk of having asthma or allergies.
Plus, babies who are breastfed exclusively for the first 6 months, without any
formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea.
In humans breastfeeding is associated with many other benefits:- It makes earlier a closer contact between the mother and her infantApplication activity 2.6
- The infant has a better control over its own milk intake, this prevents over
eating in late life
- Fats and irons from breast milk are better absorbed than those in cow’s
milk and milk is easily digested.
- Breast feeding provides important antibodies that help to prevent
respiratory infections and meningitis,
- Breastfeeding helps the mother’s reproduction organ return to a normal
state more rapidly
- Breast feeding promotes the secretion of LH (and prolactin) and this
makes a delay in follicle development and ovulation,
- The act of sucking on the breasts, promotes the development of the jaw,facial muscles and teeth (sucking from a bottle requires less effort).
1. Copy and complete the table to show, for each hormone, the precise
site of its secretion, and its effects on the ovary or on the endometriumof the uterus.
Alcohol consumption for pregnant women is generally more dangerous on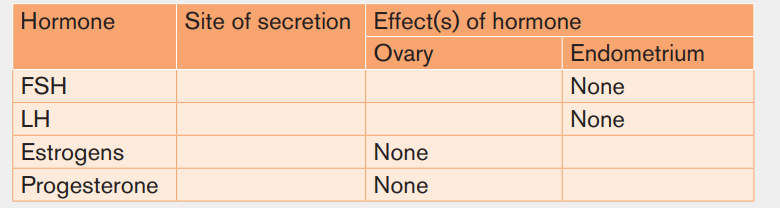
an embryo than a fetus. Suggest the reasons.
2.2. Family planning and contraceptive methods
Activity 2.7The photos below show various contraceptive methods.
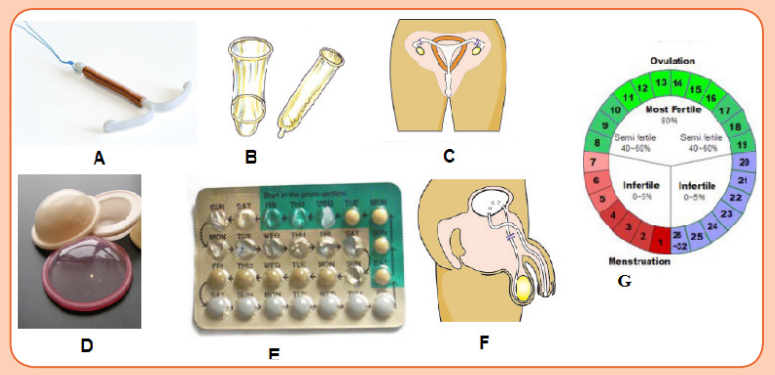 a) Use the photos to identify the letters that represent natural and artificialContraception is the prevention of conception that is preventing the fusion of
a) Use the photos to identify the letters that represent natural and artificialContraception is the prevention of conception that is preventing the fusion of
contraceptive methods. Justify your choice.
b) The most effective contraceptive method for young people is the useof condom. Provide the reasons for this statement.
the male gamete with the female gamete. Both natural and artificial methodsexist.
2.2.1 Natural contraceptive methods
Natural birth control methods include specific actions that people can do
naturally to help prevent an unintended pregnancy. Instead, these methods to
prevent pregnancy require that a man and woman not have sexual intercourse
during the time when an egg is available to be fertilized by a sperm.
The fertility awareness methods are based upon knowing when a woman
ovulates each month. In order to use a fertility awareness method, it is necessary
to watch for the signs and symptoms that indicate if ovulation has occurred oris about to occur.
i) Calendar rhythm method
The calendar rhythm method to avoid pregnancy relies upon calculating a
woman’s fertile period on the calendar. Based upon her 12 previous menstrual
cycles, a woman subtracts l8 days from her shortest menstrual cycle to determine
her first fertile day, and 11 days from her longest menstrual cycle to determine
her last fertile day. She can then calculate the total number of days during which
she may ovulate. If a woman’s menstrual cycles are quite irregular from month to
month, there will be a greater number of days during which she might become
pregnant.
The calendar method is only about 80% effective in preventing pregnancy and
when used alone, it is considered outdated and ineffective.
ii) Basal body temperature method
The basal body temperature (BBT) method is based upon the fact that a
woman’s temperature drops 12 to 24 hours before an egg is released from her
ovary and then increases again once the egg has been released. Unfortunately,
this temperature difference is not very large. It is less than 1-degree F (about ahalf degree C) when the body is at rest.
The basal body temperature method requires that a woman take her temperature
every morning before she gets out of bed. A special thermometer that is more
accurate and sensitive than a typical oral thermometer must be used, and the daily
temperature variations carefully noted. This must be done every month. Onlinecalculators are available to help a woman chart her basal body temperature.
To use the basal body temperature as a birth control method, a woman should
refrain from having sexual intercourse from the time her temperature drops untilat least 48 to72 hours after her temperature increases again.
iii) Mucus inspection method
The mucus inspection method depends on the presence or absence of a
particular type of cervical mucus that a woman produces in response to
estrogen. A woman will generate larger amounts of more watery mucus than
usual (like raw egg white) just before release of an egg from her ovary.This socalled egg-white cervical mucus stretches for up to an inch when pulled apart.
A woman can learn to recognize differences in the quantity and quality of her
cervical mucus by examining its appearance on her underwear, pads, and toilet
tissue; or she may gently remove a sample of mucus from the vaginal opening
using two fingers. She may choose to have intercourse between the time of her
last menstrual period and the time of change in the cervical mucus. During this
period, it is recommended that she have sexual intercourse only every other day
because the presence of seminal fluid makes it more difficult to determine the
nature of her cervical mucus. If the woman does not wish to become pregnant,
she should not have sexual intercourse at all for 3 to 4 days after she notices thechange in her cervical mucus.
iv) Withdrawal method
Withdrawal is a behavioral action where a man pulls his penis out of the vagina
before he ejaculates. The withdrawal method also relies on complete selfcontrol.
You must have an exact sense of timing to withdraw your penis in time.
Because this can be difficult for the man to complete successfully, the withdrawalmethod is only about 75%-80% effective in preventing pregnancy.
v) Abstinence
Abstinence from sexual activity means not having any sexual intercourse at all.
No sexual intercourse with a member of the opposite sex means that there is nochance that a man’s sperm can fertilize a woman’s egg.
vi) Lactation amenorrhea method
Lactation Amenorrhea method can postpone ovulation for up to 6 months after
giving birth. This natural birth control method works because the hormone
required to stimulate milk production prevents the release of the hormone that
triggers ovulation. This method is highly effective for the first six months after
childbirth. The mother has to breastfeed the baby at least every four hours
during the day and every six hours through the night. She also has to be aware
of her menstrual period. After six months fertility may return at any time.
Advantages of natural birth control- A woman does not need to take medication or use hormonal manipulation.Disadvantages of natural birth control include
- No procedures or fittings by a physician are required.- It can be difficult to estimate or know precisely when a woman is fertile,2.2.2. Artificial contraceptive methods
allowing increased chances for unplanned conception.
- Natural methods are not as effective as some forms of contraception.
- Ovulation test kits are used by some couples using natural methods of
contraception, and the cost of these kits is another potential disadvantage.
- Being unable to have intercourse at certain times of the month is a
disadvantage for some women.
Artificial contraception also known as birth control are medication used to
prevent pregnancy.
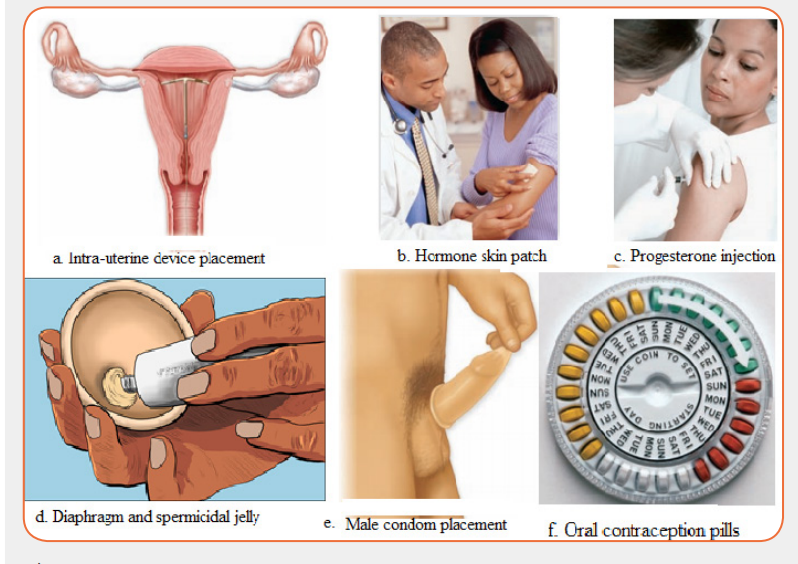
Oral Contraceptive pills: a chemical method of contraception. One version
uses a combination of progesterone and oestrogen that inhibits ovulation.Others are single hormones that require very careful management when taken.
Intrauterine device (IUD) the coil is placed inside the uterus an exact
understanding how this works is unclear. A possible explanation is that it
‘irritates’ the endometrium such that rejects implantation of embryos. The device
is made from plastic or copper and inserted by a doctor. Nevertheless, this
device is very effective.
Condom is another mechanical method of contraception that prevents the
sperm from reaching the egg. Composed of a thin barrier of latex this is placed
over the erect penis and captures semen on ejaculation. This is also a goodbarrier to prevent the transmission of sexual diseases.
Cap (diaphragm) is another barrier method again made from latex. The cap is
placed over the cervix to prevent the entry of sperm in semen. This technique
requires that the cap is put in position in advance of sexual intercourse and that
it is used in combination with a spermicidal cream. When used correctly this is
an effective contraceptive however this is not a barrier against the transmissionof sexual diseases.
Sterilization is a surgical and near permanent solution for contraception such
as: Vasectomy. In men this involves cutting the vas deferens and prevents sperm
entering the semen. In this state, man still ejaculates normally and releases
semen however this does not contain sperm. Tubal ligation involves the cutting
of fallopian tube so that eggs cannot reach the uterus. In women the surgery cutsor ties the oviducts thus preventing sperm from reaching the egg in fertilisation.
Advantages and disadvantages of birth control
Advantages of birth control/contraceptives- Gives great protection against unplanned pregnancy if one follows- Woman must begin using hormonal contraceptive in advance before they
instructions.
- Condoms to some extent protect against pregnancy and STDS.
- Combinations of pills reduce/prevent cysts in breasts and ovaries.
- Improved family wellbeing.- Improved maternal and infant health.
become effective.
- Some women experience several; headaches, breast tenderness, chest
pain, discharge from vagina, leg cramps and swelling or pain.
Disadvantages of birth control/contraceptives- Necessity of taking medication continually.Application activity 2.7
- High cost of medication.
- Hormonal contraceptive does not protect against STDS.
- Eggs may fail to mature in the ovary for a woman who uses hormonal
contraceptives.- Woman must remember to take them regularly.
1. Determining the fertile period
Count the number of days of your menstrual cycles and count the number of
days for 10 consecutive cycles. Choose the cycle with the highest number
of days and the cycle with the lowest number of days. Subtract 18 from the
lowest cycle and 11 from the highest cycle.
Example: Mary has 27 days as her shortest cycle and 36 as her longest
cycle. She has had her menstruation on 09/08/2019. What will be her fertile
period?2. The diagrams below represent different contraceptive methods.
 i) Use the diagrams to state contraceptive method that can prevent bothSkills Lab 2
i) Use the diagrams to state contraceptive method that can prevent bothSkills Lab 2
STDs and pregnancy. Justify your answer.
ii) Suppose you are married, which contraceptive method do you preferto use and why?
Pregnancy test
The HCG Card Pregnancy Test is a rapid chromatographic immune assay for
the qualitative detection of human chorionic gonadotropin in urine to aid in
the early detection of pregnancy. The test utilizes a combination of antibodies
including a monoclonal HCG antibody to selectively detect elevated levels of
HCG.
The pregnancy test works by checking the urine for a hormone called human
chorionic gonadotropin (HCG). The woman body only makes this hormone if
she pregnant. HCG is released when a fertilized egg attaches to the lining of
the uterus when pregnancy begins. If pregnancy test is positive, it means that
woman is pregnant. If the pregnancy test is negative, it means that woman isnot pregnant.
Procedure:- Carefully read the instruction included in your test kit before collecting
your urine sample.
- Remove the plastic cap to expose the absorbent window.
- Use collected first morning urine one to two weeks after the first missed
period.
- Collect urine in a cup and then dip the indicator stick into the cup to
measure the HCG hormone level.
- Hold an indicator stick directly in the urine stream until it is soaked,
which should take about five seconds.
- Remove the HCG card pregnancy and make observation.- Take conclusion of the observation following the indicated interpretation.
End Unit Assessment 2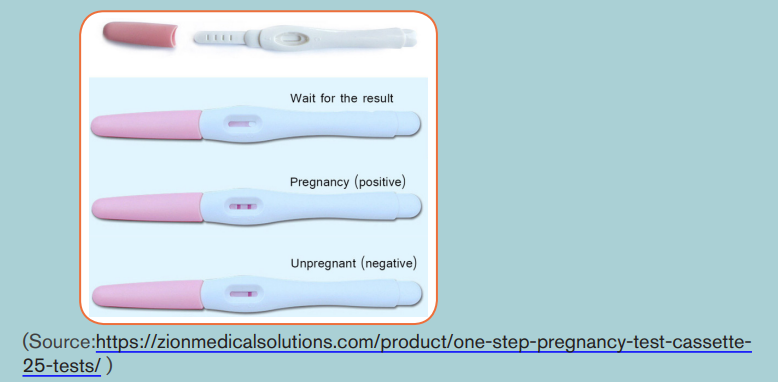
1. Which of the following do sperm NOT travel through?a) Ureter2. The placenta in humans is derived from the:
b) Urethra
c) Vas deferens
d) Epididymisa) Embryo only3. The graph below shows the level of reproductive hormones in the
b) Uterus only
c) Endometrium and embryo
d) None of the aboveblood of an un-named mammal during its reproductive cycle.
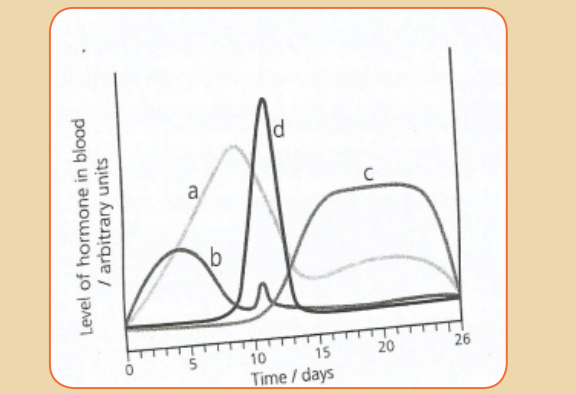 a) Name the hormones labelled (a) to (d)4. Answer the following questions:
a) Name the hormones labelled (a) to (d)4. Answer the following questions:
b) Give the likely day of the cycle on which ovulation takes place and
give reasons for your answer.a) Define the term fertilizationb) The diagram below shows the structure of a human sperm.
 i) Explain the part played by the organelle labelled A in the process5. Which contraceptive methods can protect against sexually transmitted
i) Explain the part played by the organelle labelled A in the process5. Which contraceptive methods can protect against sexually transmitted
leading to fertilization.
ii) The acrosome contains an enzyme that breaks down proteins.
Describe the function of this enzyme in the process leading to
fertilization.
diseases / infections?
6. The diagram shows the sequence of events in the development of a
mature ovarian (Graafian) follicle and corpus luteum
a) What is the main hormone produced by the ovary when stage B is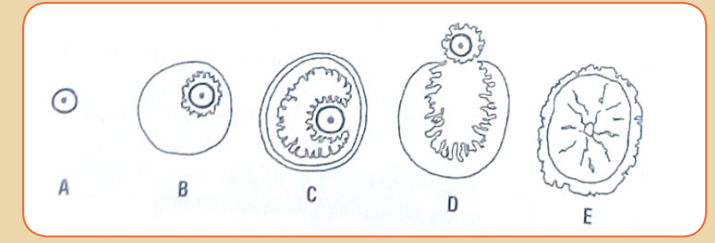
present?
b) Which two of stages A to E would you expect to find in the ovary of
a woman during the early stages of pregnancy?
c) Give the reason for your answer on b.
d) Some oral contraceptives contain only estrogens. Which of the
stages A to E would you expect to find in the ovary of a woman who
had been taking such an oral contraceptive for a prolonged period of
time?e) Give reasons for your answer on d.
